Evaluating Sensitivity and Specificity in Functional Assays: A Comprehensive Guide for Robust Research and Development
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for evaluating the sensitivity and specificity of functional assays.
Evaluating Sensitivity and Specificity in Functional Assays: A Comprehensive Guide for Robust Research and Development
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for evaluating the sensitivity and specificity of functional assays. It covers foundational principles, practical methodologies, advanced troubleshooting for optimization, and rigorous validation protocols. By integrating theoretical knowledge with actionable strategies, this guide aims to enhance the accuracy, reliability, and regulatory compliance of assays used in drug discovery, diagnostics, and clinical research.
Core Principles: Defining Sensitivity and Specificity in a Functional Context
Understanding Diagnostic vs. Analytical Sensitivity and Specificity
In the field of research and drug development, the terms "sensitivity" and "specificity" are fundamental metrics for evaluating assay performance. However, their meaning shifts significantly depending on whether they are used in an analytical or diagnostic context. This distinction is not merely semantic but represents a fundamental difference in what is being measured: the technical capability of an assay versus its real-world effectiveness in classifying samples. Analytical performance focuses on an assay's technical precision under controlled conditions, specifically its ability to detect minute quantities of an analyte (sensitivity) and to distinguish it from interfering substances (specificity) [1] [2]. In contrast, diagnostic performance evaluates the assay's accuracy in correctly identifying individuals with a given condition (sensitivity) and without it (specificity) within a target population [1] [3].
Confusing these terms can lead to significant errors in test interpretation, assay selection, and ultimately, decision-making in the drug development pipeline. A test with exquisite analytical sensitivity may be capable of detecting a single molecule of a target analyte, yet still perform poorly as a diagnostic tool if the target is not a definitive biomarker for the disease in question [1] [4]. Therefore, researchers and scientists must always qualify these terms with the appropriate adjectives—"analytical" or "diagnostic"—to ensure clear communication and accurate assessment of an assay's capabilities and limitations [2].
Conceptual Comparison: Analytical vs. Diagnostic
The core difference between analytical and diagnostic measures lies in their focus and application. The following table provides a concise comparison of these concepts:
| Feature | Analytical Sensitivity & Specificity | Diagnostic Sensitivity & Specificity |
|---|---|---|
| Primary Focus | Technical performance of the assay itself [1] | Accuracy in classifying a patient's condition [1] |
| Context | Controlled laboratory conditions [1] | Real-world clinical or preclinical population [1] [5] |
| What is Measured | Detection and discrimination of an analyte [2] | Identification of presence or absence of a disease/condition [3] |
| Key Question | "Can the assay reliably detect and measure the target?" | "Can the test correctly identify sick and healthy individuals?" [3] |
| Impact of Result | Affects accuracy and precision of quantitative data. | Directly impacts false positives/negatives and predictive value [6]. |
The Inverse Relationship and the Trade-Off
In the realm of diagnostic testing, sensitivity and specificity often exist in an inverse relationship [6]. Modifying a test's threshold to increase its sensitivity (catch all true positives) typically reduces its specificity (introduces more false positives), and vice versa [5] [3]. This trade-off is a critical consideration in both medical diagnostics and preclinical drug development.
In preclinical models, for example, this trade-off can be "dialed in" by setting a specific threshold on the model's quantitative output [5]. A model could be tuned for perfect sensitivity (flagging all toxic drugs) but at the cost of misclassifying many safe drugs as toxic (low specificity). Conversely, a model can be tuned for perfect specificity (never misclassifying a safe drug as toxic), which may slightly reduce its sensitivity [5]. The optimal balance depends on the context: for a serious disease with a good treatment, high sensitivity is prioritized to avoid missing cases; for a condition where a false positive leads to invasive follow-up, high specificity is key [3].
Quantitative Data and Experimental Comparison
The evaluation of analytical and diagnostic parameters requires distinct experimental approaches and yields different types of data. The following table summarizes the key performance indicators, their definitions, and how they are determined experimentally.
| Parameter | Definition | Typical Experimental Protocol & Data Output |
|---|---|---|
| Analytical Sensitivity (LoD) | The smallest amount of an analyte in a sample that can be accurately measured [1] [7]. | Protocol: Test multiple replicates (e.g., 20 measurements) of samples at different concentrations, including levels near the expected detection limit [7]. Output: A specific concentration (e.g., 0.1 ng/mL) representing the lowest reliably detectable level [7]. |
| Analytical Specificity | The ability of an assay to measure only the intended analyte without cross-reactivity or interference [1]. | Protocol: Conduct interference studies using specimens spiked with potentially cross-reacting analytes or interfering substances (e.g., medications, endogenous substances) [1] [7]. Output: A list of substances that do or do not cause cross-reactivity or interference, often reported as a percentage [1]. |
| Diagnostic Sensitivity | The proportion of individuals with a disease who are correctly identified as positive by the test [6] [3]. | Protocol: Perform the test on a cohort of subjects with confirmed disease (via a gold standard method) and calculate the proportion testing positive [8]. Output: A percentage (e.g., 99.2%) derived from: TP / (TP + FN) [8]. |
| Diagnostic Specificity | The proportion of individuals without a disease who are correctly identified as negative by the test [6] [3]. | Protocol: Perform the test on a cohort of healthy subjects (confirmed by gold standard) and calculate the proportion testing negative [8]. Output: A percentage (e.g., 83.1%) derived from: TN / (TN + FP) [8]. |
Experimental Protocols and Best Practices
Determining Analytical Sensitivity (Limit of Detection)
Establishing the Limit of Detection (LoD) for an assay is a rigorous process. A best practice approach involves:
- Replicate Testing: Perform a minimum of 20 independent measurements at, above, and below the suspected LoD [7]. This provides a robust statistical basis for the calculation.
- Appropriate Controls: For molecular assays involving nucleic acid extraction, a control must be included to monitor the efficiency of the extraction process itself. Using whole organisms (e.g., bacteria or viruses) as control material is recommended to challenge the entire workflow from extraction to detection [7].
- Data Analysis: The LoD is determined as the lowest concentration at which ≥95% of the replicates test positive, confirming consistent and reliable detection at that level.
Establishing Analytical Specificity
Evaluating analytical specificity involves testing the assay's resilience to interference and cross-reactivity.
- Interference Studies: Test specimens spiked with high concentrations of potential interfering agents against non-spiked specimens. Interferents can include endogenous substances (like lipids or bilirubin), exogenous substances (common medications), or substances from sample collection (e.g., powdered gloves) [1] [7].
- Cross-Reactivity Panels: Assess a panel of genetically or structurally related organisms or analytes to identify potential sources of false-positive results. For example, an assay for Virus A should be tested against closely related Virus B and Virus C to ensure it does not generate a positive signal [7].
- Matrix Studies: These studies should be conducted for each specimen type (e.g., serum, plasma, saliva) that will be used with the assay, as the matrix can influence interference [7].
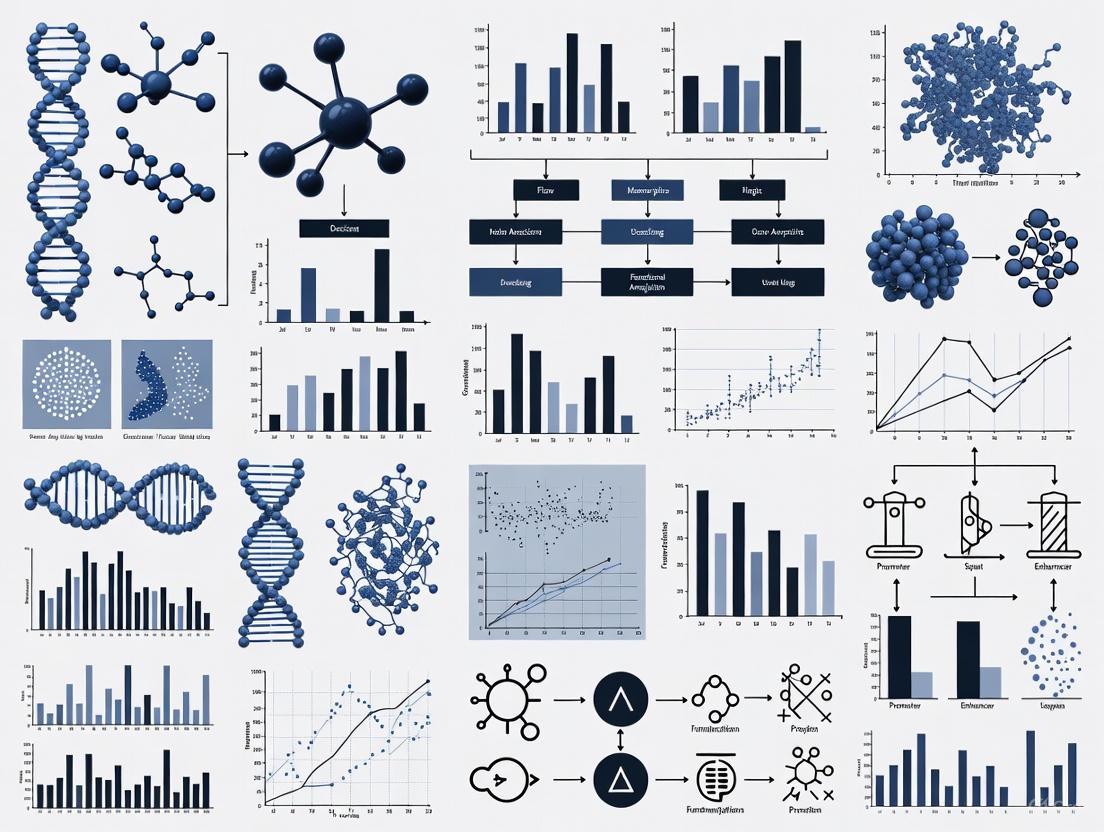
Workflow for Comprehensive Assay Characterization
The following diagram illustrates the logical progression and key components involved in characterizing both the analytical and diagnostic performance of an assay, highlighting their distinct roles in the development pipeline.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and tools required for the rigorous validation of sensitivity and specificity in assay development.
| Tool/Reagent | Function in Validation |
|---|---|
| Reference Standards | Well-characterized materials with known analyte concentrations, essential for calibrating instruments and establishing a standard curve for quantitative assays. |
| Linear/Performance Panels | Commercially available panels of samples across a range of concentrations, used to determine linearity, analytical measurement range, and Limit of Detection (LoD) [7]. |
| Cross-Reactivity Panels | Panels containing related but distinct organisms or analytes, critical for testing and demonstrating the analytical specificity of an assay [7]. |
| ACCURUN-type Controls | Third-party controls that are typically whole-organism or whole-cell, used to appropriately challenge the entire assay workflow from extraction to detection, verifying performance [7]. |
| Interference Kits | Standardized kits containing common interfering substances (e.g., bilirubin, hemoglobin, lipids) to systematically evaluate an assay's susceptibility to interference [7]. |
| Automated Liquid Handlers | Systems like the I.DOT liquid handler automate liquid dispensing, improving precision, minimizing human error, and enhancing the reproducibility of validation data [9]. |
A clear and unwavering distinction between analytical and diagnostic sensitivity and specificity is paramount for researchers and drug development professionals. Analytical metrics define the technical ceiling of an assay in a controlled environment, while diagnostic metrics reveal its practical utility in the messy reality of biological populations. Understanding that a high analytical sensitivity does not automatically confer a high diagnostic sensitivity is a cornerstone of robust assay development and interpretation [1]. The strategic "dialing in" of the sensitivity-specificity trade-off, guided by the specific context of use—whether to avoid missing a toxic drug candidate or to prevent the costly misclassification of a safe one—is a critical skill [5]. By adhering to best practices in experimental validation and leveraging the appropriate tools and controls, scientists can generate reliable, meaningful data that accelerates the drug development pipeline and ultimately leads to safer and more effective therapeutics.
The Critical Role of a Gold Standard in Assay Validation
In the rigorous world of diagnostic and functional assay development, the gold standard serves as the critical benchmark against which all new tests are measured. Often characterized as the "best available" reference method rather than a perfect one, this standard constitutes what has been termed an "alloyed gold standard" in practical applications [10]. The validation of any new assay relies fundamentally on comparing its performance—typically measured through sensitivity (ability to correctly identify true positives) and specificity (ability to correctly identify true negatives)—against this reference point [10]. When developing tests to detect a condition of interest, researchers must measure diagnostic accuracy against an existing gold standard, with the implication that sensitivity and specificity are inherent attributes of the test itself [10].
The process of assay validation comprehensively demonstrates that a test is fit for its intended purpose, systematically evaluating every aspect to ensure it provides accurate, reliable, and meaningful data [11]. According to the Organisation for Economic Co-operation and Development (OECD), validation establishes "the reliability and relevance of a particular approach, method, process or assessment for a defined purpose" [12]. This process is particularly crucial in biomedical fields, where validated assays provide the reliable data needed for informed clinical decisions [11].
The Imperfect Reality: "Alloyed" Gold Standards and Their Consequences
Theoretical Framework of Imperfect Reference Standards
Despite their critical role, gold standards are frequently imperfect in practice, with sensitivity or specificity less than 100% [10]. This imperfection can significantly impact conclusions about the validity of tests measured against it. Foundational work by Gart and Buck (1966) demonstrated that assuming a gold standard is perfect when it is not can dramatically perturb estimates of diagnostic accuracy [10]. They showed formally that when a reference test used as a gold standard is imperfect, observed rates of co-positivity and co-negativity can vary markedly with disease prevalence [10].
The terminology of "gold standard" should be understood to mean that the standard is "the best available" rather than perfect [10]. In reality, no test is inherently perfect, and regulatory agencies have come to accept data from various model systems despite acknowledging inherent shortcomings [12]. The Institute of Medicine (IOM) defines validation as "assessing [an] assay and its measurement performance characteristics [and] determining the range of conditions under which the assay will give reproducible and accurate data" [12].
Quantitative Impact on Measured Specificity
Recent simulation studies examining the impact of imperfect gold standard sensitivity on measured test specificity reveal striking effects, particularly at different levels of condition prevalence [10]. When gold standard sensitivity decreases, researchers observe increasing underestimation of test specificity, with the extent of underestimation magnified at higher prevalence levels [10].
Table 1: Impact of Imperfect Gold Standard Sensitivity on Measured Specificity
| Death Prevalence | Gold Standard Sensitivity | True Test Specificity | Measured Specificity |
|---|---|---|---|
| 98% | 99% | 100% | <67% |
| High (>90%) | 90-99% | 100% | Significantly suppressed |
| 50% | 90% | 100% | Minimal suppression |
This phenomenon was demonstrated in real-world oncology research using the National Death Index (NDI) as a gold standard for mortality endpoints [10]. The NDI aggregates death certificates from all U.S. states, representing the most complete source of certified death information, yet still suffers from imperfect sensitivity due to delays in death reporting and processing [10]. At 98% death prevalence, even near-perfect gold standard sensitivity (99%) resulted in suppression of specificity from the true value of 100% to a measured value of <67% [10].
The following diagram illustrates how an imperfect gold standard affects validation outcomes:
Statistical Correction Methods for Imperfect Reference Standards
When confronting an imperfect gold standard, researchers have developed several statistical correction methods to estimate the true sensitivity and specificity of a new test. The most prominent approaches include:
- Gart and Buck Correction Method: Uses algebraic functions to adjust estimates based on known sensitivity and specificity of the imperfect reference standard [13]
- Staquet et al. Correction Method: Equivalent to the Gart and Buck approach, providing estimators for when the index test and reference standard are conditionally independent [13]
- Brenner Correction Method: Offers estimators for both conditionally independent and dependent scenarios [13]
These "correction methods" aim to correct the estimated sensitivity and specificity of the index test using available information about the imperfect reference standard via algebraic functions, without requiring probabilistic modeling like latent class models [13].
Comparative Performance of Correction Methods
Simulation studies comparing these correction methods reveal distinct performance characteristics under different conditions:
Table 2: Comparison of Statistical Correction Methods for Imperfect Gold Standards
| Method | Key Assumption | Performance Under Ideal Conditions | Limitations |
|---|---|---|---|
| Staquet et al. | Conditional independence | Outperforms Brenner method | Produces illogical results (outside [0,1]) with very high (>0.9) or low (<0.1) prevalence |
| Brenner | Conditional independence | Good performance | Outperformed by Staquet et al. under most conditions |
| Both Methods | Conditional dependence | Fail to estimate accurately when covariance terms not near zero | Require alternative approaches like latent class models |
Under the assumption of conditional independence, the Staquet et al. correction method generally outperforms the Brenner correction method, regardless of disease prevalence and whether the performance of the reference standard is better or worse than the index test [13]. However, when disease prevalence is very high (>0.9) or low (<0.1), the Staquet et al. method can produce illogical results outside the [0,1] range [13]. When tests are conditionally dependent, both methods fail to accurately estimate sensitivity and specificity, particularly when covariance terms between the index test and reference standard are not close to zero [13].
Case Study: Functional Assays for BRCA1 Variant Classification
Experimental Framework and Validation Protocol
The application of rigorous validation principles is exemplified in functional assays for classifying BRCA1 variants of uncertain significance (VUS). Women who inherit inactivating mutations in BRCA1 face significantly increased risks of early-onset breast and ovarian cancers, making accurate variant classification critical for clinical management [14]. The integration of functional data has emerged as a powerful approach to determine whether missense variants lead to loss of function [15].
In one comprehensive study, researchers collected, curated, and harmonized functional data for 2,701 missense variants representing 24.5% of possible missense variants in BRCA1 [15]. The experimental protocol involved:
- Literature Curation and Data Extraction: Annotating all published functional data for BRCA1 missense variants, with specific assay instances tracked as "tracks" [15]
- Data Harmonization: Converting diverse experimental data into binary categorical variables (functional impact versus no functional impact) to enable cross-study comparison [15]
- Reference Panel Establishment: Using a stringent reference panel combining data from the ENIGMA consortium and ClinVar to assess track accuracy [15]
- Evidence Integration: Applying American College of Medical Genetics and Genomics/Association for Molecular Pathology (ACMG/AMP) variant interpretation guidelines to assign evidence criteria [15]
The following workflow diagrams the functional assay validation process:
Validation Outcomes and Performance Metrics
The functional assay validation demonstrated exceptional performance characteristics. Using a reference panel of known variants classified by multifactorial models, the validated assay displayed 1.0 sensitivity (lower bound of 95% confidence interval=0.75) and 1.0 specificity (lower bound of 95% confidence interval=0.83) [14]. This analysis achieved excellent separation of known neutral and pathogenic variants [14].
The integration of data from validated assays provided ACMG/AMP evidence criteria for an overwhelming majority of variants assessed: evidence in favor of pathogenicity for 297 variants or against pathogenicity for 2,058 variants, representing 96.2% of current VUS functionally assessed [15]. This approach significantly reduced the number of VUS associated with the C-terminal region of the BRCA1 protein by approximately 87% [14].
Table 3: BRCA1 Functional Assay Validation Results
| Parameter | Result | Impact |
|---|---|---|
| Sensitivity | 1.0 (95% CI lower bound: 0.75) | Excellent detection of pathogenic variants |
| Specificity | 1.0 (95% CI lower bound: 0.83) | Excellent identification of neutral variants |
| Variants with Evidence | 96.2% of VUS assessed | Dramatic reduction in classification uncertainty |
| VUS Reduction | ~87% decrease in C-terminal region | Significant clinical clarity improvement |
Regulatory Frameworks and Validation Guidelines
International Validation Standards
Formal validation processes have been established across major regulatory jurisdictions to ensure assay reliability and relevance:
United States (ICCVAM): The Interagency Coordinating Committee on the Validation of Alternative Methods (ICCVAM) was established by the National Institute of Environmental Health Sciences (NIEHS) to address the growing need for obtaining regulatory acceptance of new toxicity-testing methods [12]. ICCVAM evaluates fundamental performance characteristics including accuracy, reproducibility, sensitivity, and specificity [11].
European Union (EURL ECVAM): The European Union Reference Laboratory for Alternatives to Animal Testing (EURL ECVAM) coordinates the independent evaluation of the relevance and reliability of tests for specific purposes at the European level [12].
International (OECD): The Organisation for Economic Co-operation and Development (OECD) has established formal international processes for validating test methods, creating guidelines for development and adoption of OECD test guidelines [12].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Research Reagent Solutions for Functional Assay Validation
| Reagent/Resource | Function in Validation | Application Example |
|---|---|---|
| Reference Variants | Benchmarking assay performance against known pathogenic/neutral variants | BRCA1 classification using ENIGMA and ClinVar variants [15] |
| Binary Categorization Framework | Harmonizing diverse data sources into standardized format | Converting functional data to impact/no impact classification [15] |
| Validated Functional Assays | Providing high-quality evidence for variant classification | Transcriptional activation assays for BRCA1 [14] |
| Statistical Correction Methods | Adjusting for imperfect reference standards | Staquet et al. and Brenner methods for accuracy estimation [13] |
| ACMG/AMP Guidelines | Structured framework for evidence integration | Clinical variant classification standards [15] |
The critical role of the gold standard in assay validation cannot be overstated, yet researchers must acknowledge and account for its inherent imperfections. The assumption of a perfect reference standard when validating new tests can lead to significantly biased estimates of sensitivity and specificity, particularly in high-prevalence settings [10]. Through sophisticated statistical correction methods, rigorous validation frameworks like those demonstrated in BRCA1 functional assays, and adherence to international regulatory standards, researchers can navigate the challenges of "alloyed gold standards" to generate reliable, clinically actionable data.
New validation research and review of existing validation studies must consider the prevalence of the conditions being assessed and the potential impact of an imperfect gold standard on sensitivity and specificity measurements [10]. By implementing comprehensive validation programs that encompass both method validation and calibration, laboratories can ensure they generate high-quality data capable of supporting critical research and clinical decisions [11].
Contents
- Core Definitions and Context
- The Confusion Matrix: A Framework for Calculation
- Step-by-Step Calculation Guide
- Advanced Metrics and Threshold Effects
- Experimental Protocols and Research Applications
- Essential Research Toolkit
Core Definitions and Context
In the evaluation of specificity and sensitivity in functional assays, particularly within drug development and biomedical research, the accurate calculation of true positives (TP), true negatives (TN), false positives (FP), and false negatives (FN) is foundational. These metrics form the basis for assessing the performance of diagnostic tests, classification models, and assays by comparing their outputs against a known reference standard, often termed the "ground truth" or "gold standard" [16] [6]. A deep understanding of these concepts allows researchers to quantify the validity and reliability of their methods, a critical step in translating research findings into clinical applications [6].
The core definitions are as follows:
- True Positive (TP): An instance where the test correctly identifies the presence of a condition or the success of an assay. For example, a diseased patient is correctly classified as diseased, or a successful drug interaction is correctly flagged [16] [3].
- False Positive (FP): An instance where the test incorrectly indicates the presence of a condition when it is objectively absent. This is also known as a Type I error [16] [17]. In a functional assay, this might represent a compound incorrectly identified as active.
- True Negative (TN): An instance where the test correctly identifies the absence of a condition. A healthy patient is correctly classified as healthy, or an inactive compound is correctly identified [16] [3].
- False Negative (FN): An instance where the test fails to detect a condition that is present. This is also known as a Type II error [16] [17]. In research, this could be a therapeutically active compound that the assay fails to detect.
These outcomes are fundamental to deriving essential performance metrics such as sensitivity, specificity, and predictive values, which are prevalence-dependent and crucial for understanding a test's utility in a specific population [6] [3].
The Confusion Matrix: A Framework for Calculation
The confusion matrix, also known as an error matrix, is the standard table layout used to visualize and calculate TP, TN, FP, and FN [18]. It provides a concise summary of the performance of a classification algorithm or diagnostic test. The matrix contrasts the actual condition (ground truth) against the predicted condition (test result).
The following diagram illustrates the logical structure and relationships within a standard binary confusion matrix.
The structure of the confusion matrix allows researchers to quickly grasp the distribution of correct and incorrect predictions. The diagonal cells (TP and TN) represent correct classifications, while the off-diagonal cells (FP and FN) represent the two types of errors [18]. This visualization is critical for identifying whether a test is prone to over-diagnosis (high FP) or under-diagnosis (high FN), enabling targeted improvements in assay design or model training. The terminology is applied consistently across different fields, from clinical medicine to machine learning [16] [17].
Table 1: Comparison of Outcome Terminology Across Domains
| Actual Condition | Predicted/Test Outcome | Outcome Term | Clinical Context | Machine Learning Context |
|---|---|---|---|---|
| Positive | Positive | True Positive (TP) | Diseased patient correctly identified | Spam email correctly classified as spam |
| Positive | Negative | False Negative (FN) | Diseased patient missed by test | Spam email incorrectly sent to inbox |
| Negative | Positive | False Positive (FP) | Healthy patient incorrectly flagged | Legitimate email incorrectly marked as spam |
| Negative | Negative | True Negative (TN) | Healthy patient correctly identified | Legitimate email correctly delivered to inbox |
Step-by-Step Calculation Guide
Calculating TP, TN, FP, and FN requires a dataset with known ground truth labels and corresponding test or model predictions. The process involves systematically comparing each pair of results and tallying them into the four outcome categories [18].
1. Experimental Protocol for Data Collection:
- Define Gold Standard: Establish a reliable reference method (e.g., a clinically proven diagnostic test, mass spectrometry confirmation, or expert manual review) to determine the true condition of each sample [6].
- Run Test Method: Apply the new assay or classification model to the same set of samples.
- Record Results: For each sample, record both the result from the gold standard (Actual Condition) and the result from the test method (Predicted Condition).
2. Workflow for Populating the Confusion Matrix: The following workflow diagram outlines the logical decision process for categorizing each sample result into TP, TN, FP, or FN.
3. Worked Calculation Example:
Consider a study evaluating a new blood test for a disease on a cohort of 1,000 individuals [6]. The results were summarized as follows:
- A total of 427 individuals had positive test findings, and 573 had negative findings.
- Out of the 427 with positive findings, 369 actually had the disease.
- Out of the 573 with negative findings, 558 did not have the disease.
To calculate the four core metrics, we first construct the 2x2 confusion matrix.
Table 2: Confusion Matrix for Blood Test Example
| Predicted Condition (Test Result) | |||
|---|---|---|---|
| Positive | Negative | ||
| Actual Condition (Gold Standard) | Positive | True Positive (TP) = 369 | False Negative (FN) = ? |
| Negative | False Positive (FP) = ? | True Negative (TN) = 558 |
The missing values can be calculated using the row and column totals:
- Total Actual Positives (P): The total number of individuals who truly had the disease. This is not directly given but can be derived. We know from the positive test column that TP = 369. We also know the total number of positive tests is 427.
- False Positives (FP): The number of individuals without the disease who tested positive. FP = Total Positive Tests - TP = 427 - 369 = 58 [6].
- Total Actual Negatives (N): The total number of individuals without the disease. We know TN = 558. We also know the total number of negative tests is 573.
- False Negatives (FN): The number of individuals with the disease who tested negative. FN = Total Negative Tests - TN = 573 - 558 = 15 [6].
- Total Actual Positives (P) confirmed: TP + FN = 369 + 15 = 384.
- Total Actual Negatives (N) confirmed: FP + TN = 58 + 558 = 616.
The completed confusion matrix is shown below.
Table 3: Completed Confusion Matrix for Blood Test Example
| Predicted Condition (Test Result) | Total (Actual) | |||
|---|---|---|---|---|
| Positive | Negative | |||
| Actual Condition (Gold Standard) | Positive | TP = 369 | FN = 15 | P = 384 |
| Negative | FP = 58 | TN = 558 | N = 616 | |
| Total (Predicted) | PP = 427 | PN = 573 | Total = 1000 |
From this matrix, key performance metrics are derived [6] [3]:
- Sensitivity = TP / (TP + FN) = 369 / 384 ≈ 0.961 or 96.1%
- Specificity = TN / (TN + FP) = 558 / 616 ≈ 0.906 or 90.6%
- Positive Predictive Value (PPV) = TP / (TP + FP) = 369 / 427 ≈ 0.864 or 86.4%
- Negative Predictive Value (NPV) = TN / (TN + FN) = 558 / 573 ≈ 0.974 or 97.4%
Advanced Metrics and Threshold Effects
The classification threshold is a critical concept that directly influences the values in the confusion matrix. It is the probability cut-off point used to assign a continuous output (e.g., from a logistic regression model) to a positive or negative class [17]. For instance, in spam detection, if an email's predicted probability of being spam is above the threshold (e.g., 0.5), it is classified as "spam"; otherwise, it is "not spam" [17].
Effect of Threshold Adjustment:
- Increasing the Threshold: Makes the test more stringent.
- Fewer False Positives (FP): The test is less likely to incorrectly label a negative as positive.
- Potentially More False Negatives (FN): The test may now miss some true positives that have scores just below the higher threshold.
- Result: Specificity increases, Sensitivity decreases [17].
- Decreasing the Threshold: Makes the test more lenient.
- Fewer False Negatives (FN): The test is more likely to catch true positives.
- Potentially More False Positives (FP): The test may now incorrectly label more negatives as positives.
- Result: Sensitivity increases, Specificity decreases [17].
This trade-off between sensitivity and specificity is inherent to all diagnostic tests and classification systems [19] [3]. The optimal threshold is not always 0.5; it must be chosen based on the relative costs of FP and FN errors in a specific application. For example, in cancer screening, a low threshold might be preferred to minimize FN (missed cancers), even at the cost of more FP (leading to further testing) [17].
The Receiver Operating Characteristic (ROC) Curve The ROC curve is a fundamental tool for visualizing the trade-off between sensitivity and specificity across all possible classification thresholds [19]. It plots the True Positive Rate (Sensitivity) against the False Positive Rate (1 - Specificity) at various threshold settings.
- The Area Under the Curve (AUC) provides a single metric to evaluate the overall performance of a test. An AUC of 1.0 represents a perfect test, while an AUC of 0.5 represents a test with no discriminative power, equivalent to random guessing [19].
- Researchers use ROC curves to compare different assays or models and to select the optimal operating point (threshold) for their specific needs [19].
Experimental Protocols and Research Applications
In the context of evaluating specificity and sensitivity in functional assays, the calculation of the confusion matrix is integrated into rigorous experimental protocols.
Protocol for Assay Validation:
- Sample Preparation: Create a blinded panel of samples with known activity states (e.g., using recombinant proteins, cell lines with known genetic mutations, or compounds with confirmed bioactivity). The "gold standard" should be a well-characterized and orthogonal method [6].
- Assay Execution: Run the functional assay on the entire panel according to standardized operating procedures. Record the raw output data (e.g., fluorescence intensity, cell count, enzymatic rate).
- Data Analysis and Thresholding: Convert raw data into categorical results (Positive/Negative) by applying a pre-defined threshold. This threshold may be established from control samples or using ROC analysis on a training set [19].
- Unblinding and Matrix Construction: Unblind the samples and construct the confusion matrix by comparing the assay's categorical results to the known sample states.
- Performance Calculation: Calculate sensitivity, specificity, PPV, NPV, and other relevant metrics (e.g., Likelihood Ratios, Accuracy) from the matrix [6].
Application in High-Throughput Screening (HTS): In drug discovery, HTS assays screen thousands of compounds. The confusion matrix helps quantify the assay's quality. A high rate of false positives leads to wasted resources on follow-up studies, while false negatives mean missing potential drug candidates. Metrics derived from the matrix are used to optimize assay conditions and set hit-selection thresholds that balance sensitivity and specificity [6].
Essential Research Toolkit
The following table details key reagents, tools, and resources essential for conducting research involving the calculation and application of classification metrics.
Table 4: Essential Research Reagents and Tools for Assay Evaluation
| Item Name | Function/Application | Relevance to Specificity/Sensitivity Research |
|---|---|---|
| Gold Standard Reference Material | Provides the ground truth for sample status (e.g., purified active/inactive compound, genetically defined cell line). | Critical for accurately determining TP, TN, FP, and FN. The validity of all calculated metrics depends on the accuracy of the gold standard [6]. |
| Statistical Software (R, Python, SciVal) | Used for data analysis, calculation of metrics, generation of confusion matrices, and plotting ROC curves. | Automates the computation of sensitivity, specificity, PPV, NPV, and AUC. Essential for handling large datasets from high-throughput experiments [19] [20]. |
| Blinded Sample Panels | A set of samples where the experimenter is unaware of the true status during testing to prevent bias. | Ensures the objectivity of the test results, leading to a more reliable and unbiased confusion matrix [6]. |
| Scimago Journal Rank (SJR) & CiteScore | Bibliometric tools for comparing journal impact and influence. | Used by researchers to identify high-quality journals in which to publish findings related to assay validation and diagnostic accuracy [20]. |
| FDA Drug Development Tool (DDT) Qualification Programs | Regulatory pathways for qualifying drug development tools for a specific context of use. | Provides a framework for validating biomarkers and other tools, where demonstrating high sensitivity and specificity is often a key requirement [21]. |
In the realm of diagnostic testing and assay development, sensitivity and specificity are foundational metrics that mathematically describe the accuracy of a test in classifying the presence or absence of a target condition [3]. These metrics are particularly crucial in functional assays research, where evaluating the performance of new detection methods against reference standards is essential for validating their clinical and research utility.
Sensitivity, or the true positive rate, is defined as the probability that a test correctly classifies an individual as 'diseased' or 'positive' when the condition is truly present [22]. It answers the question: "If the condition is present, how likely is the test to detect it?" [3]. Mathematically, sensitivity is calculated as the number of true positives divided by the sum of true positives and false negatives [3] [6]. A test with 100% sensitivity would identify all actual positive cases, meaning there would be no false negatives.
Specificity, or the true negative rate, is defined as the probability that a test correctly classifies an individual as 'disease-free' or 'negative' when the condition is truly absent [22]. It answers the question: "If the condition is absent, how likely is the test to correctly exclude it?" [3]. Mathematically, specificity is calculated as the number of true negatives divided by the sum of true negatives and false positives [3] [6]. A test with 100% specificity would correctly identify all actual negative cases, meaning there would be no false positives.
These metrics are intrinsically linked to the concept of a reference standard (often referred to as a gold standard), which is the best available method for definitively diagnosing the condition of interest [22]. New diagnostic tests or functional assays are validated by comparing their performance against this reference standard, typically using a 2x2 contingency table to categorize results into true positives, false positives, true negatives, and false negatives [23] [22].
The Fundamental Trade-off: Theory and Mechanisms
The inverse relationship between sensitivity and specificity represents a core challenge in diagnostic test and assay development [3] [22]. This trade-off means that as sensitivity increases, specificity typically decreases, and vice-versa [6]. This phenomenon is not due to error in test design, but rather an inherent property of classification systems, particularly when distinguishing between conditions based on a continuous measurement.
The primary mechanism driving this trade-off is the positioning of the decision threshold or cutoff point on a continuous measurement scale [24]. Many diagnostic tests, including immunoassays and molecular detection assays, produce results on a continuum. Establishing a cutoff point to dichotomize results into "positive" or "negative" categories forces a balance between the two types of classification errors: false negatives and false positives.
- A highly sensitive test uses a liberal cutoff that minimizes false negatives but accepts more false positives, thereby reducing specificity [3]. This approach is exemplified by a test configured to cast a wide net, ensuring it catches all true cases but also captures some non-cases.
- A highly specific test uses a conservative cutoff that minimizes false positives but accepts more false negatives, thereby reducing sensitivity [3]. This approach is exemplified by a test configured to only identify the most clear-cut cases, missing some true cases but rarely misclassifying non-cases.
This relationship is powerfully summarized by the mnemonics SnNOUT and SpPIN:
- SnNOUT: A highly SeNsitive test, when Negative, rules OUT the disease [22]. This is because the test rarely misses true positive cases.
- SpPIN: A highly SPecific test, when Positive, rules IN the disease [22]. This is because the test rarely misclassifies healthy individuals as positive.
The following diagram illustrates how moving the decision threshold affects the balance between sensitivity and specificity, false positives, and false negatives:
Experimental Evidence and Quantitative Data
The inverse relationship between sensitivity and specificity is consistently demonstrated across diverse research domains, from medical diagnostics to machine learning. The following table summarizes quantitative findings from various studies that illustrate this trade-off in practice.
Table 1: Experimental Data Demonstrating Sensitivity-Specificity Trade-offs Across Fields
| Field/Application | Test/Condition | High Sensitivity Scenario | High Specificity Scenario | Reference |
|---|---|---|---|---|
| General Diagnostic Principle | Cut-off Adjustment | Sensitivity: ~91%, Specificity: ~82% | Sensitivity: ~82%, Specificity: ~91% | [3] |
| Medical Diagnostics (IOP) | Intraocular Pressure for Glaucoma | Lower cut-off (e.g., 12 mmHg): High Sensitivity, Low Specificity | Higher cut-off (e.g., 35 mmHg): Low Sensitivity, High Specificity (SpPIN) | [22] |
| Cancer Detection (Liquid Biopsy) | Early-Stage Lung Cancer | Sensitivity: 84%, Specificity: 100% (as reported in one study) | N/A | [24] |
| Machine Learning / Public Health | Model Optimization | Context: High cost of missing disease (e.g., cancer). High Sensitivity prioritized. | Context: High cost of false alarms (e.g., drug side effects). High Specificity prioritized. | [25] |
The data from general diagnostic principles shows a clear inverse correlation, where a configuration favoring one metric (e.g., ~91% sensitivity) results in a lower value for the other (e.g., ~82% specificity), and vice versa [3]. The example of using intraocular pressure (IOP) for glaucoma screening perfectly encapsulates the trade-off. A low cutoff pressure (e.g., 12 mmHg) ensures almost no glaucoma cases are missed (high sensitivity, fulfilling SnNOUT) but incorrectly flags many healthy individuals (low specificity). Conversely, a very high cutoff (e.g., 35 mmHg) means a positive result is almost certainly correct (high specificity, fulfilling SpPIN) but misses many true glaucoma cases (low sensitivity) [22].
Context is critical in interpreting these trade-offs. In cancer detection via liquid biopsy, a reported 84% sensitivity and 100% specificity would be considered an excellent profile for a screening test, as it prioritizes ruling out the disease without generating excessive false positives [24]. The prioritization of sensitivity versus specificity is ultimately a strategic decision based on the consequences of error [25].
Research Reagent Solutions and Methodologies
The development and optimization of functional assays with defined sensitivity and specificity profiles depend on a suite of critical research reagents and methodologies. The selection and quality of these components directly influence the assay's performance, reproducibility, and ultimately, the position of its decision threshold.
Table 2: Essential Research Reagent Solutions for Assay Development
| Reagent/Material | Function in Assay Development | Impact on Sensitivity & Specificity |
|---|---|---|
| Reference Standard Material | Provides the definitive measurement against which the new test is validated; considered the 'truth' for categorizing samples in the 2x2 table [22]. | The validity of the entire sensitivity/specificity analysis depends on the accuracy of the reference standard. An imperfect standard introduces misclassification errors [23]. |
| Well-Characterized Biobanked Samples | Comprise panels of known positive and negative samples used to calibrate the assay and establish initial performance metrics [24]. | Using samples with clearly defined status is crucial for accurately calculating true positive and true negative rates during the assay validation phase. |
| High-Affinity Binding Partners | Includes monoclonal/polyclonal antibodies, aptamers, or receptors that specifically capture and detect the target analyte [24]. | High affinity and specificity reduce cross-reactivity (improving specificity) and enhance the signal from genuine positives (improving sensitivity). |
| Signal Amplification Systems | Enzymatic (e.g., HRP, ALP), fluorescent, or chemiluminescent systems that amplify the detection signal from low-abundance targets. | Directly enhances the ability to detect low levels of analyte, a key factor in improving the analytical sensitivity of an assay. |
| Blocking Agents & Buffer Components | Reduce non-specific binding and background noise in the assay system (e.g., BSA, non-fat milk, proprietary blocking buffers). | Critical for minimizing false positive signals, thereby directly improving the specificity of the assay. |
The experimental protocol for establishing an assay's sensitivity and specificity involves a clear, multi-stage workflow that moves from sample collection and testing to result calculation and threshold optimization, as illustrated below:
Detailed Experimental Protocol:
Sample Collection and Reference Standard Testing: A cohort of subjects is recruited, and each undergoes testing with the reference standard to definitively classify them as either having the condition (Diseased) or not having the condition (Healthy) [22]. This establishes the "true" status for each subject.
Experimental Assay Performance and Measurement: All subjects, regardless of their reference standard status, are then tested using the new experimental assay or diagnostic test. The results from this test are recorded, typically as continuous or ordinal data [23].
Result Categorization (2x2 Table Construction): The results from the reference standard and the experimental test are compared for each subject, and subjects are assigned to one of four categories in a 2x2 contingency table [6] [22]:
- True Positives (TP): Subjects with the condition who test positive on the experimental assay.
- False Negatives (FN): Subjects with the condition who test negative on the experimental assay.
- False Positives (FP): Subjects without the condition who test positive on the experimental assay.
- True Negatives (TN): Subjects without the condition who test negative on the experimental assay.
Metric Calculation: Sensitivity and Specificity are calculated using the values from the 2x2 table [3] [6]:
- Sensitivity = TP / (TP + FN)
- Specificity = TN / (TN + FP)
Threshold Optimization and ROC Analysis: If the experimental assay produces a continuous output, steps 3 and 4 are repeated for multiple potential decision thresholds. The resulting pairs of sensitivity and specificity values are plotted to generate a Receiver Operating Characteristic (ROC) curve [26]. The area under this curve (AUC) provides a single measure of overall test discriminative ability, independent of any single threshold.
Implications for Research and Drug Development
Understanding and strategically managing the sensitivity-specificity trade-off is paramount for researchers and drug development professionals. This balance directly impacts various stages of the pipeline, from initial biomarker discovery to clinical trial enrollment and companion diagnostic development.
In biomarker discovery and validation, the choice between a high-sensitivity or high-specificity assay configuration depends on the intended application. A screening assay designed to identify potential candidates from a large population often prioritizes high sensitivity to minimize false negatives, ensuring few true cases are missed for further investigation [3] [24]. Conversely, a confirmatory assay used to validate hits from a primary screen must prioritize high specificity to minimize false positives, thereby ensuring that only truly promising candidates advance in the costly and resource-intensive drug development pipeline [3].
For patient stratification and clinical trial enrollment, diagnostics with high specificity are crucial. Enrolling patients into a trial based on a biomarker requires high confidence that the biomarker is truly present (SpPIN) to ensure the trial population is homogenous and accurately defined [22]. This increases the statistical power of the trial and the likelihood of demonstrating a true treatment effect. Misclassification due to a low-specificity test can dilute the treatment effect by including biomarker-negative patients, potentially leading to trial failure.
The trade-off also fundamentally influences risk assessment and decision-making. The consequences of false negatives versus false positives differ vastly across contexts [25]. In diseases like cancer, where missing a diagnosis (false negative) can be fatal, high sensitivity is paramount. In contrast, for conditions where a false positive diagnosis may lead to invasive, risky, or expensive follow-up procedures or treatments, high specificity becomes the critical metric [3] [25]. Researchers must quantitatively evaluate this trade-off using tools like the ROC curve to select a threshold that aligns with the clinical and research objectives, a process that is as much strategic as it is statistical [26].
In the evaluation of specificity and sensitivity in functional assays, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) represent critical performance metrics that bridge statistical measurement with clinical and research utility [23]. While sensitivity and specificity describe the inherent accuracy of a test relative to a reference standard, PPV and NPV quantify the practical usefulness of test results in real-world contexts [27] [28]. These predictive values answer fundamentally important questions for researchers and clinicians: When a test yields a positive result, what is the probability that the target condition is truly present? Conversely, when a test yields a negative result, what is the probability that the condition is truly absent? [29] [30]
Unlike sensitivity and specificity, which are considered intrinsic test characteristics, PPV and NPV possess the crucial attribute of being dependent on disease prevalence within the study population [27] [31] [28]. This prevalence dependence creates a dynamic relationship that must be thoroughly understood to properly interpret test performance across different populations and settings. For researchers developing diagnostic assays, appreciating this relationship is essential for designing appropriate validation studies and establishing clinically relevant performance requirements [30].
Defining Key Performance Metrics
Fundamental Definitions and Calculations
The evaluation of diagnostic tests typically begins with a 2×2 contingency table that cross-classifies subjects based on their true disease status (as determined by a reference standard) and their test results [32] [33]. This classification generates four fundamental categories:
- True Positives (TP): Subjects with the disease who test positive
- False Positives (FP): Subjects without the disease who test positive
- False Negatives (FN): Subjects with the disease who test negative
- True Negatives (TN): Subjects without the disease who test negative [32]
From these categories, the key performance metrics are calculated as follows:
- Sensitivity = TP / (TP + FN) × 100 [33] [23]
- Specificity = TN / (TN + FP) × 100 [33] [23]
- Positive Predictive Value (PPV) = TP / (TP + FP) × 100 [32] [33] [30]
- Negative Predictive Value (NPV) = TN / (TN + FN) × 100 [32] [33] [30]
- Prevalence = (TP + FN) / (TP + FN + FP + TN) × 100 [31] [30]
Conceptual Distinctions Between Test Characteristics
A critical conceptual distinction exists between sensitivity/specificity and predictive values [23]. Sensitivity and specificity are test-oriented metrics that evaluate the assay's performance against a reference standard. In contrast, PPV and NPV are result-oriented metrics that assess the clinical meaning of a specific test result [28]. This distinction has profound implications for how these statistics are interpreted and applied in research and clinical practice.
Sensitivity and specificity remain constant for a given test regardless of the population being tested (assuming consistent test implementation) because they are calculated vertically in the 2×2 table [30]. Conversely, PPV and NPV fluctuate substantially with changes in disease prevalence because they are calculated horizontally across the 2×2 table [27] [28]. This fundamental difference explains why a test with excellent sensitivity and specificity may perform poorly in certain populations with unusually high or low disease prevalence.
The Mathematical Relationship Between Prevalence and Predictive Values
Formulas Connecting Prevalence to Predictive Values
The mathematical relationship between prevalence, test characteristics, and predictive values can be expressed through Bayesian probability principles [32] [29]. The formulas for calculating PPV and NPV from sensitivity, specificity, and prevalence are:
PPV = (Sensitivity × Prevalence) / [(Sensitivity × Prevalence) + (1 - Specificity) × (1 - Prevalence)] [32] [29]
NPV = [Specificity × (1 - Prevalence)] / [Specificity × (1 - Prevalence) + (1 - Sensitivity) × Prevalence] [32] [29]
These formulas demonstrate mathematically how predictive values are functions of both test performance (sensitivity and specificity) and population characteristics (prevalence) [34]. The relationship can be visualized through the following conceptual diagram:
Conceptual diagram showing how prevalence, sensitivity, and specificity influence PPV and NPV.
Impact of Prevalence Changes on Predictive Values
The direction and magnitude of prevalence's effect on predictive values follow predictable patterns [27] [31] [28]:
- As prevalence increases: PPV increases while NPV decreases
- As prevalence decreases: PPV decreases while NPV increases
This relationship occurs because as a disease becomes more common in a population (higher prevalence), a positive test result is more likely to represent a true positive than a false positive, thereby increasing PPV [31]. Simultaneously, in high-prevalence populations, a negative test result is more likely to represent a false negative than a true negative, thereby decreasing NPV [28]. The inverse relationship applies when prevalence decreases.
The following table demonstrates how prevalence impacts PPV and NPV for a test with 95% sensitivity and 90% specificity:
| Prevalence | PPV | NPV |
|---|---|---|
| 1% | 8.8% | >99.9% |
| 5% | 33.3% | 99.7% |
| 10% | 51.4% | 99.4% |
| 20% | 70.4% | 98.7% |
| 50% | 90.5% | 94.7% |
Table 1: Impact of prevalence on PPV and NPV for a test with 95% sensitivity and 90% specificity [27] [30].
Experimental Evidence and Practical Demonstrations
Case Study: Acetaminophen Toxicity Test
A compelling example of prevalence impact comes from a study of a point-of-care test (POCT) for acetaminophen toxicity [28]. Researchers evaluated the test characteristics across two populations with different prevalence rates:
Population A (6% prevalence):
- Sensitivity: 50%, Specificity: 68%
- PPV: 9%, NPV: 96%
Population B (1% prevalence):
- Sensitivity: 50%, Specificity: 68%
- PPV: 2%, NPV: 99%
This case demonstrates that despite identical sensitivity and specificity, the PPV dropped dramatically from 9% to 2% when prevalence decreased from 6% to 1%, while NPV increased slightly from 96% to 99% [28]. For researchers, this highlights the critical importance of selecting appropriate validation populations that reflect the intended use setting for the assay.
Experimental Protocol for Evaluating Predictive Values
To properly evaluate PPV and NPV in diagnostic assay development, researchers should implement the following methodological protocol:
Define Reference Standard: Establish and document the criterion (gold standard) method that will serve as the reference for determining true disease status [33] [23]. This standard must be applied consistently to all study participants.
Select Study Population: Recruit a representative sample that reflects the spectrum of disease severity and patient characteristics expected in the target use population [33]. The sample size should provide sufficient statistical power for precise estimates.
Blinded Testing: Perform both the index test (new assay) and reference standard test on all participants under blinded conditions where test interpreters are unaware of the other test's results [23].
Construct 2×2 Table: Tabulate results comparing the index test against the reference standard [32] [30].
Calculate Metrics: Compute sensitivity, specificity, PPV, NPV, and prevalence with corresponding confidence intervals [35].
Stratified Analysis: If possible, analyze performance across subgroups with different prevalence rates to demonstrate how predictive values vary [28].
Research Reagent Solutions for Predictive Value Studies
The following reagents and methodologies are essential for conducting robust evaluations of diagnostic test performance:
| Research Reagent/Methodology | Function in Predictive Value Studies |
|---|---|
| Reference Standard Materials | Establish definitive disease status for calculating true positives and negatives [33] [23] |
| Validated Positive Controls | Ensure test sensitivity by confirming detection of known positive samples [30] |
| Validated Negative Controls | Ensure test specificity by confirming non-reactivity with known negative samples [30] |
| Population Characterization Assays | Accurately determine prevalence in study populations through independent methods [31] [28] |
| Statistical Analysis Software | Compute performance metrics with confidence intervals (e.g., R, SAS) [35] |
| Blinded Assessment Protocols | Minimize bias in test interpretation and result recording [23] |
Table 2: Essential research reagents and methodologies for evaluating predictive values in diagnostic studies.
Implications for Diagnostic Assay Development and Evaluation
Setting Appropriate Performance Requirements
When establishing sensitivity and specificity requirements for new assays, researchers must consider the intended use population's prevalence and the desired PPV and NPV [30]. For example, if a test must achieve ≥90% PPV and ≥99% NPV with an expected prevalence of 20%, the required sensitivity and specificity would be approximately 96% and 98% respectively [30]. This forward-thinking approach ensures that tests demonstrate adequate predictive performance in their target implementation settings.
Applications in Screening vs Diagnostic Contexts
The relationship between prevalence and predictive values has particular significance when considering screening versus diagnostic applications [23]. Screening tests are typically applied to populations with lower disease prevalence, which consequently produces lower PPVs even with reasonably high sensitivity and specificity [29]. This explains why positive screening tests often require confirmation with more specific diagnostic tests [23]. Researchers developing screening assays must recognize that apparently strong sensitivity and specificity may translate to clinically unacceptable PPV in low-prevalence populations.
PPV and NPV serve as crucial connectors between abstract test characteristics and practical diagnostic utility. Understanding how these predictive values fluctuate with disease prevalence is essential for designing appropriate validation studies, interpreting diagnostic test results, and establishing clinically relevant performance requirements. For researchers working with specificity and sensitivity functional assays, incorporating prevalence considerations into assay development and evaluation represents a critical step toward creating diagnostically useful tools that perform reliably in their intended settings. The mathematical relationships and experimental evidence presented provide a foundation for making informed decisions throughout the diagnostic development process.
Practical Measurement: Techniques for Quantifying Assay Performance
Establishing a Validated Panel of Positive and Negative Controls
In the rigorous field of biomolecular research and diagnostic assay development, the establishment of a validated panel of positive and negative controls is a critical foundation for ensuring data integrity, reproducibility, and translational relevance. Controls serve as the benchmark against which experimental results are calibrated, providing evidence that an immunohistochemistry (IHC) test or other functional assay is performing with its expected sensitivity and specificity as characterized during technical optimization [36]. Within the context of evaluating specificity and sensitivity in functional assays, a well-designed control panel transcends mere quality checking; it becomes an indispensable tool for differentiating true biological signals from experimental artifacts, thereby directly impacting the reliability of scientific conclusions and, in clinical contexts, patient care decisions.
The fundamental principle behind controls is relatively straightforward: positive controls confirm that the experimental setup is capable of producing a positive result under the known conditions, while negative controls verify that observed effects are due to the specific experimental variable and not nonspecific interactions or procedural errors [37]. However, the practical implementation of a comprehensive and validated panel requires careful consideration of biological context, technical parameters, and the specific assay platform employed. This guide provides a systematic approach to establishing such a panel, objectively comparing performance across common assay platforms, and detailing the experimental protocols necessary for rigorous validation.
Theoretical Foundations: Types and Purposes of Controls
A validated control panel is not monolithic; it comprises several distinct types of controls, each designed to monitor different aspects of assay performance. Understanding the classification and specific purpose of each control type is the first step in constructing a robust panel.
Positive Controls
Positive controls are samples or tissues known to express the target antigen or exhibit the phenomenon under investigation. They primarily monitor the calibration of the assay system and protocol sensitivity [36]. A comprehensive panel should include:
- External Positive Tissue Controls (Ext-PTC): Separate tissue sections or cell lines known to express the target antigen. These should ideally undergo fixation and processing identical to the test samples to ensure comparable performance [36].
- Internal Positive Tissue Controls (Int-PTC): Native, intrinsic elements within the patient's own test tissue that are known to consistently express the target antigen. The presence of expected staining in these internal controls provides strong evidence of proper assay function for that specific sample [36].
For maximum confidence, positive controls should represent a range of expression levels, including both low-expression and high-expression samples, to demonstrate that the assay sensitivity is sufficient to detect the target across its biological spectrum [38] [36].
Negative Controls
Negative controls are essential for evaluating the specificity of an IHC test and for identifying false-positive staining reactions [36]. They are categorized based on their preparation and specific application:
- Negative Reagent Controls (NRCs): These controls involve replacing the primary antibody with a non-immune immunoglobulin of the same species, isotype, and concentration. This identifies false-positive reactions due to nonspecific binding of the primary antibody or components of the detection system [36].
- Negative Tissue Controls (NTCs): These consist of tissues or cells where the target protein is known to be absent. The absence of staining in these samples confirms that the detected signal in test samples is specific to the target antigen and not due to cross-reactivity or other artifacts [38].
Table 1: Classification and Application of Key Control Types
| Control Type | Purpose | Composition | Interpretation of Valid Result |
|---|---|---|---|
| External Positive Control (Ext-PTC) | Monitor assay sensitivity and calibration | Tissue/cell line with known target expression, processed like test samples | Positive staining in expected distribution and intensity |
| Internal Positive Control (Int-PTC) | Monitor assay performance for a specific sample | Indigenous elements within the test tissue known to express the target | Positive staining in expected indigenous elements |
| Negative Reagent Control (NRC) | Identify false-positives from antibody/detection system | Primary antibody replaced with non-immune Ig | Absence of specific staining |
| Negative Tissue Control (NTC) | Confirm target-specific staining | Tissue/cell line known to lack the target antigen | Absence of specific staining |
The following diagram illustrates the logical decision-making process for incorporating these different controls into a validated assay system, ensuring both sensitivity and specificity are monitored.
Diagram: Control Implementation Logic for Assay Validation
Establishing a Validated Control Panel: A Step-by-Step Methodology
Building a validated panel requires a strategic approach that encompasses material selection, experimental design, and data interpretation. The following protocols provide a framework for this process.
Selection and Sourcing of Control Materials
The foundation of a reliable control panel is the careful selection of its components.
- Cell Lines and Tissues: Cell lines that endogenously express or lack the protein of interest are widely used as controls [38]. For instance, in validating a CD19 antibody, the RAJI B-cell line served as a positive control, while JURKAT (T-cell) and U937 (monocytic) lines acted as negative controls [38]. The use of well-characterized tissue microarrays (TMAs) containing both positive and negative control tissues on a single slide is a powerful approach for efficient validation [38].
- Transfected Cells: For targets where naturally expressing cell lines are unavailable, transfected cells (e.g., COS-7, HEK293T) expressing the target antigen via cDNA are valuable positive controls. The negative control in this case should consist of cells transfected with the empty vector only [38]. A critical preliminary step is to verify that the host cell line does not endogenously express the target or a cross-reactive protein.
- Purified Proteins: Purified proteins or peptides are ideal positive controls in techniques like Western blot and ELISA. They can be used to verify antibody specificity and, in ELISA, to generate standard curves for quantification [37].
- Induced Systems: For inducible targets, systems that allow controlled expression, such as the tetracycline (TetON)-inducible system in transgenic mice used for Nanog validation, provide dynamic positive controls with varying expression levels [38].
Experimental Protocol for Control Panel Validation via Western Blot
Western blotting is a cornerstone technique for protein analysis, and its validation requires a multi-faceted control panel.
1. Sample Preparation:
- Test Samples: Lyse cells or tissues of interest in an appropriate RIPA buffer supplemented with protease and phosphatase inhibitors.
- Positive Controls: Use a cell lysate known to express the target protein (e.g., a characterized cell line or a lysate from Rockland, which offers pre-validated products) [37]. For transfected systems, use lysates from cells expressing the recombinant target.
- Negative Controls: Use a cell lysate from a source known to lack the target protein (e.g., a different cell lineage) or from empty-vector transfectants [38].
- Loading Control: Prepare samples for a constitutively expressed housekeeping protein (e.g., β-actin, GAPDH, α-tubulin) with a molecular weight distinct from the target to verify equal protein loading across all lanes [37].
2. Gel Electrophoresis and Transfer:
- Load equal amounts of protein (20-30 µg) from each sample, including positive, negative, and loading controls, onto an SDS-PAGE gel (4-20% gradient).
- Perform electrophoresis and transfer to a PVDF or nitrocellulose membrane using standard protocols.
3. Immunoblotting:
- Block the membrane with 5% non-fat milk in TBST for 1 hour.
- Incubate with the primary antibody against your target protein, diluted in blocking buffer, overnight at 4°C.
- Include a separate blot or strip for the loading control antibody.
- Wash the membrane and incubate with an appropriate HRP-conjugated secondary antibody for 1 hour at room temperature.
- Detect the signal using a chemiluminescent substrate and image the blot.
4. Interpretation:
- A valid result shows a band at the expected molecular weight in the positive control and test samples, with no band in the negative control.
- The loading control should show uniform band intensity across all lanes, confirming equal loading.
Table 2: Example Control Panel for a CD19 Western Blot
| Sample Type | Expected Result (CD19) | Purpose | Example Material |
|---|---|---|---|
| Positive Control | Band at ~95 kDa | Confirm assay works | RAJI B-cell lysate [38] |
| Negative Control | No band | Confirm antibody specificity | JURKAT T-cell lysate [38] |
| Loading Control | Uniform band (e.g., 42 kDa for β-actin) | Verify equal protein loading | All sample lanes |
Experimental Protocol for Control Panel Validation via Immunohistochemistry (IHC)
IHC presents unique challenges for validation, particularly concerning tissue integrity and staining interpretation.
1. Slide Preparation:
- Test Tissues: Section formalin-fixed, paraffin-embedded (FFPE) test tissues.
- Positive Control Tissues: Use a multi-tissue block (TMA) containing cores from tissues known to express the target (e.g., lymph node for PD-1) [38]. The Ext-PTC should have undergone similar fixation and processing.
- Negative Control Tissues: Use a TMA containing cores from tissues known to lack the target (e.g., kidney, heart for PD-1) [38].
- Consecutive Sections: For NRCs, use a consecutive section from the test block itself.
2. Staining Protocol:
- Deparaffinize and rehydrate the slides.
- Perform antigen retrieval using a method optimized for the target.
- Block endogenous peroxidases and apply a protein block to reduce nonspecific binding.
- For the test slide: Apply the validated primary antibody.
- For the Negative Reagent Control (NRC) slide: Apply a non-immune immunoglobulin of the same isotype and concentration as the primary antibody [36].
- Apply the detection system (e.g., polymer-based system) and chromogen.
- Counterstain, dehydrate, and mount.
3. Interpretation:
- The test slide should show specific staining in the test tissue and the Ext-PTC.
- The NRC slide should show an absence of specific staining, confirming the primary antibody's specificity.
- The Int-PTC, if present, should show appropriate staining.
- Staining patterns should be compared with another antibody against the same target, if available, to strengthen confidence [38].
Comparative Performance Across Assay Platforms
The performance and requirements for control panels can vary significantly across different analytical platforms. The following comparison highlights how control strategies are applied in two common but distinct techniques: the traditional ELISA and the more modern Surface Plasmon Resonance (SPR).
ELISA vs. SPR: A Control Perspective
ELISAs are standard plate-based assays relying on enzyme-linked antibodies for detection, while SPR is a label-free, real-time method that measures binding via changes in refractive index [39].
Table 3: Platform Comparison for Biomolecular Detection and Control Application
| Parameter | ELISA | Surface Plasmon Resonance (SPR) |
|---|---|---|
| Data Measurement | End-point, quantitative (affinity only) | Real-time, quantitative (affinity & kinetics) [39] |
| Label Requirement | Yes (enzyme-conjugated antibody) | No (label-free) [39] |
| Assay Time | Long (>1 day), multiple steps | Short (minutes to hours), streamlined [39] |
| Low-Affinity Interaction Detection | Poor (washed away in steps) | Excellent (real-time monitoring) [39] |
| Positive Control Role | Verify enzyme and detection chemistry | Verify ligand immobilization and system response |
| Negative Control Role | Identify cross-reactivity of antibodies | Identify nonspecific binding to sensor chip |
| Typical Positive Control | Sample with known target concentration | Purified analyte with known kinetics |
| Typical Negative Control | Sample without target / Isotype control | A non-interacting analyte / blank flow cell |
The workflow for these two techniques, from setup to data analysis, differs substantially, as outlined below.
Diagram: Comparative Workflows of ELISA and SPR Assays
Supporting Data from Comparative Studies
Empirical evidence underscores the importance of platform selection and rigorous control. A 2024 study comparing an in-house ELISA with six commercial ELISA kits for detecting anti-Bordetella pertussis antibodies revealed significant variability. The detection of IgA and IgG antibodies at a significant level ranged from 5.0% to 27.0% and 12.0% to 70.0% of patient sera, respectively, across different kits. Furthermore, the results from the commercial kits were consistent for IgG in only 17.5% of cases, highlighting that even with controlled formats, performance can differ dramatically [40]. This variability reinforces the necessity for labs to establish and validate their own control panels tailored to their specific protocols.
Conversely, studies comparing ELISA with SPR demonstrate SPR's superior ability to detect low-affinity interactions. In one investigation, SPR detected a 4% positivity rate for low-affinity anti-drug antibodies (ADAs), compared to only 0.3% by ELISA, showcasing SPR's higher sensitivity for these clinically relevant molecules [39]. This has direct implications for control panel design; validating an assay for low-affinity binders requires controls that can challenge the system's lower detection limits, for which SPR is inherently more suited.
The Scientist's Toolkit: Essential Research Reagent Solutions
A properly equipped laboratory is fundamental to establishing and maintaining a validated control panel. The following table details key reagents and their functions in this process.
Table 4: Essential Research Reagents for Control Panel Establishment
| Reagent / Material | Function in Control Panels | Application Examples |
|---|---|---|
| Validated Cell Lines | Serve as reproducible sources of positive and negative control material. | RAJI (CD19+), JURKAT (CD19-) for flow cytometry [38]. |
| Control Cell Lysates & Nuclear Extracts | Ready-to-use positive controls for Western blot, ensuring lot-to-lot reproducibility. | Rockland's whole-cell lysates or nuclear extracts from specific cell lines or tissues [37]. |
| Tissue Microarrays (TMAs) | Allow simultaneous testing on multiple validated tissues on a single slide for IHC. | TMAs containing lymph node, spleen (positive) and kidney, heart (negative) for PD-1 [38]. |
| Purified Proteins/Peptides | Act as positive controls and standards for quantification in ELISA and Western blot. | Used to verify antibody specificity in a competition assay or generate a standard curve [37]. |
| Loading Control Antibodies | Detect housekeeping proteins to verify equal sample loading in Western blot. | Antibodies against β-actin, GAPDH, or α-tubulin [37]. |
| Isotype Controls | Serve as critical negative reagent controls (NRCs) for techniques like flow cytometry and IHC. | Non-immune mouse IgG2a used when testing with a mouse IgG2a monoclonal antibody [36]. |
| Low Endotoxin Control IgGs | Act as critical controls in sensitive biological assays like neutralization experiments. | Low endotoxin mouse or rabbit IgG to rule out endotoxin effects in cell-based assays [37]. |
The establishment of a validated panel of positive and negative controls is a non-negotiable component of rigorous biomolecular research and diagnostic assay development. It is the linchpin for generating reliable, interpretable, and reproducible data. As demonstrated, a one-size-fits-all approach is ineffective; the panel must be carefully tailored to the specific assay platform, whether it be IHC, Western blot, ELISA, or SPR, and must incorporate a variety of control types—from external and internal positive controls to reagent and tissue negative controls—to comprehensively monitor both sensitivity and specificity. The significant variability observed even among commercial ELISA kits [40] underscores the responsibility of each laboratory to perform its own due diligence in validation. Furthermore, the evolution of analytical techniques like SPR, with its enhanced ability to characterize low-affinity interactions [39], continuously refines the standards for what constitutes adequate experimental control. Ultimately, a robust, well-characterized control panel is not merely a procedural hurdle but a fundamental asset that bolsters scientific confidence, from the research bench to the clinical decision.
Determining the Limit of Detection (LOD) for Analytical Sensitivity
In the context of evaluating specificity and sensitivity in functional assays, determining the Limit of Detection (LOD) is a fundamental requirement for researchers, scientists, and drug development professionals. The LOD represents the lowest amount of an analyte that can be reliably detected by an analytical procedure, establishing the fundamental sensitivity threshold of any bioanalytical method [41]. Within clinical laboratories and diagnostic development, there has historically been a lack of agreement on both terminology and methodology for estimating this critical parameter [42]. This guide objectively compares the predominant approaches for LOD determination, supported by experimental data and standardized protocols, to provide a clear framework for selecting the most appropriate methodology based on specific research needs and regulatory requirements.
The LOD is formally defined as the lowest analyte concentration likely to be reliably distinguished from the Limit of Blank (LoB) and at which detection is feasible [42]. It is crucial to distinguish LOD from related parameters: the Limit of Blank (LoB) describes the highest apparent analyte concentration expected when replicates of a blank sample containing no analyte are tested, while the Limit of Quantitation (LoQ) represents the lowest concentration at which the analyte can not only be detected but also quantified with predefined goals for bias and imprecision [42]. Understanding these distinctions is essential for proper assay characterization, particularly in regulated environments like clinical diagnostics where these performance specifications gauge assay effectiveness during intended use [41].
Core Concepts and Statistical Foundations
The statistical foundation of LOD determination acknowledges that random measurement errors create inherent limitations in detecting elements and compounds at very low concentrations [43]. This reality necessitates a statistical approach to define when an analyte is truly "detected" with reasonable certainty. The LOD is fundamentally a probabilistic measurement, defined as the level at which a measurement has a 95% probability of being greater than zero [44]. This means that while detection below the established LOD is possible, it occurs with lower probability [41].
The core statistical model underlying many LOD approaches assumes a Gaussian distribution of analytical signals. For blank samples, the LoB is calculated as the mean blank signal plus 1.645 times its standard deviation (SD), capturing 95% of the blank distribution [42]. The LOD is then derived by considering both the LoB and the variability of low-concentration samples, typically calculated as LoB + 1.645(SD of low concentration sample) [42]. This statistical framework acknowledges that overlap between analytical responses of blank and low-concentration samples is inevitable, with Type I errors (false positives) occurring when blank samples produce signals above the LoB, and Type II errors (false negatives) occurring when low-concentration samples produce signals below the LoB [42].
Table 1: Key Statistical Parameters in LOD Determination
| Parameter | Definition | Statistical Basis | Typical Calculation |
|---|---|---|---|
| Limit of Blank (LoB) | Highest apparent analyte concentration expected from blank samples | 95th percentile of blank distribution | Meanblank + 1.645(SDblank) |
| Limit of Detection (LOD) | Lowest concentration reliably distinguished from LoB | 95% probability of detection | LoB + 1.645(SD_low concentration sample) |
| Limit of Quantitation (LoQ) | Lowest concentration quantifiable with acceptable precision and bias | Based on predefined bias and imprecision goals | ≥ LOD, determined by meeting precision targets |
| Method Detection Limit (MDL) | Minimum concentration distinguishable from method blanks with 99% confidence | EPA-defined protocol for environmental methods | Based on spiked samples and method blanks |
Comparative Analysis of LOD Determination Methods
Classical Statistical Approach
The classical statistical method, formalized in guidelines like CLSI EP17, utilizes both blank samples and samples with low concentrations of analyte [42]. This approach requires testing a substantial number of replicates—typically 60 for manufacturers establishing these parameters and 20 for laboratories verifying a manufacturer's LOD [42]. The methodology involves measuring replicates of a blank sample to calculate the LoB, then testing replicates of a sample containing a low concentration of analyte to determine the LOD [42]. A key advantage of this method is its standardization and widespread regulatory acceptance. However, a significant limitation is that it may provide underestimated values of LOD and LoQ compared to more contemporary graphical methods [45].
The implementation of this approach follows a specific verification protocol: once a provisional LOD is established, samples containing the LOD concentration are tested to confirm that no more than 5% of values fall below the LoB [42]. If this criterion is not met, the LOD must be re-estimated using a sample of higher concentration [42]. For methods where the assumption of Gaussian distribution is inappropriate, the CLSI guideline provides non-parametric techniques as alternatives [42].
Empirical Probit Regression Method
Probit regression offers an empirical approach to LOD determination that models the relationship between analyte concentration and detection probability [46]. This method involves testing multiple concentrations around the presumed LOD with sufficient replicates to establish a concentration-response relationship for detection frequency. The LOD is typically defined as the concentration corresponding to 95% detection probability [41]. This approach is particularly valuable for binary detection methods like qPCR, where results are often expressed as detected/not detected rather than continuous measurements.
Recent sensitivity analyses reveal that probit regression results are significantly influenced by the number and distribution of tested concentrations [46]. When data sets are restricted but remain centered around the presumed LOD, the estimated LOD tends to lower; when restricted to top-weighted concentrations, the estimated LOD lowers and confidence intervals widen considerably [46]. These findings reinforce recommendations from the Clinical and Laboratory Standards Institute and highlight the need for caution when constrained testing designs are used in LOD estimation [46]. The robustness of this method increases with more concentrations tested across the critical range and with higher replication.
Graphical Validation Approaches
Advanced graphical methods have emerged as powerful alternatives for LOD determination, including uncertainty profiles and accuracy profiles [45]. The uncertainty profile is a decision-making graphical tool that combines uncertainty intervals with acceptability limits, based on tolerance intervals and measurement uncertainty [45]. Similarly, accuracy profiles plot bias and precision expectations across concentrations to visually determine the valid quantification range. These methods provide a more realistic assessment of method capabilities compared to classical statistical approaches [45].
A comparative study implementing these strategies for an HPLC method dedicated to determining sotalol in plasma found that graphical tools provide relevant and realistic assessment, with LOD and LOQ values found by uncertainty and accuracy profiles being in the same order of magnitude [45]. The uncertainty profile method specifically provides precise estimate of the measurement uncertainty, offering additional valuable information for method validation [45]. These graphical strategies represent a reliable alternative to classic concepts for assessment of LOD and LOQ, particularly for methods requiring comprehensive understanding of performance at the detection limit.
EPA Method Detection Limit Procedure
The United States Environmental Protection Agency (EPA) has established a standardized procedure for determining the Method Detection Limit (MDL), designed for a broad variety of physical and chemical methods [47]. The MDL is defined as "the minimum measured concentration of a substance that can be reported with 99% confidence that the measured concentration is distinguishable from method blank results" [47]. The current procedure (Revision 2) uses both method blanks and spiked samples to calculate separate values (MDLb and MDLS), with the final MDL being the higher of the two values [47].
A key feature of the EPA procedure is the requirement that samples used to calculate the MDL are representative of laboratory performance throughout the year rather than from a single date [47]. This approach captures instrument drift and variation in equipment conditions, leading to an MDL that represents actual laboratory practice rather than best-case scenarios [47]. Laboratories must analyze at least seven low-level spiked samples and seven method blanks for one instrument, typically spread over multiple quarters [47].
Table 2: Comparison of LOD Determination Methodologies
| Method | Theoretical Basis | Data Requirements | Advantages | Limitations |
|---|---|---|---|---|
| Classical Statistical (CLSI EP17) | Gaussian distribution of blank and low-concentration samples | 60 replicates for establishment; 20 for verification | Standardized, widely accepted for clinical methods | May provide underestimated values [45] |
| Probit Regression | Concentration-detection probability relationship | Multiple concentrations around presumed LOD with 10-20 replicates each | Directly models detection probability, ideal for binary outputs | Sensitive to concentration selection and distribution [46] |
| Graphical (Uncertainty Profile) | Tolerance intervals and measurement uncertainty | Multiple concentrations across expected range with replication | Provides realistic assessment with uncertainty estimation [45] | More complex implementation and interpretation |
| EPA MDL | 99% confidence distinguishability from blank | 7+ spiked samples and method blanks over time | Represents real-world lab performance over time [47] | Primarily used for environmental applications |
Experimental Protocols for LOD Determination
Standard Protocol for Empirical LOD Determination
For assays such as qPCR, a straightforward empirical approach can be implemented to determine LOD [41]. The protocol begins with creating primary serial dilutions of the target analyte, typically using 1:10 dilution steps spanning from a concentration almost certain to be detected down to one likely below the detection limit [41]. Each dilution is tested in multiple replicates (e.g., triplicate), including appropriate negative controls. Results are tabulated to identify the range where detection becomes inconsistent, followed by a secondary dilution series with smaller steps (e.g., 1:2 dilutions) and more replicates (10-20) within this critical range [41]. The LOD is identified as the lowest concentration where the detection rate is ≥95% [41].
This empirical approach directly measures method performance at critical concentrations and is particularly valuable for methods where theoretical calculations may not capture all practical limitations. The protocol can be enhanced by incorporating multiple reagent lots and instruments to capture expected performance across the typical population of analyzers and reagents, providing a more robust LOD estimate [41].
Statistical Protocol Per CLSI EP17 Guidelines
The standardized statistical protocol involves two distinct phases: first, determining the LoB by testing replicates of a blank sample, then determining the LOD by testing replicates of a sample containing a low concentration of analyte [42]. For the blank sample, the mean and standard deviation are calculated, with LoB defined as meanblank + 1.645(SDblank) assuming a Gaussian distribution [42]. For the low-concentration sample, the LOD is calculated as LoB + 1.645(SD_low concentration sample) [42]. This approach specifically acknowledges and accounts for the statistical reality that some blank samples will produce false positive results (Type I error) while some low-concentration samples will produce false negative results (Type II error) [42].
Probit Regression Implementation
The probit regression protocol requires testing a minimum of 5-7 different analyte concentrations around the presumed LOD, with each concentration tested in a sufficient number of replicates (typically 10-20) to reliably estimate detection probability [46]. The concentrations should be centered around the presumed LOD rather than clustered at higher values, as restricted or top-weighted concentration distributions can lead to underestimated LOD values and widened confidence intervals [46]. The resulting data is analyzed using probit regression to model the relationship between concentration and detection probability, with the LOD typically taken as the concentration corresponding to 95% detection probability. The model fit should be evaluated using appropriate statistical measures like the Akaike information criterion [46].
Visualization of LOD Determination Workflows
LOD Determination Method Selection Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for LOD Experiments
| Reagent/Material | Function in LOD Determination | Application Examples |
|---|---|---|
| Blank Matrix | Provides analyte-free background for LoB determination and sample preparation | Diluent for standard preparation; negative controls [42] |
| Primary Standard | Creates serial dilutions for empirical LOD determination; establishes calibration curve | Cloned amplicon for qPCR LOD; purified analyte for HPLC [41] |
| Internal Standard | Normalizes analytical response and corrects for procedural variability | Atenolol for HPLC determination of sotalol in plasma [45] |
| Reference Materials | Verifies method performance and LOD accuracy; quality control | Certified reference materials with known low concentrations |
| Matrix Modifiers | Mimics sample composition for spiked recovery studies; evaluates matrix effects | Serum, plasma, or tissue extracts for bioanalytical methods |
The determination of LOD for analytical sensitivity requires careful consideration of methodological approaches, each with distinct advantages and limitations. The classical statistical approach provides standardization essential for clinical and diagnostic applications, while empirical probit regression directly models detection probability for binary output methods. Graphical methods like uncertainty profiles offer comprehensive assessment of method validity, and the EPA MDL procedure ensures representativeness of real-world laboratory conditions.
Selection of the appropriate method should consider the analytical technique, regulatory requirements, and intended use of the assay. For regulated clinical diagnostics, the CLSI EP17 approach provides necessary standardization; for research methods requiring comprehensive understanding of performance, graphical methods may be preferable; for environmental applications, the EPA procedure is mandated. Regardless of the method selected, proper experimental design with adequate replication and concentration selection is critical for obtaining accurate, reliable LOD values that truly characterize assay capability at the detection limit.
Designing Cross-Reactivity and Interference Studies for Specificity
In the development of biologics and diagnostics, demonstrating assay specificity is paramount. Specificity refers to the ability of an assay to measure the target analyte accurately and exclusively in the presence of other components that may be expected to be present in the sample matrix [48]. Two of the most significant challenges to assay specificity are cross-reactivity and interference, which, if unaddressed, can compromise data integrity and lead to erroneous conclusions in preclinical and clinical studies [49]. Cross-reactivity occurs when an antibody or receptor binds to non-target analytes that share structural similarities with the intended target [50]. This is primarily due to the nature of antibody-binding sites; a paratope (the antibody's binding region) can bind to unrelated epitopes if they present complementary regions of shape and charge [48]. Interference, a broader challenge, encompasses the effect of any substance in the sample that alters the correct value for the analyte, with matrix effects from complex biological fluids being a predominant concern [49]. A recent industry survey identified matrix interference as the single most important challenge in ligand binding assays for large molecules, cited by 72% of respondents [49]. This guide provides a structured framework for designing rigorous studies to evaluate these parameters, enabling researchers to generate reliable, high-quality data.
Fundamental Concepts and Definitions
A clear understanding of the core concepts is essential for designing robust studies. The following terms form the foundational vocabulary of assay specificity evaluation [48] [49] [50]:
- Specificity: The degree to which an immunoassay differentiates between the target analyte and other non-target components. It measures the immune system's ability to recognize unique antigens.
- Cross-Reactivity: A specific type of interference where the assay reagents (typically antibodies) recognize and bind to analytes that are structurally similar to the target analyte but are not identical. For instance, an antibody might bind to a protein isoform, a precursor, a metabolite, or a related protein from the same family [49] [50].
- Interference: The effect of any substance present in the sample that alters the accurate measurement of the analyte concentration. Sources can be varied and include heterophilic antibodies, rheumatoid factors, complement, hemolyzed blood lipids, and concomitant medications [49].
- Epitope: The specific region (approximately 15 amino acids) on the surface of an antigen that is recognized and bound by an antibody. Only about 5 of these amino acids typically contribute most of the binding energy [48].
- Paratope: The part of the antibody molecule (also comprising about 15 amino acids) that binds to the epitope. A single paratope can, under certain conditions, bind to multiple, unrelated epitopes [48].
- Analyte: The substance or chemical constituent that is being measured in an assay.
The relationship between specificity and cross-reactivity is often a function of binding affinity and assay conditions. Under poor binding conditions, even low-affinity binding can be highly specific, as only the strongest complementary partners form detectable bonds. Conversely, under favorable binding conditions, low-affinity binding can develop a broader set of complementary partners, leading to increased cross-reactivity and reduced specificity [48].
Comparative Analysis of Specificity Assessment Approaches
Different methodologies are employed to investigate cross-reactivity and interference, each with distinct strengths, applications, and data outputs. The choice of approach depends on the stage of development, the resources available, and the required level of specificity.
Table 1: Comparison of Specificity and Cross-Reactivity Assessment Methods
| Method | Primary Application | Key Measured Outputs | Pros | Cons |
|---|---|---|---|---|
| Response Curve Comparison [50] | Quantifying cross-reactivity of structurally similar analytes. | Half-maximal response (IC50); Percent Cross-Reactivity. | Provides a quantitative measure of cross-reactivity; Allows for parallel curve analysis to confirm similar binding mechanics. | Less effective for assessing non-specific matrix interference; Requires pure preparations of cross-reactive analytes. |
| Spiked Specimen Measurement [50] | Validating specificity in a clinically relevant matrix. | Measured concentration vs. expected concentration; Percent Recovery. | Tests specificity in the actual sample matrix (e.g., serum, plasma); Clinically translatable results. | Percent cross-reactivity may not be constant across all concentration levels; Risk of misinterpreting if spiked concentrations are not clinically relevant. |
| Parallelism / Linearity of Dilution [49] | Detecting matrix interference. | Observed concentration vs. sample dilution; Linear regression fit. | Identifies the presence of interfering substances in the matrix; Confirms assay suitability for the given sample type. | Does not identify the specific interfering substance; May require large sample volumes if not miniaturized. |
| Miniaturized Flow-Through Immunoassay [49] | Reducing interference and reagent use in routine testing. | Analyte concentration; Coefficient of Variation (CV). | Dramatically reduces matrix contact time, minimizing interference; Consumes minimal sample and reagents. | Requires specialized equipment (e.g., Gyrolab platform); May have higher initial setup costs. |
The data generated from these methods is critical for regulatory submissions and internal decision-making. For cross-reactivity studies using response curve comparison, the result is expressed as a percentage, calculated as: (Concentration of target analyte at 50% B/MAX) / (Concentration of cross-reactant at 50% B/MAX) * 100 [50]. A lower percentage indicates higher specificity. For interference and recovery studies, the result is expressed as Percent Recovery: (Measured Concentration / Expected Concentration) * 100. Acceptable recovery typically falls within 80-120%, depending on the assay and regulatory guidelines.
Experimental Protocols for Specificity Testing
Protocol for Cross-Reactivity Assessment via Response Curve Comparison
This protocol provides a step-by-step method to quantitatively determine the degree of cross-reactivity for related substances [50].
1. Principle: A dose-response curve for the target analyte is generated and compared to the curve of a potential cross-reactant. The ratio of concentrations needed to achieve the same response (e.g., half-maximal) determines the percent cross-reactivity.
2. Materials:
- Reference standard of the target analyte.
- Purified cross-reactive analytes (e.g., metabolites, isoforms, related proteins).
- Assay buffer.
- Appropriate biological matrix (e.g., stripped serum).
- Validated immunoassay kit or reagents.
3. Procedure: a. Prepare a calibration curve by spiking the target analyte into the appropriate matrix across a wide concentration range (e.g., 8-12 points). b. For each potential cross-reactant, prepare a separate dose-response curve in the same matrix, covering a concentration range expected to generate a full response. c. Run all curves in the same assay run to minimize inter-assay variability. d. Plot the dose-response curves for the target and all cross-reactants.
4. Data Analysis:
a. Determine the concentration of each substance that produces the half-maximal response (50% B/MAX).
b. Calculate the percent cross-reactivity for each cross-reactant using the formula:
% Cross-Reactivity = [IC50 (Target Analyte) / IC50 (Cross-Reactant)] * 100
5. Interpretation: A cross-reactivity of 100% indicates equal recognition. A value of 1% suggests the cross-reactant is 100 times less potent than the target. Values below 0.1% are generally considered negligible, but this threshold is context-dependent [50].
Protocol for Interference Assessment via Spiked Recovery and Parallelism
This protocol evaluates the impact of the sample matrix and other potential interferents on assay accuracy [49] [50].
1. Principle: The target analyte is spiked into the sample matrix at multiple concentrations. The measured values are compared to the expected values to calculate percent recovery. Parallelism tests the linearity of sample dilution.
2. Materials:
- Patient or test samples with known and unknown backgrounds.
- High-purity analyte stock solutions.
- Assay buffers and reagents.
3. Procedure for Spiked Recovery: a. Select a minimum of 3 different native samples (e.g., from different donors) with low endogenous analyte levels. b. Spike each sample with the target analyte at 3-4 different concentrations across the assay's dynamic range. c. Also, prepare the same spike concentrations in a clean, ideal solution (e.g., buffer) to serve as a control. d. Assay all samples and controls. e. Calculate the recovery for each spike level in each matrix.
4. Procedure for Parallelism: a. Select a minimum of 3 patient samples with a high endogenous level of the analyte. b. Serially dilute these samples (e.g., 1:2, 1:4, 1:8) using the appropriate assay buffer or stripped matrix. c. Assay the diluted samples. d. Plot the observed concentration against the dilution factor.
5. Data Analysis:
a. Recovery: % Recovery = (Measured Concentration in Spiked Sample - Measured Concentration in Native Sample) / Spiked Concentration * 100
b. Parallelism: Perform linear regression analysis. The dilutions should produce a linear plot with a y-intercept near zero. Significant deviation from linearity indicates matrix interference.
Visualization of Experimental Workflows
To clarify the logical sequence of these experiments, the following diagrams outline the core workflows.
Diagram 1: Specificity Study Workflow
Diagram 2: Cross-Reactivity Calculation
The Scientist's Toolkit: Key Reagents and Materials
The reliability of specificity studies hinges on the quality and appropriateness of the materials used. The following table details essential reagents and their critical functions in developing and validating a robust immunoassay.
Table 2: Essential Research Reagent Solutions for Specificity Testing
| Reagent / Material | Function & Role in Specificity | Key Considerations for Selection |
|---|---|---|
| Monoclonal Antibodies (mAb) | Recognize a single, specific epitope on the target antigen. Used primarily for capture to establish high assay specificity [49]. | High affinity and specificity for the target epitope. Low lot-to-lot variability. Must be screened for non-target binding [49]. |
| Polyclonal Antibodies (pAb) | A mixture of antibodies that recognize multiple epitopes on a single antigen. Often used for detection to increase sensitivity [49]. | Can provide higher sensitivity but may have a higher risk of cross-reactivity. Should be affinity-purified [49]. |
| Stripped / Surrogate Matrix | A matrix (e.g., serum, plasma) depleted of the endogenous analyte. Used to prepare calibration standards and quality controls for recovery experiments [50]. | The stripping process should not alter other matrix components. Charcoal-stripped serum is common. A surrogate (e.g., buffer with BSA) may be used but must be validated. |
| Pure Cross-Reactive Analytes | Metabolites, isoforms, precursors, or structurally similar proteins used to challenge the assay and quantify cross-reactivity [50]. | Should be of high purity and well-characterized. The selection should be based on the biological context and likelihood of presence in study samples. |
| Blocking Agents | Substances (e.g., animal serums, irrelevant IgG, proprietary blockers) added to the assay buffer to reduce non-specific binding and matrix interference [49]. | Must effectively block interference without affecting the specific antibody-antigen interaction. Requires optimization for each assay format. |
| Miniaturized Flow-Through Systems | Platforms (e.g., Gyrolab) that use microfluidics to process nanoliter volumes, reducing reagent consumption and minimizing matrix interference through short contact times [49]. | Reduces sample and reagent consumption by 50-80%. The flow-through design favors high-affinity interactions, reducing low-affinity interference [49]. |
Designing comprehensive cross-reactivity and interference studies is a critical component of functional assay development. By implementing the structured protocols and comparative approaches outlined in this guide—ranging from quantitative response curve analyses to spike-and-recovery experiments in relevant matrices—researchers can systematically identify and mitigate risks to assay specificity. The choice of high-quality reagents, particularly the strategic use of monoclonal and polyclonal antibodies, is fundamental to success. Furthermore, leveraging modern technological solutions like miniaturized flow-through systems can provide a practical path to achieving robust, specific, and reliable data, thereby de-risking the drug development pipeline from discovery through clinical stages. A rigorously validated assay, proven to be specific and free from meaningful interference, forms the bedrock of trustworthy scientific and regulatory decision-making.
Best Practices for Sample Sizing and Replication in Validation Studies
In the field of specificity and sensitivity functional assays research, the reliability of study findings hinges on two pillars: a sample size large enough to yield precise performance estimates and a robust strategy for replicating results. Validation studies with inadequate sample sizes increase uncertainty and limit the interpretability of findings, raising the likelihood that these findings may be disproved in future studies [51]. Furthermore, understanding the distinction between replication—confirming results in an independent setup—and validation—often performed by the same group with different data or technology—is critical for establishing credible evidence [52] [53]. This guide outlines best practices for designing validation studies that produce reliable, reproducible, and actionable results for drug development.
Statistical Foundations for Sample Sizing
Justifying the sample size in a validation study is a fundamental step that moves beyond "convenience samples." The sample must be large enough to precisely estimate the key performance measures of interest, such as sensitivity, specificity, and predictive values [51] [54].
Core Sample Size Calculation Criteria
Current comprehensive guidance for evaluating prediction models with binary outcomes suggests calculating sample size based on three primary criteria to ensure precise estimation of calibration, discrimination, and net benefit [54]. These should form the initial stage of sample size determination.
Criterion 1: Sample Size for a Precise Observed/Expected (O/E) Ratio. This measures calibration, or the agreement between predicted and observed event rates. The formula is:
- ( N = \frac{1-\varnothing }{\varnothing {\left(SE\left(\text{ln}\left(\frac{O}{E}\right)\right)\right)}^{2}} )
- Here, ( \varnothing ) is the assumed true outcome prevalence, and ( SE\left(\text{ln}\left(\frac{O}{E}\right)\right) ) is the target standard error for the log of the O/E ratio [54].
Criterion 2: Sample Size for a Precise Calibration Slope (β). The calibration slope assesses how well the model's predictions match observed outcomes across their range. The formula is:
- ( N = \frac{{I}{\alpha }}{SE{\left(\beta \right)}^{2}\left({I}{\alpha }{I}{\beta }-{I}{\alpha \beta }^{2}\right)} )
- Here, ( SE(\beta ) ) is the target standard error for the slope, and the ( I ) terms are elements of Fisher’s information matrix derived from the linear predictor distribution in the evaluation population [54].
Criterion 3: Sample Size for a Precise C-statistic. The c-statistic (or AUC) measures the model's ability to discriminate between those with and without the outcome. The standard error formula, which makes no distributional assumptions, is:
- ( SE\left(C\right)=\sqrt{\frac{C\left(1-C\right)\left(1+\left(\frac{N}{2}-1\right)\left(\frac{1-C}{2-C}\right)+\frac{\left(\frac{N}{2}-1\right)C}{1+C}\right)}{{N}^{2}\varnothing \left(1-\varnothing \right)}} )
- Here, ( C ) is the anticipated true c-statistic in the evaluation population [54].
Extended Criteria for Threshold-Based Performance Measures
When a clinical threshold is used for classification, which is common in functional assays, additional performance measures like sensitivity and specificity are reported. Sample size calculations should be extended to ensure these are also precisely estimated [54]. The required sample size can be derived by setting a target standard error or confidence interval width for each measure, using their known standard error formulae. For a binary outcome, these standard errors are [54]:
- Sensitivity (Recall) & Specificity: ( SE = \sqrt{\frac{ p (1 - p) }{ n } } ), where ( p ) is the expected sensitivity (or specificity) and ( n ) is the number of true positives (for sensitivity) or true negatives (for specificity).
- Positive Predictive Value (PPV/Precision) & Negative Predictive Value (NPV): ( SE = \sqrt{\frac{ PPV (1 - PPV) }{ n{pos} } } ), where ( n{pos} ) is the number of positive predictions (for PPV). The formula for NPV is analogous, using ( n_{neg} ).
- F1-Score: An iterative method is required to estimate the sample size needed for a sufficiently precise estimate of the F1-score, which is the harmonic mean of precision and recall [54].
A pragmatic perspective can be gained by reviewing accepted practice. An analysis of 1,750 scale-validation articles published in 2021 found that after removing extreme outliers, mean sample sizes varied, often being higher for studies involving students and lower for those involving patients [55]. This highlights the context-dependent nature of sample size selection.
Table 1: Summary of Key Sample Size Formulae for Validation Studies
| Performance Measure | Formula / Approach | Key Parameters |
|---|---|---|
| Observed/Expected (O/E) Ratio | ( N = \frac{1-\varnothing }{\varnothing {\left(SE\left(\text{ln}\left(\frac{O}{E}\right)\right)\right)}^{2}} ) | Outcome prevalence (( \varnothing )), target standard error for ln(O/E) |
| Calibration Slope (β) | ( N = \frac{{I}{\alpha }}{SE{\left(\beta \right)}^{2}\left({I}{\alpha }{I}{\beta }-{I}{\alpha \beta }^{2}\right)} ) | Target standard error for slope (( SE(\beta ) )), linear predictor distribution |
| C-Statistic (AUC) | ( SE\left(C\right)=\sqrt{\frac{C(1-C)(1+(\frac{N}{2}-1)\frac{1-C}{2-C}+\frac{(\frac{N}{2}-1)C}{1+C})}{{N}^{2}\varnothing (1-\varnothing )}} ) | Anticipated C-statistic (( C )), outcome prevalence (( \varnothing )) |
| Sensitivity & Specificity | ( SE = \sqrt{\frac{ p (1 - p) }{ n } } ) | Expected sensitivity/specificity (( p )), number of true positives/negatives (( n )) |
| PPV & NPV | ( SE = \sqrt{\frac{ PPV (1 - PPV) }{ n_{pos} } } ) | Expected PPV/NPV, number of positive/negative predictions (( n{pos} ), ( n{neg} )) |
| F1-Score | Iterative computational method | Target standard error, expected precision and recall |
Experimental Protocols for Validation
A robust validation protocol ensures that the estimated performance measures are reliable and generalizable.
Detailed Methodology for a Functional Assay Validation Study
The following protocol provides a framework for validating a functional assay, incorporating best practices for sample sizing and replication.
Pre-Validation Power Analysis:
- Define the primary performance measure for your assay (e.g., Sensitivity).
- Specify the expected value for this measure (e.g., 0.85) and the desired confidence interval width (e.g., ± 0.05).
- Using the appropriate standard error formula, calculate the minimum number of required positive and negative samples needed to achieve the desired precision. The largest sample size calculated from all relevant measures (including the core criteria) should be adopted [54].
Sample Cohort Definition:
- Enroll participants or samples that are representative of the target population in which the assay is intended to be used.
- Ensure the cohort is independent from any data used during the assay's development phase to ensure a true external validation [54].
- Apply pre-defined inclusion and exclusion criteria consistently.
Blinded Data Generation:
- Conduct the functional assay experiments such that the technicians are blinded to the reference standard outcomes (ground truth).
- This prevents conscious or unconscious bias in the interpretation of the assay results.
Replication Analysis:
- Technical Replication: Perform repeat measurements of a subset of samples within the same laboratory to assess intra-assay variability.
- Independent Replication: If possible, have a subset of samples analyzed by a separate, independent laboratory. This is the gold standard for establishing the robustness of findings [52] [53].
Statistical Analysis and Performance Calculation:
- Compare the assay results against the reference standard to create a 2x2 contingency table.
- Calculate all relevant performance metrics: Sensitivity, Specificity, PPV, NPV, Accuracy, and F1-Score.
- Report confidence intervals (e.g., 95% CI) for all metrics to convey the uncertainty of the estimates, as dictated by the sample size.
Research Reagent Solutions for Robust Validation
The reliability of a validation study is also dependent on the quality and consistency of the materials used.
Table 2: Essential Materials for Functional Assay Validation
| Research Reagent / Material | Critical Function in Validation |
|---|---|
| Well-Characterized Biobank Samples | Provides a standardized set of positive and negative controls with known ground truth, essential for calculating sensitivity and specificity across batches. |
| Reference Standard Materials | Serves as the gold standard against which the new assay is compared; its accuracy is paramount for a valid study. |
| Calibrators and Controls | Ensures the assay is operating within its specified parameters and allows for normalization of results across different runs and days. |
| Blinded Sample Panels | A panel of samples with known status, provided to the testing team without identifiers, is crucial for an unbiased assessment of assay performance. |
Workflow and Relationship Diagrams
The following diagrams illustrate the key logical relationships and workflows in validation study design.
Figure 1: Validation Study Workflow. This diagram outlines the sequential steps for conducting a robust validation study, from initial design to final reporting.
Figure 2: Concepts of Validation vs. Replication. This chart clarifies the distinct meanings of validation and independent replication in research studies [52] [53].
The credibility of specificity and sensitivity functional assays in drug development is non-negotiable. By implementing statistically justified sample sizes—calculated to precisely estimate both core and threshold-based performance measures—and by adhering to rigorous experimental protocols that include independent replication, researchers can significantly enhance the reliability and interpretability of their validation studies. This rigorous approach ensures that predictive models and assays brought into the development pipeline are built upon a foundation of robust, replicable evidence.
The evaluation of specificity and sensitivity forms the cornerstone of functional assay research, guiding the selection of appropriate methodologies across diverse biomedical applications. As research and drug development grow increasingly complex, the strategic choice between cell-based, molecular (PCR), and immunoassay techniques becomes critical. Each platform offers distinct advantages and limitations in quantifying biological responses, detecting pathogens, and profiling proteins. This guide provides an objective, data-driven comparison of these methodologies through recent case studies, experimental data, and detailed protocols to inform researchers and drug development professionals in their assay selection and implementation.
Comparative Analysis of Assay Platforms: Key Characteristics
The table below summarizes the core functional principles, strengths, and limitations of cell-based, molecular (PCR), and immunoassay platforms, providing a foundational comparison for researchers.
Table 1: Core Characteristics of Major Assay Platforms
| Assay Platform | Primary Function & Target | Key Strengths | Inherent Limitations |
|---|---|---|---|
| Cell-Based Assays | Analyzes cellular responses (viability, signaling) using live cells [56] | Provides physiologically relevant data; crucial for drug efficacy and toxicity screening [57] [56] | High cost and technical complexity; potential for variable results [56] |
| Molecular Assays (PCR/dPCR) | Detects and quantifies specific nucleic acid sequences (DNA/RNA) [58] | High sensitivity and specificity; absolute quantification without standard curves (dPCR) [59] [58] | Requires specialized equipment; higher cost than immunoassays; complex sample handling [59] [58] |
| Immunoassays | Measures specific proteins or antigens using antibody-antigen binding [58] | High specificity; rapid results; ideal for routine diagnostics and point-of-care testing [58] | Generally lower sensitivity than PCR; may miss early-stage infections [58] |
Case Study 1: Cell-Based Assays in Drug Discovery
Experimental Context and Protocol
Cell-based assays are indispensable in drug discovery for studying complex cellular phenotypes and mechanisms of action within a physiological context [57]. A typical protocol involves:
- Cell Culture: Maintaining relevant cell lines (e.g., primary cells, stem cell-derived models) under controlled conditions.
- Treatment: Exposing cells to chemical compounds, biological agents, or candidate therapeutics.
- Incubation: Allowing sufficient time for cellular response, which can range from hours to days.
- Signal Detection: Measuring specific outputs using reagents designed to report on viability, proliferation, apoptosis, or pathway activation via fluorescence, luminescence, or absorbance.
- Data Analysis: Processing raw data to determine IC50/EC50 values, efficacy, and toxicity.
Advanced trends include the use of 3D cell cultures, organ-on-a-chip systems, and integration with high-throughput screening (HTS) automation and AI-driven image analysis to enhance physiological relevance and data output [57] [56].
Performance and Market Outlook
The critical role of these assays is reflected in the market, which is projected to grow from USD 20.96 billion in 2025 to approximately USD 45.16 billion by 2034, at a compound annual growth rate (CAGR) of 8.9% [56]. This growth is primarily driven by escalating drug discovery efforts and the demand for more predictive preclinical models. A key development is the U.S. FDA's pilot program allowing human cell-based assays to replace animal testing for antibody therapies, accelerating drug development and improving predictive accuracy [56].
Case Study 2: Molecular Assays for Pathogen Detection
Experimental Protocol: Digital PCR vs. Real-Time RT-PCR
Molecular assays, particularly PCR-based methods, are the gold standard for pathogen detection due to their high sensitivity [59] [60]. The following workflow outlines a comparative diagnostic evaluation between digital PCR (dPCR) and Real-Time RT-PCR.
Diagram 1: dPCR vs RT-PCR workflow
Performance Data: Sensitivity and Precision
A 2025 study compared dPCR and Real-Time RT-PCR for detecting major respiratory viruses (Influenza A/B, RSV, SARS-CoV-2) across 123 samples stratified by viral load [59].
Table 2: Performance Comparison of dPCR vs. Real-Time RT-PCR [59]
| Virus Category | Viral Load (by Ct Value) | Platform Performance Findings |
|---|---|---|
| Influenza A | High (Ct ≤ 25) | dPCR demonstrated superior accuracy over Real-Time RT-PCR |
| Influenza B | High (Ct ≤ 25) | dPCR demonstrated superior accuracy over Real-Time RT-PCR |
| SARS-CoV-2 | High (Ct ≤ 25) | dPCR demonstrated superior accuracy over Real-Time RT-PCR |
| RSV | Medium (Ct 25.1-30) | dPCR demonstrated superior accuracy over Real-Time RT-PCR |
| All Viruses | Medium & Low Loads | dPCR showed greater consistency and precision in quantification |
The study concluded that dPCR offers absolute quantification without standard curves, reducing variability and improving diagnostic accuracy, particularly for intermediate viral levels. However, its routine use is currently limited by higher costs and less automation compared to Real-Time RT-PCR [59].
Comparative Detection: PCR vs. Culture
Another 2025 study on wound infections compared real-time PCR to traditional culture, revealing PCR's enhanced detection capability [61]. When referenced against culture, PCR showed a sensitivity of 98.3% and a specificity of 73.5%. However, advanced statistical analysis estimated PCR's true specificity at 91%, suggesting that culture, as the reference method, suffers from significant underdetection. The PCR assay detected 110 clinically significant pathogens that were missed or ambiguously reported by culture, highlighting its value in diagnosing complex, polymicrobial infections [61].
Case Study 3: Multiplex Immunoassays for Biomarker Analysis
Experimental Protocol: Comparing Immunoassay Platforms
Multiplex immunoassays enable the simultaneous measurement of multiple protein biomarkers from a single sample, which is invaluable for profiling complex diseases. A 2025 study directly compared three platforms—Meso Scale Discovery (MSD), NULISA, and Olink—for analyzing inflammatory proteins in stratum corneum tape strips (SCTS), a challenging sample type with low protein yield [62].
- Sample Collection: SCTS were collected from patients with hand dermatitis and from patch-test reactions (allergens and irritants).
- Sample Preparation: Proteins were extracted from the tape strips using phosphate-buffered saline with Tween 20 and sonication.
- Multiplex Analysis: The same extracts were analyzed on the MSD, NULISA, and Olink platforms, focusing on 30 shared proteins.
- Data Processing: Proteins were considered detectable if >50% of samples exceeded the platform's specific detection limit. Correlation and differential expression between healthy and dermatitis-affected skin were assessed.
Performance Data: Detectability and Concordance
The study provided clear data on the performance of the three immunoassay platforms in a challenging sample matrix [62].
Table 3: Platform Performance in Stratum Corneum Tape Strips [62]
| Immunoassay Platform | Detectability of Shared Proteins | Key Differentiating Features |
|---|---|---|
| Meso Scale Discovery (MSD) | 70% (Highest sensitivity) | Provided absolute protein concentrations, enabling normalization. |
| NULISA | 30% | Required smaller sample volumes and fewer assay runs. |
| Olink | 16.7% | Required smaller sample volumes and fewer assay runs. |
Despite differences in detectability, the platforms showed strong biological concordance. Four proteins (CXCL8, VEGFA, IL18, CCL2) were detected by all three and showed similar differential expression patterns between control and dermatitis-affected skin [62]. This underscores that while sensitivity varies, the biological conclusions can be consistent across well-validated platforms.
The Scientist's Toolkit: Essential Research Reagent Solutions
Selecting the appropriate reagents and tools is fundamental to the success of any assay. The following table details key solutions used across the featured methodologies.
Table 4: Essential Reagents and Materials for Assay Development
| Item Name | Function / Application | Example Use-Case |
|---|---|---|
| Assay Kits & Reagents | Pre-designed solutions for analyzing cellular processes (viability, apoptosis) or detecting targets (antigens, DNA) [57] [56]. | Streamlined workflow in cell-based screening and diagnostic immunoassays [56]. |
| Cell Lines & Culture Media | Provides the living system for cell-based assays, supporting growth and maintenance [57]. | Drug efficacy and toxicity testing in physiologically relevant models [57] [56]. |
| Primers & Probes | Target-specific sequences for amplifying and detecting nucleic acids in PCR/dPCR [59]. | Absolute quantification of viral RNA in respiratory pathogen panels [59]. |
| Validated Antibodies | Key binders for detecting specific proteins (antigens) in immunoassays [62] [58]. | Protein biomarker detection and quantification in multiplex panels (MSD, NULISA, Olink) [62]. |
| Automated Nucleic Acid Extractors | Isolate pure DNA/RNA from complex biological samples for molecular assays [59]. | High-throughput RNA extraction for SARS-CoV-2 RT-PCR testing [59] [60]. |
Strategic Workflow: Selecting the Right Assay
The choice between assay types is dictated by the research question, target analyte, and required performance characteristics. The following decision pathway provides a logical framework for selection.
Diagram 2: Assay selection workflow
The strategic application of cell-based, PCR, and immunoassays is fundamental to advancing biomedical research and drug development. As evidenced by the case studies, the optimal methodological choice is context-dependent. Cell-based assays provide unrivaled physiological relevance for functional analysis. Molecular assays (PCR/dPCR) deliver maximum sensitivity and precision for nucleic acid detection and quantification. Immunoassays offer speed, specificity, and practicality for protein detection, especially in clinical and point-of-care settings. The ongoing integration of automation, AI, and novel biological models like 3D cultures is enhancing the throughput, predictive power, and reproducibility of all these platforms. By understanding the comparative performance, operational workflows, and specific reagent requirements of each method, scientists can make informed decisions that robustly support their research objectives within the critical framework of specificity and sensitivity evaluation.
Enhancing Performance: Strategies to Overcome Common Assay Pitfalls
In the rigorous world of drug development and clinical research, the accurate interpretation of experimental data is paramount. The concepts of false positives and false negatives are central to this challenge. A false positive occurs when a test incorrectly indicates the presence of a condition, such as a disease or a treatment effect, when it is not actually present. Conversely, a false negative occurs when a test fails to detect a condition that is truly present [16]. For researchers and scientists, the management of these errors is not merely a statistical exercise; it directly impacts the safety and efficacy of therapeutic interventions, influences clinical decision-making, and ensures the responsible allocation of research resources [63]. This guide provides an objective comparison of methodologies designed to quantify and mitigate these errors, framed within the critical context of evaluating specificity and sensitivity in functional assays.
Core Concepts: Error Types and Their Implications
In statistical hypothesis testing, false positives are analogous to Type I errors (denoted by the Greek letter α), while false negatives are analogous to Type II errors (denoted by β) [16]. The rates of these errors are inversely related to fundamental metrics of test performance:
- Sensitivity (or the power of a test): Calculated as 1 - β, it represents the probability of correctly identifying a true positive effect [16].
- Specificity: Calculated as 1 - α, it represents the probability of correctly identifying a true negative result [16].
A critical challenge in research is the misinterpretation of p-values. A p-value of 0.05 does not equate to a 5% false positive rate. The actual False Positive Risk (FPR) can be much higher, depending on the prior probability of the hypothesis being true. For instance, even an observation of p = 0.001 may still carry an FPR of 8% if the prior probability of a real effect is only 10% [16]. This highlights the necessity of considering pre-experimental plausibility alongside statistical results.
Comparative Analysis of Reliable Change Methodologies
In pre-post study designs common in clinical and pharmacological research, distinguishing random fluctuations from substantive change is crucial. Distribution-based methods, which rely on the statistical properties of data, are often employed for this purpose [63]. The following section compares two prominent methods for assessing individual reliable change.
The Contenders: Jacobson-Truax vs. Hageman-Arrindell
Jacobson-Truax Reliable Change Index (RCI): This is the most widely cited method for assessing individual change in pre-post designs [63]. It calculates the difference between an individual's pre-test (
Xi) and post-test (Yi) scores, standardized by the standard error of the difference. Formula:RCI = (Xi - Yi) / √[2(Sx√(1-Rxx))²]whereSxis the pre-test standard deviation andRxxis the test's reliability [63].Hageman-Arrindell (HA) Approach: This method was proposed as a more sophisticated alternative to the RCI. Its key innovation is the incorporation of the reliability of the pre-post differences (
RDD), which addresses psychometric controversies surrounding difference scores [63]. Formula:HA = { (Yi - Xi)RDD + (My - Mx)(1 - RDD) } / √[2RDD(Sx√(1-Rxx))²]whereMxandMyare the pre- and post-test means [63].
Experimental Performance Data
Simulation studies using pre-post designs have been conducted to evaluate the false positive and false negative rates of these two methods. The results are summarized in the table below.
Table 1: Performance Comparison of RCI and HA Methods in Simulated Pre-Post Studies
| Performance Metric | Jacobson-Truax (RCI) | Hageman-Arrindell (HA) | Interpretation |
|---|---|---|---|
| False Positive Rate | Unacceptably high (5.0% to 39.7%) [63] | Acceptable results [63] | HA demonstrates superior control over Type I errors. |
| False Negative Rate | Acceptable when using stringent effect size criteria [63] | Similar to RCI, acceptable with stringent criteria [63] | Both methods perform comparably in controlling Type II errors. |
| Overall Conservatism | Less conservative, identifies more changes [63] | More conservative, identifies fewer changes [63] | HA's conservatism leads to fewer false positives. |
Experimental Protocol for Method Comparison
The comparative data in Table 1 were derived from a specific simulation methodology that can be replicated for validating assays:
- Study Design: A pre-post test design is simulated, where a measurement is taken before and after a hypothetical intervention in the same group of subjects [63].
- Data Simulation: Researchers generate datasets under two primary conditions:
- No True Change Scenario: Data are simulated where any observed pre-post difference is due to random variation alone. This setup is used to estimate the false positive rate.
- True Change Scenario: Data are simulated with a systematic, true effect added to the post-test scores. This setup is used to estimate the false negative rate.
- Parameter Manipulation: Key variables such as sample size, effect size magnitude (using both conventional Cohen's criteria and more stringent Ferguson's criteria), and test reliability are systematically varied across simulations.
- Classification & Analysis: For each simulated dataset, both the RCI and HA indices are calculated for every "subject." The proportions of false positives and false negatives are then tallied and compared across the two methods [63].
Visualizing the Assessment of Reliable Change
The following diagram illustrates the logical workflow for applying these methods to determine reliable change in a research setting.
Diagram: Workflow for Reliable Change Assessment
The Scientist's Toolkit: Essential Reagents & Materials
The following table details key solutions and materials required for implementing the experimental protocols discussed, particularly in the context of clinical or biomarker research.
Table 2: Essential Research Reagent Solutions for Functional Assays
| Reagent/Material | Function/Brief Explanation |
|---|---|
| Validated Questionnaires/Biomarker Assays | Standardized tools (e.g., GAD-7 for anxiety) or immunoassays with known psychometric/properties (reliability Rxx, sensitivity, specificity) to ensure consistent measurement of the target construct [63]. |
| Statistical Computing Environment | Software such as R (with ggplot2 for visualization) or Python with specialized libraries (e.g., scikit-learn) for performing complex calculations like RCI/HA and running simulation studies [64]. |
| Reference Standard Samples | For biomarker assays, well-characterized positive and negative control samples are essential for validating test accuracy, calibrating equipment, and calculating sensitivity/specificity daily [65]. |
| CT Imaging & Analysis Software | In disease phenotyping research (e.g., COPD), CT scans provide an objective, quantitative "gold standard" (like emphysema burden) against which the sensitivity and specificity of functional parameters are validated [65]. |
| Simulation Code Scripts | Custom or pre-validated scripts (e.g., Excel macro for HA calculation) to automate the data generation and classification processes in simulation studies, ensuring reproducibility and reducing manual error [63]. |
The choice between the Jacobson-Truax RCI and the Hageman-Arrindell methods represents a critical trade-off between sensitivity and specificity in identifying reliable change. The RCI, while more popular and simpler to compute, carries a significantly higher risk of false positives, which could lead to erroneously declaring an ineffective treatment as successful. The HA method, by incorporating the reliability of pre-post differences, provides more robust control against Type I errors, making it a more conservative and often more prudent choice for rigorous research settings. For scientists and drug development professionals, mitigating sources of error requires a deliberate methodological selection. When the cost of a false positive is high—such as in late-stage clinical trials or safety evaluations—opting for the more conservative HA approach is strongly recommended. This decision, grounded in an understanding of the underlying statistical performance data, ensures that the conclusions drawn from functional assays and clinical studies are both valid and reliable.
The Impact of Reagent Quality and Lot-to-Lot Variability
For researchers, scientists, and drug development professionals, the integrity of biological reagents is a foundational element that underpins the reliability of all experimental data. Reagent quality and consistency are paramount, directly influencing the specificity, sensitivity, and reproducibility of functional assays. Among the most significant yet often underestimated challenges is lot-to-lot variation (LTLV), a form of analytical variability introduced when transitioning between different production batches of reagents and calibrators [66] [67].
This variation is not merely a statistical nuisance; it carries substantial clinical and research consequences. Instances of undetected LTLV have led to misdiagnoses, such as erroneous HbA1c results affecting diabetes diagnoses and falsely elevated PSA results causing undue patient concern [66]. In the research context, particularly in regulated bioanalysis, such variability can delay preclinical and clinical studies, resulting in significant losses of time, money, and reputation [68]. This guide provides a comparative analysis of how reagent quality and LTLV impact assay performance, offering detailed protocols and data to empower professionals in making informed decisions.
Fundamental Causes of Lot-to-Lot Variation
Lot-to-lot variability arises from a confluence of factors, primarily rooted in the inherent biological nature of the raw materials and the complexities of the manufacturing process. It is estimated that 70% of an immunoassay's performance is determined by the quality of its raw materials, while the remaining 30% is ascribed to the production process [67].
The table below summarizes the key reagents and the specific quality fluctuations that lead to LTLV.
Table 1: Key Reagents and Their Associated Causes of Lot-to-Lot Variation
| Reagent Type | Specifications Leading to LTLV |
|---|---|
| Antigens/Antibodies | Unclear appearance, low storage concentration, high aggregate, low purity, inappropriate storage buffer [67]. |
| Enzymes (e.g., HRP, ALP) | Inconsistent enzymatic activity between batches, presence of unknown interfering impurities [67]. |
| Conjugates | Unclear appearance, low concentration, low purity [67]. |
| Kit Controls & Calibrators | The use of the same materials for both controls and calibrators; instability of master calibrators [67]. |
| Buffers/Diluents | Not mixed thoroughly, resulting in pH and conductivity deviation [67]. |
A critical example involves antibodies, which are prone to aggregation, particularly at high concentrations. These aggregates, fragments, and unpaired chains can cause high background noise, signal leap, and ultimately, inaccurate analyte concentration readings [67]. Furthermore, even with identical amino acid sequences, a switch from a hybridoma-sourced monoclonal antibody to a recombinant version can lead to substantial differences in assay sensitivity and maximum signals due to impurities not detected by standard purity tests [67].
Quantifying the Impact on Assay Performance
The theoretical risks of LTLV manifest in tangible, measurable shifts in assay results. The following table compiles empirical data from a study investigating lot-to-lot comparability for five common immunoassay items, demonstrating the extent of variability observed in a real-world laboratory setting [69].
Table 2: Observed Lot-to-Lot Variation in Immunoassay Items [69]
| Analyte | Platform | Percentage Difference (% Diff) Range Between Lots | Maximum Difference to Standard Deviation (D:SD) Ratio |
|---|---|---|---|
| α-fetoprotein (AFP) | ADVIA Centaur | 0.1% to 17.5% | 4.37 |
| Ferritin | ADVIA Centaur | 1.0% to 18.6% | 4.39 |
| CA19-9 | Roche Cobas E 411 | 0.6% to 14.3% | 2.43 |
| HBsAg | Architect i2000 | 0.6% to 16.2% | 1.64 |
| Anti-HBs | Architect i2000 | 0.1% to 17.7% | 4.16 |
This data underscores the extensive and unpredictable variability that can occur across different analytes and instrument platforms. The D:SD ratio is a particularly insightful metric, as it represents the degree of difference between lots compared to the assay's daily variation. A high ratio indicates a shift that is large relative to the assay's inherent imprecision, signaling a clinically significant change [69].
Experimental Evaluation of Reagent Lots
Standardized Protocol for Lot-to-Lot Comparability Testing
To ensure new reagent lots do not adversely affect patient or research results, a standardized evaluation protocol must be followed. The general principle involves a side-by-side comparison of the current and new lots using patient samples [66] [70]. The workflow below outlines the key stages of this process.
Detailed Experimental Methodology:
Define Acceptance Criteria: Prior to testing, establish objective, pre-defined performance criteria for accepting the new lot. These criteria should be based on clinical requirements, biological variation, or total allowable error specifications—not arbitrary percentages [66] [70]. For a test like BNP with a single clinical application, this is straightforward; for multi-purpose tests like hCG, it is more complex [70].
Determine Sample Size and Range: Select a sufficient number of patient samples (typically 5 to 20) to ensure statistical power for detecting a clinically significant shift [66] [70]. The samples should, where possible, span the analytical range of the assay, with particular attention to concentrations near critical medical decision limits [70].
Execute Testing: All selected patient samples should be tested using both the current and new reagent lots on the same instrument, by the same operator, and on the same day to minimize extraneous sources of variation [66].
Statistical Analysis and Decision: Analyze the paired results to calculate the difference, percent difference, and the D:SD ratio [69]. Compare these results against the pre-defined acceptance criteria to make an objective decision on whether to accept or reject the new lot [66].
A Risk-Based Approach for Laboratory Efficiency
Performing a full patient comparison for every reagent lot change is resource-intensive. A modified, risk-based approach, as proposed by Martindale et al., categorizes assays to optimize validation efforts [66] [70]:
- Group 1 (Unstable/Tedious Assays): Includes tests for highly unstable analytes (e.g., ACTH) or laborious tests (e.g., fecal fats). Initial assessment with Internal Quality Control (IQC) material alone is considered the only practical method [66] [70].
- Group 2 (Historically Stable Assays): Includes assays with a history of showing minimal, clinically unimportant shifts (e.g., shifts in IQC of less than one standard deviation). Patient comparisons are only triggered if initial IQC measurements violate error rules [66] [70].
- Group 3 (High-Risk Assays): Includes tests with a known history of significant LTLV (e.g., hCG, troponin). Full patient comparison (e.g., 10 samples) is required regardless of initial IQC results [66] [70].
The Scientist's Toolkit: Essential Reagent Management Solutions
Successfully navigating reagent variability requires a suite of tools and strategies. The following table details key solutions for ensuring reagent quality and consistency.
Table 3: Research Reagent Solutions for Managing Quality and Variability
| Solution / Material | Function & Importance in Managing Variability |
|---|---|
| Native Patient Samples | Serves as the gold-standard material for lot comparability testing due to superior commutability over commercial IQC/EQA materials, which can yield misleading results [66]. |
| Characterization Profiles | A set of data (purity, concentration, affinity, specificity, aggregation) for each critical reagent lot. Serves as a benchmark for qualifying new lots and troubleshooting assay performance [68] [71]. |
| Moving Averages (Averages of Normally Distributed Individuals) | A statistical quality control procedure that monitors the average of patient results in real-time. Effective for detecting subtle, cumulative drifts in assay performance that individual lot-to-lot comparisons may miss [70]. |
| Critical Reagent Lifecycle Management | A comprehensive system for the generation, characterization, storage, and distribution of critical reagents. Ensures a consistent supply and maintains a consistent reagent profile throughout the drug development lifecycle [68]. |
| CLSI Evaluation Protocol EP26 | Provides a standardized, statistically sound protocol for user evaluation of reagent lot-to-lot variation, offering guidance on sample size, acceptance criteria, and data analysis [70]. |
Strategies for Mitigation and Future Outlook
Proactive Mitigation of Lot-to-Lot Variability
Addressing LTLV requires a proactive, multi-faceted strategy involving both manufacturers and end-users.
For Manufacturers: The focus should be on reducing variation at the point of manufacture by implementing rigorous quality control of raw materials and production processes. Setting acceptance criteria based on medical needs or biological variation, rather than arbitrary percentages, is a critical step forward [66] [67].
For Laboratories and Researchers: Beyond executing validation protocols, laboratories should implement moving averages to monitor long-term drift [70]. Furthermore, collaboration and data-sharing between laboratories and with manufacturers can provide a broader, more rapid detection system for problematic reagent lots [66].
Emerging Trends and Future Perspectives
The biological reagents market is dynamic, with several trends shaping its future:
Market Growth and Innovation: The global biological reagents market is poised for robust growth, projected to reach approximately $23,860 million by 2025 with a CAGR of 6.9% through 2033. This expansion is fueled by demand in advanced diagnostics, personalized medicine, and breakthroughs in genomics and proteomics, driving the need for higher-purity and more specific reagents [72].
Regulatory Evolution: While current regulatory guidelines on critical reagent management are limited, a renewed focus from agencies like the FDA and EMA is anticipated. This will likely lead to more specific recommendations on stability assessments, expiry/re-testing, and characterization [68].
Advanced Statistical Models: Bayesian statistical methodologies are being developed to provide a more adaptive, knowledge-building framework for lot release and variability assessment. These models integrate prior knowledge with new data for optimal risk-based decision making, showing promise for future application in reagent quality control [73].
In the realm of biomedical research and diagnostic assay development, the optimization of critical parameters is not merely a procedural step but a fundamental requirement for achieving robust, reproducible, and meaningful results. The performance of an assay—defined by its sensitivity, specificity, and accuracy—is intrinsically tied to the fine-tuning of variables such as incubation times, temperatures, and reagent concentrations. Within the broader thesis of evaluating specificity and sensitivity in functional assays, this guide provides a comparative analysis of optimization methodologies across key experimental platforms. We present objective performance data and detailed protocols to guide researchers and drug development professionals in systematically enhancing their assays, thereby ensuring that research outcomes are reliable and translatable.
Comparative Analysis of Optimization Parameters Across Key Assays
The following table summarizes the critical parameters and their optimal ranges for three foundational techniques: ELISA, Western Blotting, and qPCR. These values serve as a starting point for experimental setup and subsequent optimization.
Table 1: Key Optimization Parameters for Common Functional Assays
| Assay Type | Critical Parameter | Recommended Optimal Range | Performance Impact of Optimization |
|---|---|---|---|
| ELISA [74] [75] | Coating Antibody Concentration | 1-15 µg/mL (Purified) | Maximizes antigen capture; reduces non-specific binding. |
| Detection Antibody Concentration | 0.5-10 µg/mL (Purified) | Enhances specific signal; minimizes background. | |
| Blocking Buffer & Time | 1-2 hours, Room Temperature | Critical for reducing background noise. | |
| Enzyme Conjugate Concentration (HRP) | 10-200 ng/mL (system-dependent) | Balances signal intensity with background. | |
| Western Blot [76] [77] | Gel Electrophoresis Voltage | 150-300 V (with modified buffer) | Faster run times (23-45 min) with maintained resolution [77]. |
| Electrotransfer Time | 15-35 min (protein size-dependent) | Prevents over-transfer of small proteins or under-transfer of large ones [77]. | |
| Membrane Pore Size | 0.22 µm for proteins <25 kDa | Prevents loss of low molecular weight proteins [77]. | |
| Blocking Time | 10-60 minutes | Reduces background; insufficient blocking increases noise [76]. | |
| qPCR [78] [79] | Primer Melting Temperature (Tm) | 60-64°C | Ideal for enzyme function and specificity. |
| Primer Annealing Temperature (Ta) | Tm -5°C | Balances specificity (higher Ta) and efficiency (lower Ta). | |
| GC Content | 35-65% (50% ideal) | Ensures stable primer binding; avoids secondary structures. | |
| Amplicon Length | 70-150 bp | Optimized for efficient amplification with standard cycling. |
Detailed Experimental Protocols for Optimization
Checkerboard Titration for ELISA Optimization
The checkerboard titration is a fundamental method for simultaneously optimizing paired assay components, such as capture and detection antibodies [74].
Methodology:
- Plate Coating: Prepare a dilution series of the capture antibody in coating buffer (e.g., 1, 5, 10, and 15 µg/mL). Dispense different concentrations into rows of a microplate.
- Blocking: After coating and washing, block the plate with a suitable protein-based buffer (e.g., BSA or serum) for 1-2 hours at room temperature.
- Antigen Addition: Add a constant, known concentration of the target antigen to all wells.
- Detection Antibody Titration: Prepare a dilution series of the detection antibody. Apply different concentrations to the columns of the plate.
- Signal Detection: Proceed with the addition of enzyme conjugate and substrate according to standard protocol.
- Data Analysis: The optimal combination is identified as the lowest concentration of both antibodies that yields the strongest specific signal with the lowest background.
Bayesian Optimization for High-Dimensional Biological Processes
For complex, high-dimensional optimization problems—such as balancing the expression levels of multiple genes in a metabolic pathway—traditional one-factor-at-a-time approaches are inefficient. Bayesian Optimization (BO) provides a powerful, machine learning-driven alternative [80].
Methodology:
- Principle: BO is a sequential strategy for global optimization of "black-box" functions that are expensive to evaluate. It is ideal for biological experiments where testing every possible parameter combination is infeasible [80].
- Core Components:
- Probabilistic Surrogate Model: A Gaussian Process (GP) is used to model the unknown relationship between input parameters (e.g., inducer concentrations) and the output (e.g., product yield). The GP provides a prediction of the mean output and the associated uncertainty (variance) for any untested point [80].
- Acquisition Function: This function uses the GP's predictions to propose the next most informative experiment by balancing exploration (testing regions of high uncertainty) and exploitation (testing regions predicted to have high performance). Common functions include Expected Improvement (EI) and Upper Confidence Bound (UCB) [80].
- Workflow: The process is iterative. After a few initial experiments, the BO algorithm proposes the next parameter set to test. The result of that experiment is then used to update the GP, and the process repeats, rapidly converging on the global optimum [80].
- Validation: In a retrospective study optimizing a 4-dimensional metabolic pathway, a BO policy converged to the optimum in just 19 experimental points, compared to the 83 points required by a traditional grid search [80].
Diagram 1: Bayesian Optimization Workflow for guiding resource-efficient experimentation.
Gradient Analysis for Western Blotting
Optimizing antibody concentrations in Western Blotting can be efficiently achieved through gradient analysis, which can be performed via protein or reagent gradients [76].
Methodology:
- Protein Gradient: Load a series of dilutions of your protein sample across multiple lanes. This determines the dynamic range of the antibody and the ideal protein load for subsequent experiments.
- Reagent Gradient:
- Load the same protein concentration in multiple lanes.
- After transfer, carefully cut the membrane into individual lanes.
- Incubate each lane with a different concentration of the primary antibody.
- After washing and incubation with secondary antibody, reassemble the membrane for imaging.
- Data Analysis: The optimal antibody dilution is the one that provides the strongest specific signal with the clearest bands and the lowest background.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Their Functions in Assay Optimization
| Tool / Reagent | Primary Function | Application Notes |
|---|---|---|
| Antibody-Matched Pairs [74] | Capture and detect target antigen in sandwich ELISA. | Require validation for mutual compatibility; critical for specificity. |
| Blocking Buffers (BSA, Milk) [74] [76] | Coat unused binding sites on plates or membranes to reduce background. | Choice of blocker (e.g., milk vs. BSA) can impact specific antibody performance. |
| Modified Electrotransfer Buffers [77] | Facilitate protein transfer from gel to membrane. | Replacing methanol with ethanol reduces toxicity; SDS content can be adjusted for protein size. |
| Double-Quenched qPCR Probes [79] | Report amplification in real-time via fluorophore-quencher separation. | Provide lower background and higher signal-to-noise than single-quenched probes. |
| Pre-mixed Gel Reagents [77] | Simplify and accelerate polyacrylamide gel preparation. | Stable for weeks at 4°C, reducing procedural time and variability. |
| Horseradish Peroxidase (HRP) [74] [75] | Enzyme for colorimetric, chemiluminescent, or fluorescent detection. | Concentration must be optimized for the specific substrate and detection system. |
Advanced Optimization: Beyond Basic Parameters
Diagram 2: Format selection and optimization logic for immunoassays, highlighting the distinct pathways for sandwich versus competitive formats.
For certain applications, optimization extends beyond basic parameters to the fundamental design of the assay.
Competitive vs. Sandwich Assay Formats: The choice between these formats is often dictated by the size of the analyte. Sandwich assays are suitable for larger molecules with at least two epitopes and provide an intuitive readout where signal is directly proportional to the analyte concentration. In contrast, competitive assays are used for small molecules or single-epitope targets. They require intricate optimization to balance the amounts of bioreceptors and a synthetic competitor, and they produce a counter-intuitive output where the signal decreases as the analyte concentration increases. A key advantage of competitive assays is their inherent insensitivity to the "hook effect," a cause of false negatives in sandwich assays [81].
Addressing Individual Variability with Machine Learning: As demonstrated in physiological monitoring, advanced computational models like the fusion of Kalman Filters and Long-Sequence Forecasting (LTSF) models can be trained on individual-specific data (e.g., heart rate, skin temperature) to predict a critical outcome (e.g., core body temperature) with high accuracy [82]. This principle can be translated to assay development, where models could be trained to predict optimal conditions for new biological systems based on historical experimental data, accounting for unique reagent batches or cell lines.
The path to a highly specific and sensitive functional assay is paved with systematic optimization. As the comparative data and protocols in this guide illustrate, there is no universal set of parameters; optimal conditions must be empirically determined for each experimental system. While foundational methods like checkerboard titrations and gradient analyses remain indispensable, the adoption of advanced strategies like Bayesian Optimization represents a paradigm shift. These data-driven approaches can dramatically accelerate the optimization cycle, conserve precious reagents, and navigate complex, high-dimensional parameter spaces that are intractable for traditional methods. By rigorously applying these principles, researchers can ensure their assays are robust and reliable, thereby solidifying the foundation upon which scientific discovery and drug development are built.
Addressing Matrix Interference in Complex Biological Samples
Matrix interference represents a fundamental challenge in the bioanalysis of complex biological samples, such as blood, plasma, urine, and tissues. These effects occur when extraneous components within the sample matrix disrupt the accurate detection and quantification of target analytes, leading to potentially compromised data in drug development and diagnostic applications [83] [84]. The sample matrix comprises all components of a sample other than the analyte of interest—including proteins, lipids, salts, carbohydrates, and metabolites—which collectively can interfere with analytical measurements through various mechanisms [85]. In the context of evaluating specificity and sensitivity in functional assays research, effectively managing matrix interference is not merely an analytical optimization step but a critical prerequisite for generating reliable, reproducible, and biologically meaningful data.
The mechanisms of interference are diverse and system-dependent. In immunoassays, matrix components such as heterophilic antibodies or other plasma proteins can compete with target analytes for antibody binding sites, thereby disrupting the antigen-antibody interaction and leading to inaccurate signal measurements [86]. In mass spectrometry-based methods, co-eluting matrix components predominantly cause ion suppression or enhancement effects within the ionization source, ultimately affecting the accuracy of quantitative results [85] [84]. The fundamental problem stems from the discrepancy between the ideal calibrated environment, where standards are typically prepared in clean buffers, and the complex reality of biological samples, where thousands of potential interferents coexist with the target analyte [83] [85]. Understanding and addressing these matrix effects is therefore essential for researchers and scientists who depend on precise measurements for biomarker validation, pharmacokinetic studies, and clinical diagnostics.
Comparative Analysis of Mitigation Strategies
A range of strategies has been developed to mitigate matrix interference, each with distinct advantages, limitations, and applicability depending on the analytical platform and sample type. The choice of strategy significantly influences the sensitivity, specificity, and throughput of an assay.
Table 1: Comparison of Major Matrix Interference Mitigation Strategies
| Strategy | Key Principle | Typical Applications | Impact on Sensitivity | Throughput & Ease of Automation |
|---|---|---|---|---|
| Sample Dilution | Reduces concentration of interferents below a critical threshold [83]. | ELISA, LC-MS initial sample handling [83] [87]. | Can decrease sensitivity if analyte is also diluted. | High; easily automated and integrated [88]. |
| Solid-Phase Extraction (SPE) | Selectively isolates analyte from interfering matrix using functionalized sorbents [89]. | LC-MS/MS, sample cleanup for complex matrices [89] [88]. | Generally improves sensitivity via analyte enrichment. | Medium; 96-well formats and online systems are available [88]. |
| Protein Precipitation | Removes proteins by adding organic solvents or acids [88]. | Quick plasma/serum cleanup prior to LC-MS. | Can lead to analyte loss; may not remove all interferents. | High; amenable to 96-well plate formats [88]. |
| Internal Standardization | Uses a standard compound to correct for variability in sample processing and ionization [85] [87]. | Essential for quantitative LC-MS, GC-MS. | Does not directly affect, but greatly improves quantitation accuracy. | High; easily incorporated into automated workflows. |
| Antibody Optimization | Adjusts antibody surface coverage and affinity to outcompete low-affinity interferents [86]. | Microfluidic immunoassays, biosensor development. | Can be optimized to maintain or enhance sensitivity. | Low-Medium; requires careful assay development. |
| Matrix-Matched Calibration | Uses standards prepared in the same matrix as samples to correct for background effects [83]. | Various, including ELISA and spectroscopic methods. | Helps recover true sensitivity by accounting for background. | Low; requires sourcing and testing of blank matrix. |
The selection of an appropriate mitigation strategy is a critical decision in assay design. For instance, while sample dilution is straightforward and easily automatable, it may be unsuitable for detecting low-abundance analytes [83] [87]. Solid-phase extraction (SPE) and related sorbent-based techniques have gained prominence due to the development of high-performance media, including porous organic frameworks, molecularly imprinted polymers, and carbon nanomaterials, which offer superior selectivity and enrichment capabilities [89]. For mass spectrometric applications, the use of a stable isotope-labeled internal standard (SIL-IS) is considered one of the most effective approaches because it can correct for both sample preparation losses and ion suppression/enhancement effects, as the IS and analyte experience nearly identical matrix effects [85] [87] [84].
A pivotal finding from recent research on microfluidic immunoassays highlights that antibody surface coverage is a major factor governing serum matrix interference. Studies demonstrate that optimizing the density of immobilized capture antibodies can effectively minimize interference from low-affinity serum components, without necessitating additional sample preparation steps [86]. This insight provides a new route for developing robust point-of-care tests by shifting the paradigm of assay optimization from buffer-based to serum-based conditions [86].
Experimental Protocols for Key Mitigation Approaches
To ensure the reliability and reproducibility of bioanalytical data, it is essential to implement and document robust experimental protocols for assessing and controlling matrix interference. The following sections detail established methodologies for two critical approaches: evaluating and optimizing antibody surface coverage in immunoassays, and implementing the internal standard method for LC-MS quantification.
Protocol 1: Optimizing Antibody Surface Coverage in Microfluidic Immunoassays
This protocol is designed to systematically investigate and optimize the density of immobilized antibodies to minimize matrix interference, based on experimental approaches validated in recent literature [86].
- Step 1: Capillary Surface Preparation. Use fluorinated microcapillary film (MCF) strips or similar microfluidic channels with a consistent internal diameter (e.g., 212 μm). Ensure the inner surface is clean and amenable to homogeneous antibody coating [86].
- Step 2: Variable Antibody Coating. Prepare a series of capture antibody solutions at varying concentrations (e.g., ranging from 0 to 200 μg/mL). Introduce these solutions into separate microcapillary channels and incubate to allow for immobilization. This creates a gradient of antibody surface coverage across the different channels [86].
- Step 3: Blocking and Sample Incubation. After coating, block all channels with a suitable blocking agent (e.g., 3% w/v protease-free BSA in PBS) to minimize nonspecific binding. Subsequently, introduce a fixed concentration of the target antigen prepared in both a control buffer (e.g., PBS) and the biological matrix of interest (e.g., undiluted human serum) into the respective channels. Maintain a constant antigen incubation time (e.g., 5 minutes) [86].
- Step 4: Detection and Signal Analysis. Perform the necessary steps for signal generation according to the assay format (e.g., add a labeled detection antibody and enzymatic substrate for a colorimetric readout). Capture digital images of the microcapillary strips and quantify the signal intensity. The optimal antibody surface coverage is identified as the concentration that yields a strong, specific signal for the serum sample that is comparable to the signal obtained in the buffer control, indicating minimal matrix interference [86].
- Step 5: Validation with Whole Blood. To further validate the optimized conditions, repeat the assay using the identified optimal antibody concentration and test analyte spiked into whole blood. Compare the signal recovery against matched buffer and serum samples to confirm the robustness of the protocol under more complex matrix conditions [86].
Protocol 2: Implementing Internal Standardization for LC-MS/MS Quantification
This protocol outlines the use of the internal standard method to correct for matrix effects, a cornerstone of reliable quantitative analysis in mass spectrometry [85] [87] [84].
- Step 1: Selection of Internal Standard. The ideal internal standard is a stable isotope-labeled (SIL) analogue of the target analyte, which has nearly identical chemical and physical properties. If a SIL analogue is unavailable, a structural analogue with similar chromatography and ionization behavior can be selected [85].
- Step 2: Sample Preparation with IS. Add a fixed, known amount of the internal standard to every sample, including calibrators, quality controls (QCs), and unknown study samples, at the earliest possible stage of the sample preparation process. This ensures the IS corrects for variability throughout sample processing and analysis [85] [84].
- Step 3: Calibration with Ratios. Prepare the calibration curve using a series of standard solutions with known concentrations of the target analyte. For each calibration point, plot the y-axis as the peak area ratio of the analyte to the internal standard and the x-axis as the concentration ratio of the analyte to the internal standard [85].
- Step 4: Data Acquisition and Analysis. Inject the prepared samples into the LC-MS/MS system. Quantify the target analyte and the internal standard in each sample based on their specific mass transitions (MRM) and retention times.
- Step 5: Quantification. For each unknown sample, calculate the analyte-to-internal standard peak area ratio. Use this ratio and the established calibration curve to back-calculate the concentration of the target analyte in the sample. This method corrects for losses during sample preparation and for matrix-induced suppression or enhancement of the ionization efficiency [85] [87].
Table 2: Key Research Reagent Solutions for Managing Matrix Interference
| Reagent / Material | Function in Mitigating Interference | Application Examples |
|---|---|---|
| Stable Isotope-Labeled Internal Standards | Corrects for analyte loss during preparation and matrix effects during ionization; the gold standard for MS quantitation [85] [87]. | LC-MS/MS biomonitoring of pesticides, pharmaceuticals, and endogenous metabolites [87] [84]. |
| Porous Organic Frameworks (MOFs/COFs) | High-surface-area sorbents for selective extraction and enrichment of analytes, removing them from the complex matrix [89]. | SPE for glycopeptides, pesticides, and drugs from urine, serum, and meat samples [89]. |
| Molecularly Imprinted Polymers | Synthetic antibodies with tailor-made recognition sites for a specific analyte, offering high selectivity during extraction [89]. | MSPE of fluoroquinolones, cocaine, and catalpol from biological fluids [89]. |
| Ion Exchange/Functionalized Sorbents | Selectively bind ionic interferents or analytes based on charge, cleaning up the sample matrix [90] [89]. | Isolation of Cr(III) and Cr(VI) in soil extracts and water [90]. |
| High-Purity Blocking Agents | Reduce nonspecific binding of matrix proteins and other components to assay surfaces and reagents [83] [86]. | Immunoassay development on microfluidic strips and ELISA plates [83] [86]. |
Strategic Workflow and Implementation Guide
Navigating the various options for managing matrix interference requires a systematic strategy. The following decision pathway visualizes a logical sequence for selecting and combining methods to achieve optimal assay performance.
The successful implementation of a matrix interference strategy extends beyond the initial selection of methods. For mass spectrometry, the use of a stable isotope-labeled internal standard remains the most reliable corrective measure, but it should be paired with adequate sample cleanup to ensure overall assay robustness [85] [87] [84]. For immunoassays, the emerging best practice is to conduct final assay optimization directly in the target biological matrix, fine-tuning parameters like antibody concentration and incubation times to outcompete interferents [86]. Furthermore, rigorous validation is mandatory. This includes conducting spike-and-recovery experiments to assess accuracy and using post-column infusion experiments to visualize ion suppression zones in LC-MS methods [85] [84]. By adhering to a systematic workflow and leveraging advanced reagents and materials, researchers can effectively neutralize the challenge of matrix interference, thereby ensuring the generation of specific, sensitive, and reliable data for functional assays research.
Leveraging Automation to Improve Precision, Throughput, and Reproducibility
In the fields of drug development and functional assay research, the traditional reliance on manual processes has become a significant bottleneck, introducing variability and limiting the pace of discovery. The convergence of increasing demand for precision medicine, the need for high-throughput screening in pharmaceutical R&D, and the ongoing reproducibility crisis in science has made automation an indispensable tool for the modern laboratory [91] [92]. Automation technologies are revolutionizing how scientists approach experiments, moving from artisanal, hands-on protocols to standardized, data-rich, and highly repeatable workflows. This transformation is not merely about speed; it is about enhancing the very quality and reliability of scientific data itself. This guide objectively compares leading automation approaches and platforms, providing researchers and drug development professionals with the data and frameworks needed to evaluate how automation can be leveraged to achieve superior precision, throughput, and reproducibility within their specific research contexts, particularly in sensitivity and specificity functional assays.
The Impact of Automation on Core Research Metrics
Automation influences research outcomes across three critical dimensions: precision, throughput, and reproducibility. The relationship between these enhanced metrics and overall research efficacy can be visualized as follows:
Enhancing Precision and Data Quality
Automation significantly reduces the coefficient of variation (CV) in experimental procedures, a critical factor in functional assays where small signal differences determine outcomes. For instance, in nucleic acid normalization—a foundational step in many molecular assays—automated liquid handlers have demonstrated a CV of under 5% for both volumetric transfers and final normalized concentrations, a level of consistency difficult to maintain manually [93]. This precision is paramount for assays evaluating specificity and sensitivity, as it minimizes background noise and enhances the accurate detection of true positives and negatives.
Accelerating Throughput and Efficiency
The most evident impact of automation is the dramatic acceleration of laboratory workflows. A compelling case study from a contract research organization (CRO) automating its virology ELISA testing showed that a task previously requiring two technicians and 45 minutes per plate was reduced to 20-25 minutes with automation, freeing highly skilled staff for higher-value analysis [92]. This leap in efficiency is driven by systems capable of uninterrupted operation and parallel processing, enabling researchers to scale their experimental ambitions and generate data at a pace commensurate with modern drug development cycles.
Establishing Robust Reproducibility
Reproducibility is the cornerstone of trustworthy science, yet over 70% of researchers have reported failing to reproduce another scientist's experiments [92]. Automation directly addresses this "reproducibility crisis" by enforcing standardized protocols. When an experimental workflow is codified into an automated system, the procedure remains constant across different users, days, and even laboratories [92]. This eliminates subtle protocol divergences that can lead to irreproducible results, ensuring that data generated in one lab can be reliably replicated in another, thereby strengthening the foundation of collaborative and translational research.
Comparative Analysis of Laboratory Automation Systems
Selecting the appropriate automation system requires a careful balance of needs. The following flowchart provides a strategic framework for this decision-making process, emphasizing the critical choice between throughput and adaptability:
Performance Benchmarking of Automation Platforms
The market offers a spectrum of automation solutions, each with distinct strengths. The table below summarizes the key performance indicators and primary use cases for several system types based on real-world implementations.
Table 1: Comparative Performance of Laboratory Automation Systems
| System Type / Feature | Reported Precision (CV) | Throughput Improvement | Key Strengths | Ideal Research Context |
|---|---|---|---|---|
| High-Throughput Multi-channel | <5% (volumetric) [93] | 2-3x faster than manual [93] | High speed for large sample numbers; parallel processing | Repetitive screening (e.g., compound libraries, clinical chemistry) [94] |
| Adaptable R&D Platforms | High (protocol standardization) [93] | Saves hours of manual labor [92] | Flexibility; ease of re-configuration; user-friendly software | Early-stage R&D with evolving protocols; multi-purpose labs [93] |
| Single-Channel Precision | High (avoids reagent waste) [93] | Faster than manual, but not highest speed [93] | Superior liquid handling for scarce reagents; glove-box compatible | Protein crystallography; nucleic acid quantification; sensitive assays [93] |
| Fully Integrated Workflows | High (end-to-end tracking) [92] | Reduces process from 45min to 25min [92] | Full audit trails; barcode tracking; seamless data flow | Regulated environments; CROs; high-integrity biobanking [92] |
Strategic Tool Selection for Enterprise Needs
Beyond the lab bench, the choice of automation software and data management tools is critical for integrating automation into the broader research data pipeline. The following table compares key tool categories that support automated workflows.
Table 2: Comparison of Automation Software and Data Tool Categories
| Tool Category | Key Features | Reported Benefits | Considerations |
|---|---|---|---|
| AI-Powered Test Platforms (e.g., Virtuoso QA, Testim) [95] | Natural language programming; self-healing tests; AI-driven element detection [95] | 10x faster test creation; 85% lower maintenance [95] | Can have a steeper learning curve for non-technical users [95] |
| Traditional Frameworks (e.g., Selenium) [96] [97] | High customization; open source; strong developer community [96] | Full programming control; no licensing cost [97] | High maintenance (60-70% of effort); requires coding skills [95] |
| Codeless Platforms (e.g., Katalon, BugBug) [96] [97] | Record-and-playback; visual test building; keyword-driven [95] | Accessible to non-programmers; faster initial setup [96] | Less flexible for complex scenarios; may lack advanced features [96] |
Experimental Protocols: Quantifying Automation Benefits
To provide concrete, data-driven evidence of automation's impact, we outline two key experimental protocols that measure improvements in precision and reproducibility.
Protocol 1: Assessing Precision in Nucleic Acid Normalization
This protocol is designed to quantify the precision gains of an automated liquid handler over manual pipetting in a common sample preparation step.
- Objective: To compare the coefficient of variation (CV) of nucleic acid concentration and volume delivery between manual and automated normalization methods.
- Materials:
- Automated Liquid Handler: (e.g., Hudson Lab Automation system, single or multi-channel) [93].
- Manual Pipettes: Calibrated single and multi-channel pipettes.
- Sample: Genomic DNA or PCR product at varying concentrations.
- Normalization Buffer: TE buffer or nuclease-free water.
- Quantification Instrument: Fluorometer (e.g., Qubit) or spectrophotometer (e.g., NanoDrop).
- Method:
- Sample Preparation: Prepare a master mix of nucleic acid at a known, non-uniform concentration across a 96-well plate.
- Automated Normalization: Program the liquid handler to normalize all samples to a target concentration (e.g., 10 ng/μL) in a new destination plate. The system will calculate and transfer the required volume of sample and buffer.
- Manual Normalization: A highly experienced technician performs the same normalization procedure on an identical source plate.
- Data Collection: Quantify the final concentration of every normalized sample in both plates using the fluorometer. Record the concentration and the calculated volume that was transferred.
- Data Analysis:
- For each group (automated and manual), calculate the mean final concentration and the standard deviation.
- The Coefficient of Variation (CV) = (Standard Deviation / Mean) x 100.
- Compare the CVs between the two groups. A well-tuned automated system typically achieves a CV of under 5%, while manual pipetting often results in a higher CV [93].
- Expected Outcome: The automated process will demonstrate a statistically significant lower CV, confirming superior precision and reduced variability in sample preparation.
Protocol 2: Evaluating Reproducibility Across Multiple Runs and Users
This protocol tests the core strength of automation: its ability to produce the same result consistently over time and across different operators.
- Objective: To measure the inter-run and inter-user reproducibility of a cell viability assay (e.g., ATP assay) performed manually versus with an automated system.
- Materials:
- Cell Line: A standard adherent or suspension cell line (e.g., HEK293, HeLa).
- Viability Assay Kit: Commercially available ATP assay kit (e.g., Promega, Thermo Fisher) [91].
- Automation System: Integrated system for cell dispensing, compound addition, and luminescence reading, or a liquid handler for reagent transfer paired with a plate reader.
- Test Compound: A compound with a known IC50 value for the cell line.
- Method:
- Plate Setup: Seed cells in multiple 96-well plates at a predetermined density. The layout should include a negative control (media only), a positive control (untreated cells), and a dilution series of the test compound.
- Automated Execution: A single programmed method on the automated system is used to:
- Dispense the compound dilution series onto the cells.
- Incubate for the required period.
- Add the ATP assay reagents.
- Measure the luminescent signal.
- Manual Execution: Different trained researchers (User A, User B, etc.) independently perform the entire assay on separate days using manual pipetting.
- Replication: The automated run is repeated three times on different days. The manual assay is performed by at least two different users, also with replicates.
- Data Analysis:
- Normalize luminescence data to percent viability relative to the positive control.
- Plot dose-response curves and calculate the IC50 value for each run and user.
- Calculate the Mean IC50 and Standard Deviation for the automated group and the manual group.
- The key metric is the variability in IC50 values: Lower standard deviation in the automated group indicates higher reproducibility [92].
- Expected Outcome: The IC50 values generated by the automated system will cluster more tightly (lower standard deviation) than those generated by different manual users, demonstrating automation's critical role in achieving reproducible results.
The Scientist's Toolkit: Essential Reagents and Materials for Automated Assays
The successful implementation of automation relies on a suite of specialized consumables and reagents designed for reliability and compatibility with automated platforms.
Table 3: Essential Research Reagent Solutions for Automated Workflows
| Item | Function in Automated Workflow | Key Considerations |
|---|---|---|
| ATP Assay Kits | Measure cell viability and cytotoxicity via ATP quantitation; crucial for high-throughput drug screening [91]. | Opt for "glow-type" kinetics for compatibility with automated plate readers; ensure reagent stability for unattended runs. |
| Luminescence & Detection Reagents | Generate stable, long-half-life signals for detection in luminometers and spectrophotometers [91]. | Compatibility with high-throughput detection systems; low background signal; ready-to-use formulations to minimize manual prep. |
| Assay-Ready Microplates | Standardized plates (96, 384-well) for housing samples and reactions in automated systems. | Must have precise well dimensions and low well-to-well crosstalk; options include white plates for luminescence and black for fluorescence. |
| Nucleic Acid Normalization Kits | Provide optimized buffers for accurately diluting DNA/RNA to a uniform concentration for downstream assays [93]. | Suitability for direct use in liquid handler programs; buffer viscosity must be compatible with non-contact dispensing if used. |
| Cell-Based Assay Consumables | Includes culture plates, automated trypsinization reagents, and cell viability stains. | Plates should offer excellent cell attachment and edge effect minimization for consistent results across the entire plate. |
The integration of automation into the research laboratory is no longer a luxury but a fundamental requirement for achieving the levels of precision, throughput, and reproducibility demanded by contemporary science and drug development. As the data and protocols in this guide demonstrate, the strategic selection and implementation of automation systems—from adaptable liquid handlers to integrated software platforms—yield tangible, quantifiable benefits. These include a drastic reduction in operational variability, the ability to scale experiments to statistically powerful levels, and the generation of robust, reproducible data that can be trusted across the global scientific community. For researchers focused on specificity and sensitivity in functional assays, embracing these technologies is the most direct path to enhancing assay quality, accelerating discovery timelines, and ultimately, delivering more effective therapeutics.
Establishing Credibility: Validation Frameworks and Comparative Analysis
The transition from high-throughput genetic sequencing to clinically actionable insights represents a major bottleneck in modern precision medicine. While technologies like Next-Generation Sequencing (NGS) can identify millions of genetic variants, the clinical utility of this data is constrained by interpretation challenges. A significant obstacle is the prevalence of Variants of Uncertain Significance (VUS), which account for approximately 79% of missense variants in clinically relevant cardiac genes [98]. The existence of these VUS classifications prevents the identification of at-risk individuals, hinders family screening, and can lead to unnecessary clinical surveillance in low-risk patients [98]. This validation framework addresses the pressing need for systematic approaches to resolve VUS interpretations by integrating disease biology with functional assessment, ultimately supporting more reliable and equitable genomic medicine.
Four-Step Validation Framework
A robust, systematic framework is essential for translating genetic findings into clinically validated results. This structured approach ensures that variant interpretation is grounded in biological mechanism and supported by rigorous experimental evidence.
Step 1: Establish Disease Context and Gene-Disease Validity
Objective: Define the biological and clinical context for variant interpretation, establishing the relationship between gene function and disease mechanism.
Methodology:
- Gene-Disease Relationship Review: Determine the strength of evidence associating the gene with a specific disease phenotype through manual curation of scientific literature and existing databases [99].
- Inheritance Pattern Establishment: Identify the mode of inheritance (autosomal dominant, autosomal recessive, X-linked) for the condition [99].
- Variant Type Impact Assessment: Categorize variant types (nonsense, frameshift, missense, splice-site) and their expected functional consequences based on gene function and disease mechanism [99]. For example, in genes like BRCA2 where loss-of-function is a known disease mechanism, nonsense variants are considered strong evidence for pathogenicity [100].
Key Outputs: Documented gene-disease validity, established disease mechanism (loss-of-function, gain-of-function, dominant-negative), and defined functional domains critical for protein activity.
Step 2: Implement Functional Assays for Variant Effect
Objective: Systematically assess the functional consequences of genetic variants using standardized experimental approaches.
Methodology: Selection of appropriate functional assays based on gene function and disease mechanism:
Multiplexed Assays of Variant Effect (MAVEs): These high-throughput approaches enable functional assessment of thousands of variants in parallel, generating proactive evidence for variants not yet observed in patients [98]. Key MAVE methodologies include:
- Saturation Genome Editing (SGE): CRISPR-Cas9-based knock-in to introduce variants at endogenous loci, as demonstrated in the comprehensive functional evaluation of BRCA2 variants [100].
- Landing Pad Systems: Exogenous delivery of variant libraries to engineered genomic sites for consistent expression [98].
- Cell Survival Assays: Functional readout for essential genes, where pathogenic variants disrupt cell viability [100].
Assay Selection Criteria: Choose assays that best recapitulate the gene's biological function, such as homology-directed repair assays for DNA repair genes like BRCA2, or surface abundance and electrophysiology for ion channel genes [98].
Key Outputs: Quantitative functional scores for variants, comparison to known pathogenic and benign controls, and preliminary classification of variant impact.
Step 3: Assess Analytical Performance and Clinical Validity
Objective: Rigorously evaluate the performance characteristics of functional assays to ensure reliability and clinical applicability.
Methodology:
- Reference Standard Establishment: Utilize variants with established pathogenicity or benignity from databases like ClinVar as reference standards [100].
- Performance Metric Calculation: Determine key analytical parameters including:
- Statistical Validation: Employ appropriate statistical models such as the VarCall Bayesian model to assign probabilities of pathogenicity with confidence metrics [100].
Table 1: Performance Metrics for Functional Assays Based on Published Studies
| Assay Type | Gene | Sensitivity | Specificity | Validation Standard |
|---|---|---|---|---|
| Saturation Genome Editing | BRCA2 | 94% (missense) | 95% (missense) | ClinVar & HDR Assay [100] |
| MAVE (Multiple Genes) | CALM1/2/3, KCNH2, KCNE1 | Varies by gene & assay | Varies by gene & assay | Known pathogenic/benign variants [98] |
Key Outputs: Validated assay performance characteristics, defined quality control parameters, and established thresholds for pathogenicity classification.
Step 4: Integrate Evidence for Variant Classification
Objective: Synthesize functional data with other evidence types to assign clinically relevant variant classifications.
Methodology:
- ACMG/AMP Framework Application: Integrate functional evidence (PS3/BS3 codes) with population data, computational predictions, and familial segregation data following established guidelines [99].
- Evidence Integration: Combine functional evidence with:
- Classification Assignment: Apply decision-tree algorithms to assign one of five standardized categories: Pathogenic, Likely Pathogenic, Variant of Uncertain Significance, Likely Benign, or Benign [99].
Key Outputs: Final variant classification, comprehensive evidence summary, and clinical reporting recommendations.
Comparative Analysis of Functional Assay Technologies
Different functional assay technologies offer distinct advantages and limitations for variant effect assessment. Understanding these differences is crucial for selecting the most appropriate method for specific genes and disease contexts.
Table 2: Comparison of Functional Assay Technologies for Variant Effect Assessment
| Technology | Throughput | Key Advantages | Limitations | Representative Applications |
|---|---|---|---|---|
| Saturation Genome Editing (SGE) | High (Thousands of variants) | • Endogenous context• Assesses splicing effects• High clinical concordance | • Technically challenging• Limited to editable cell lines | BRCA2 DBD variants [100] |
| Landing Pad Systems | High (Thousands of variants) | • Controlled expression• Flexible cell models• Standardized workflows | • Non-native genomic context• Misses non-coding effects | Ion channels (KCNH2, KCNE1) [98] |
| Homology-Directed Repair (HDR) Assays | Medium (Dozens to hundreds) | • Direct function measurement• Established validation• Clinically accepted | • Lower throughput• Specialized applications | DNA repair genes [100] |
| Manual Patch Clamp Electrophysiology | Low (Single variants) | • Gold standard for ion channels• Direct functional readout• High information content | • Very low throughput• Technical expertise required | Cardiac channelopathies [98] |
Experimental Protocols for Key Assays
Detailed methodological information ensures proper implementation and validation of functional assays within the proposed framework.
Protocol: Saturation Genome Editing for Variant Functionalization
This protocol is adapted from the comprehensive BRCA2 MAVE study that functionally evaluated 6,959 single-nucleotide variants [100].
Step 1: Library Design and Generation
- Design site-saturation mutagenesis libraries to cover all possible single-nucleotide variants in target regions (e.g., exons 15-26 of BRCA2 covering the DNA-binding domain).
- Generate variant libraries using NNN-tailed PCR primers for maximum diversity coverage.
- Include 10 bp of adjacent intronic sequence to capture potential splice effects.
Step 2: Cell Line Preparation and Transfection
- Utilize haploid HAP1 cells to enable clear functional assessment of essential genes.
- Co-transfect variant library plasmids with Cas9-sgRNA constructs targeting each genomic region.
- Perform experiments in triplicate to assess reproducibility.
Step 3: Functional Selection and Sampling
- Collect genomic DNA samples at day 0 (baseline), day 5, and day 14 post-transfection.
- Monitor cell viability as selection readout for essential genes.
Step 4: Sequencing and Data Analysis
- Perform amplicon-based deep paired-end sequencing of all timepoints.
- Calculate variant frequency ratios between day 14 and day 0.
- Apply statistical models (e.g., VarCall Bayesian model) to adjust for position-dependent effects and assign pathogenicity probabilities [100].
Protocol: High-Throughput Screening Assay Validation
Adapted from the NCBI Assay Guidance Manual, this protocol ensures robust performance of high-throughput functional assays [101].
Step 1: Plate Uniformity and Signal Variability Assessment
- Conduct 3-day plate uniformity studies using the DMSO concentration planned for screening.
- Measure three critical signals:
- "Max" signal: Maximum assay response (e.g., untreated control for inhibition assays)
- "Min" signal: Background signal (e.g., fully inhibited control)
- "Mid" signal: Intermediate response (e.g., EC50 or IC50 concentration of control compound)
Step 2: Replicate-Experiment Study
- Perform independent experiments across multiple days to assess inter-assay variability.
- Include reference compounds with known effects in each run.
Step 3: Data Analysis and Quality Control
- Calculate Z'-factor to assess assay quality and robustness: Z' = 1 - [3×(σpositive + σnegative)] / |μpositive - μnegative|
- Establish acceptance criteria: Z' > 0.5 indicates excellent assay quality suitable for screening.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of the validation framework requires specific reagents and tools optimized for functional genomics applications.
Table 3: Essential Research Reagents and Materials for Variant Functionalization
| Reagent/Material | Function | Application Examples | Key Considerations |
|---|---|---|---|
| CRISPR-Cas9 System | Endogenous genome editing | Saturation genome editing [100] | • Editing efficiency• Off-target effects• Delivery method |
| Site-Saturation Mutagenesis Libraries | Variant library generation | BRCA2 DBD variant assessment [100] | • Coverage completeness• Representation bias• Synthesis quality |
| Landing Pad Cell Lines | Consistent variant expression | Ion channel MAVEs (KCNH2, KCNE1) [98] | • Genomic safe harbor• Single-copy integration• Expression stability |
| HAP1 Haploid Cells | Functional genomics | Essential gene assessment [100] | • Haploid stability• Genetic background• Transfection efficiency |
| Validated Reference Variants | Assay calibration | Pathogenic/benign controls [100] | • Clinical validity• Functional characterization• Population frequency |
The four-step validation framework presented here provides a systematic pathway from disease mechanism understanding to clinically actionable variant interpretations. By integrating disease biology with rigorous functional assessment and analytical validation, this approach addresses the critical challenge of VUS resolution that currently limits the utility of genomic medicine. The standardized methodologies, performance benchmarks, and reagent solutions detailed in this guide empower researchers and clinical laboratories to implement robust variant assessment pipelines. As functional genomics technologies continue to advance, with MAVE methods becoming more accessible and comprehensive, this framework provides a foundation for generating the high-quality evidence needed to resolve variants of uncertain significance and ultimately deliver on the promise of precision medicine for diverse patient populations.
For researchers, scientists, and drug development professionals, navigating the U.S. regulatory landscape is fundamental to ensuring that diagnostic assays and tests are not only scientifically valid but also legally compliant for clinical use. Three key entities form the cornerstone of this landscape: the Food and Drug Administration (FDA), the Clinical Laboratory Improvement Amendments (CLIA) program, and the College of American Pathologists (CAP). While often mentioned together, their roles, jurisdictions, and requirements are distinct. CLIA sets the baseline federal standards for all laboratory testing, the FDA regulates medical devices including test kits and, until recently, sought to oversee Laboratory Developed Tests (LDTs), and CAP offers a voluntary, peer-based accreditation that often exceeds CLIA requirements [102] [103].
Understanding the interplay between these frameworks is critical for evaluating the specificity, sensitivity, and overall validity of functional assays. A robust regulatory strategy ensures that research data can be seamlessly translated into clinically actionable diagnostic tools, supporting both drug development and patient care.
Recent Regulatory Shifts: The Status of LDTs
A major recent development has been the legal reversal of the FDA's plan to actively regulate Laboratory Developed Tests (LDTs). On March 31, 2025, a US District Court judge nullified the FDA's final rule on LDT oversight, effectively vacating all associated requirements and guidance documents [104] [105]. This means laboratories are no longer required to comply with the phased FDA regulatory schedule that was set to begin in May 2025 [104]. Consequently, the primary regulatory framework for LDTs remains CLIA, supplemented by accreditation programs like CAP [106].
Comparative Analysis of Regulatory Bodies
The table below provides a structured comparison of the FDA, CLIA, and CAP, highlighting their distinct scopes and requirements.
Table 1: Key Characteristics of FDA, CLIA, and CAP
| Feature | FDA (Food and Drug Administration) | CLIA (Clinical Laboratory Improvement Amendments) | CAP (College of American Pathologists) |
|---|---|---|---|
| Primary Role | Regulates medical devices (including IVD test kits) for safety and effectiveness [107] [103]. | Sets federal quality standards for all human laboratory testing [102] [103]. | A voluntary, peer-driven accreditation program for laboratories [102] [103]. |
| Governing/Administering Body | U.S. Food and Drug Administration. | Centers for Medicare & Medicaid Services (CMS), with CDC and FDA involvement [102]. | College of American Pathologists. |
| Basis of Classification | Device risk (Intended use and risk of harm) into Class I, II, or III [108]. | Test complexity (Waived, Moderate, High) [102]. | Adherence to detailed, specialty-specific checklists that exceed CLIA standards [102]. |
| Key Focus | Premarket review (510(k), PMA), labeling, quality system manufacturing (QSR) [107]. | Personnel qualifications, quality control, proficiency testing (PT), quality assurance [102]. | Entire laboratory quality management system, analytical performance, and patient safety [103]. |
| Enforcement Mechanism | Approval or clearance for market; manufacturing inspections. | CLIA certificate required to operate; sanctions for non-compliance [102]. | Biannual inspections (on-site and self-inspection) to maintain accreditation status [102]. |
The Interrelationship of FDA, CLIA, and CAP
The following diagram illustrates how these regulatory and accreditation frameworks interact in the lifecycle of a diagnostic test, from conception to clinical use, particularly in the context of the recent LDT ruling.
Experimental Protocols for Regulatory Compliance
Adhering to regulatory standards requires implementing specific experimental and quality control protocols. The following workflows are essential for validating and maintaining compliance for diagnostic assays.
Protocol 1: Analytical Test Validation (CLIA/CAP Core Requirement)
This protocol establishes the fundamental performance characteristics of an assay, which is a requirement under CLIA for non-waived tests and is rigorously enforced by CAP accreditation [102] [106].
Table 2: Key Reagents and Materials for Analytical Validation
| Research Reagent/Material | Primary Function in Validation |
|---|---|
| Reference Standard | Provides a material of known concentration/activity to establish the assay's calibration and accuracy. |
| Characterized Panel of Clinical Samples | Used to determine specificity, sensitivity, and reportable range across diverse matrices (e.g., serum, plasma). |
| Quality Control (QC) Materials | Characterized samples at multiple levels (low, normal, high) for ongoing precision and reproducibility studies. |
| Interfering Substances | Substances like lipids, hemoglobin, or common drugs to test for assay interference, ensuring result reliability. |
Methodology:
- Precision/Repeatability: Run QC materials and patient samples over at least 20 days. Calculate within-run and between-run coefficients of variation (CV). CAP checklists require CVs to be within defined, medically acceptable limits.
- Reportable Range: Test a series of samples with known concentrations spanning the assay's potential range. Perform linear regression analysis to define the limits of linearity.
- Accuracy/Method Comparison: Run at least 40 patient samples using the new method and a reference or predicate method. Use correlation statistics (e.g., Passing-Bablok regression, Bland-Altman plots).
- Analytical Sensitivity (LoD): Test a low-level sample and a blank sample repeatedly (e.g., n=20). The LoD is typically the mean of the low-level sample + 2SD above the mean of the blank.
- Analytical Specificity/Interference: Spike samples with potential interferents and compare results to un-spiked controls. A significant shift indicates interference.
Protocol 2: Proficiency Testing (PT) as a Regulatory Tool
Proficiency Testing is a mandated CLIA requirement where labs receive unknown samples from an external provider, analyze them, and report results for grading against peer laboratories [109] [106]. Updated CLIA PT requirements took full effect in January 2025, making this protocol more critical than ever [109] [110].
Methodology:
- Selection & Enrollment: Enroll in a CAP-approved PT program for each regulated analyte and specialty/subspecialty [106].
- Routine Testing: Handle PT samples exactly as patient specimens, incorporating them into the routine workflow by staff who are unaware of their PT status.
- Analysis & Reporting: Report results within the defined timeline. The laboratory's performance is evaluated against the revised 2025 CLIA acceptance criteria [109].
- Corrective Action: Investigate any unacceptable PT results thoroughly. The root cause analysis and corrective action plan must be documented and are scrutinized during CAP inspections.
Table 3: Examples of Updated 2025 CLIA Proficiency Testing Acceptance Limits [109]
| Analyte | NEW 2025 CLIA Acceptance Criteria | OLD Criteria |
|---|---|---|
| Creatinine | Target Value (TV) ± 0.2 mg/dL or ± 10% (greater) | TV ± 0.3 mg/dL or ± 15% (greater) |
| Hemoglobin A1c | TV ± 8% | Not previously a regulated analyte |
| Potassium | TV ± 0.3 mmol/L | TV ± 0.5 mmol/L |
| Troponin I | TV ± 0.9 ng/mL or 30% (greater) | Not previously a regulated analyte |
| Total Protein | TV ± 8% | TV ± 10% |
| White Blood Cell Count | TV ± 10% | TV ± 15% |
The following diagram outlines the cyclical workflow for maintaining compliance through Proficiency Testing and quality management.
Implications for Specificity and Sensitivity Research
The regulatory frameworks of CLIA and CAP directly govern how the clinical performance of an assay—its specificity and sensitivity—must be established and monitored.
- Defining Clinical Validity: For an FDA submission, data on clinical sensitivity and specificity are required, often from large, multi-center trials. For a LDT under CLIA/CAP, the laboratory must establish these metrics during the initial validation phase using a well-characterized set of clinical samples, ensuring the test reliably distinguishes between patient populations [102].
- Ongoing Verification: CAP accreditation requires continuous monitoring of assay performance. Trends in QC data and PT results can signal drift that may affect the long-term sensitivity and specificity of the test, triggering preemptive investigation and recalibration [106].
- Impact of 2025 PT Changes: The updated, often stricter, CLIA PT criteria for 2025 [109] mean that assays must demonstrate higher levels of accuracy and precision. A method with poor specificity (leading to false positives) or suboptimal sensitivity (missing low-level positives) is more likely to produce unacceptable PT results, failing regulatory requirements and necessitating corrective action.
For the research and drug development community, a clear understanding of the FDA, CLIA, and CAP guidelines is not merely about regulatory compliance—it is a fundamental component of scientific rigor and assay quality. The recent court decision on LDTs has reaffirmed CLIA's central role as the regulatory baseline for laboratory testing, with CAP accreditation representing a gold standard for quality. By integrating the experimental protocols for test validation and proficiency testing into the research lifecycle, scientists can ensure that their assays for evaluating specificity, sensitivity, and functional responses are robust, reliable, and ready for clinical application, thereby effectively bridging the gap between innovative research and patient care.
Statistical Approaches for Determining Evidence Strength and Odds of Pathogenicity
In the field of clinical genomics, accurate interpretation of genetic variants stands as a major bottleneck in precision medicine. While sequencing technologies have advanced rapidly, distinguishing pathogenic variants from benign ones remains a significant challenge, leaving a substantial proportion of variants classified as variants of uncertain significance (VUS) [111] [112]. This guide compares contemporary statistical approaches for determining evidence strength and odds of pathogenicity, focusing on their performance in enhancing the specificity and sensitivity of variant classification within the context of functional assays research. As genomic data grows, robust statistical frameworks become increasingly critical for translating genetic findings into clinically actionable insights.
Comparative Analysis of Statistical Frameworks
The following analysis compares three prominent statistical approaches for variant pathogenicity assessment, evaluating their methodologies, applications, and performance characteristics relevant to researchers and clinical scientists.
Table 1: Comparison of Statistical Approaches for Pathogenicity Assessment
| Method Name | Core Principle | Data Inputs | Reported Performance | Primary Application Context |
|---|---|---|---|---|
| Combined Binomial Test [111] | Compares expected vs. observed allele frequency in patient cohorts using binomial tests. | - Patient cohort sequencing data- Normal population AF- Disease prevalence (Q) | - Power ↑ with cohort size & ↓ disease prevalence- Specificity remains ~100% [111] | Filtering benign variants, especially rare variants with low population AF, in Mendelian diseases. |
| Odds Ratio (OR) Enrichment [112] | Calculates variant-level ORs for disease enrichment in large biobanks, calibrated to ACMG/AMP guidelines. | - Large biobank data (e.g., UK Biobank)- Clinical endpoints/phenotypes | - OR ≥ 5.0 with lower 95% CI ≥ 1 suggests strong evidence (PS4) [112] | Providing population evidence for pathogenicity across actionable disorders; VUS reclassification. |
| Multi-Parametric Function Integration [65] | Integrates novel functional parameters (e.g., Vc, sDLCO) with traditional metrics to phenotype complex diseases. | - Traditional PFTs (FEV1, FVC)- Novel parameters (Vc, sDLNO/sDLCO) | - Vc had highest correlation to CT-emphysema (R²=0.8226)- RV + Vc model pseudo R²=0.667 [65] | Enhancing phenotyping for heterogeneous diseases like COPD; identifying destructive components. |
Experimental Protocols and Workflows
Protocol for the Combined Binomial Test
This protocol is designed to identify likely benign variants by comparing their observed frequency in a patient cohort against the expected frequency if they were pathogenic [111].
Experimental Workflow:
- Cohort Selection: Identify a patient cohort of size
nwith a confirmed Mendelian disease attributable to variants in geneg. - Data Acquisition:
- Obtain the Allele Frequency (AF =
qk) of variantakfrom a large normal population database (e.g., gnomAD). - Establish the disease prevalence (
Q) for the disorder from epidemiological literature.
- Obtain the Allele Frequency (AF =
- Statistical Testing (Recessive Disease Model):
- Test 1 (Left-tailed Binomial Test):
- Null Hypothesis (H0): The variant is pathogenic.
- Expected Occurrence: The count of allele
akin the patient cohort follows a Binomial distribution withN = 2 * ntrials and success ratep = qk / Q. - Test Execution: Perform
Binomial.test(X = x, N = 2n, p = qk/Q). A significant p-value (≤ 0.05) leads to rejecting H0, suggesting the variant is unlikely to be pathogenic.
- Test 2 (Right-tailed Binomial Test):
- Null Hypothesis (H0): The variant is benign.
- Expected Occurrence: The count of allele
akin the patient cohort follows a Binomial distribution withN = 2 * ntrials and success ratep = qk. - Test Execution: Perform
Binomial.test(X = x, N = 2n, p = qk). A significant p-value (≤ 0.05) leads to rejecting H0, suggesting the variant is unlikely to be benign.
- Test 1 (Left-tailed Binomial Test):
- Interpretation: The variant is considered "unlikely to be pathogenic" (likely benign) if Test 1 is significant (p ≤ 0.05) AND Test 2 is not significant (p > 0.05) [111].
Protocol for Odds Ratio Enrichment Analysis
This protocol uses large-scale biobank data to generate and calibrate evidence of pathogenicity based on variant enrichment in affected individuals [112].
Experimental Workflow:
- Biobank Data Curation: Obtain whole-exome or whole-genome sequencing data linked to clinical health records for a large population cohort (e.g., N > 400,000).
- Phenotype Definition: Define clear, specific case criteria for the disorder of interest (e.g., breast cancer, familial hypercholesterolemia) using diagnosis codes, medication records, and lab values. Control subjects should not meet these criteria.
- Variant Filtering & Annotation: Focus on rare (e.g., MAF < 0.1%), nonsynonymous variants in pre-specified actionable genes. Annotate variants using established databases.
- Association Analysis:
- For each variant, construct a 2x2 contingency table of variant presence/absence versus case/control status.
- Calculate the Odds Ratio (OR) and its 95% confidence interval for each variant.
- Evidence Calibration: Calibrate OR thresholds to ACMG/AMP evidence levels (e.g., supporting, moderate, strong). For example, an OR ≥ 5.0 with a lower 95% confidence bound ≥ 1 might be calibrated to provide strong evidence (PS4) [112].
- Integration: Combine this population evidence with other lines of evidence (e.g., computational, functional) for a final variant classification.
Table 2: Essential Research Reagents and Resources for Pathogenicity Assessment Studies
| Item/Resource | Function/Application | Example Tools/Databases |
|---|---|---|
| Population AF Databases | Provides allele frequency in control populations to filter common, likely benign variants. | gnomAD, 1000 Genomes [111] |
| Large Biobanks | Serves as an integrated source of genomic and phenotypic data for association studies and evidence extraction. | UK Biobank [112] |
| Variant Annotation Tools | Automates the functional prediction and annotation of genetic variants. | VEP, ANNOVAR |
| Statistical Software | Provides the computational environment for performing binomial tests, regression, and OR calculations. | R, Python (Pandas, NumPy, SciPy) [113] |
| Disease-Specific Cohorts | Well-phenotyped patient cohorts are essential for testing variant enrichment and validating statistical models. | ClinGen, in-house patient registries [111] |
| ACMG/AMP Framework | The standardized guideline for combining evidence and assigning final pathogenicity classifications. | ClinGen SVI Guidelines [112] |
The statistical approaches compared herein—the Combined Binomial Test, OR Enrichment, and Multi-Parametric Integration—each offer distinct methodologies for strengthening pathogenicity evidence. The Combined Binomial Test excels at filtering rare benign variants in Mendelian diseases, while OR Enrichment leverages large biobanks to provide calibrated population evidence. Integrating multiple functional parameters enhances phenotyping resolution for complex diseases. For researchers, the choice of method depends on the specific clinical question, data availability, and disease context. A multi-faceted approach, combining these robust statistical frameworks with functional assay data, provides the most powerful path forward for resolving VUS and advancing genomic medicine.
Implementing Orthogonal Assays to Confirm Findings and Increase Confidence
In scientific research and diagnostic development, the pursuit of reliable and reproducible data is paramount. Orthogonal assays provide a powerful strategy to achieve this goal by employing multiple, biologically independent methods to measure the same analyte or biological endpoint [114]. The core principle is that these methods utilize fundamentally different mechanisms of detection or quantification, thereby minimizing the chance that the same systematic error or interference will affect all results [115]. When findings from these disparate methods converge on the same conclusion, confidence in the data is significantly increased. This approach has gained strong traction in fields like drug discovery and antibody validation, and is often referenced in guidance from regulatory bodies, including the FDA, MHRA, and EMA, as a means to strengthen underlying analytical data [115] [114] [116].
The need for orthogonal testing is particularly acute in areas where false positives can have significant consequences. For instance, during the SARS-CoV-2 pandemic, orthogonal testing algorithms (OTAs) were evaluated to improve the specificity of serological tests, ensuring that positive IgG results were not due to cross-reactivity with other coronaviruses [116]. Similarly, in lead identification for drug discovery, an orthogonal assay approach serves to eliminate false positives or confirm the activity identified during a primary assay [115]. This guide will objectively compare different orthogonal assay strategies, their experimental protocols, and their performance in enhancing the specificity and sensitivity of research findings.
Key Principles and Comparative Advantages of Orthogonal Assays
Core Conceptual Framework
An orthogonal strategy moves beyond simple replication of an experiment. It involves cross-referencing antibody-based or other primary method results with data obtained using methods that are biologically and technically independent [114]. In statistics, "orthogonal" describes equations where variables are statistically independent; applied experimentally, it means the two methods are unrelated in their potential sources of error [114]. This independence is crucial. For example, a cell-based reporter assay and a protein-binding assay like AlphaScreen rely on completely different biological principles and readouts (luminescence vs. luminescent proximity) to probe the same biological interaction [117]. When they agree, it provides strong, multi-faceted evidence for the finding.
Comparative Analysis of Orthogonal vs. Traditional Single-Assay Approaches
The table below summarizes the key performance differentiators between orthogonal and single-assay approaches.
Table 1: Performance Comparison of Single-Assay vs. Orthogonal Assay Approaches
| Feature | Single-Assay Approach | Orthogonal Assay Approach | Comparative Advantage |
|---|---|---|---|
| Specificity | Susceptible to method-specific interferences (e.g., cross-reactivity) [116]. | Significantly improved by using methods with different selectivity profiles [116]. | Reduces false positives; PPV of a SARS-CoV-2 IgG test increased from 90.9% to 98.7% with an OTA [116]. |
| Data Confidence | Limited to the confidence interval of a single method. | High, as agreement between independent methods controls for bias and reinforces the conclusion [115] [114]. | Provides a robust foundation for critical decision-making in drug development and diagnostics. |
| Regulatory Alignment | May not meet specific guidance for confirmatory data. | Recommended by regulators (FDA, EMA) for strengthening analytical data [115]. | Positions research for smoother regulatory review and acceptance. |
| Risk Mitigation | High risk of undetected systematic error. | Mitigates risk of false findings due to assay-specific artifacts [114]. | Protects against costly late-stage failures based on erroneous early data. |
| Resource Investment | Lower initial cost and time. | Higher initial cost and time for developing/running multiple assays. | The upfront investment is offset by increased trust in results and reduced follow-up on false leads. |
Experimental Protocols for Orthogonal Assays
Protocol 1: Orthogonal Antibody Validation for Western Blot
This protocol, adapted from Cell Signaling Technology, details the use of public transcriptomic data to orthogonally validate an antibody for Western Blot (WB) [114].
Orthogonal Data Mining:
- Identify the target protein (e.g., Nectin-2/CD112).
- Query a public database such as the Human Protein Atlas using the gene name (e.g., ENSG00000130202-NECTIN2) to access RNA normalized expression (nTPM) data across various cell lines [114].
- Select candidate cell lines based on the orthogonal RNA data: choose at least two with high expected expression and two with low/undetectable expected expression. For Nectin-2, RT4 and MCF7 (high) and HDLM-2 and MOLT-4 (low) were selected [114].
Binary Experimental Setup (Antibody-Dependent Method):
- Culture the selected cell lines under standard conditions.
- Prepare protein extracts from each cell line.
- Perform Western Blot analysis using the antibody under validation (e.g., Nectin-2/CD112 (D8D3F) #95333) alongside a loading control (e.g., β-Actin) [114].
Analysis and Validation:
- The antibody is considered specific for WB if the protein expression pattern (high in RT4/MCF7, low in HDLM-2/MOLT-4) strongly correlates with the orthogonal RNA expression data from the Human Protein Atlas [114].
Protocol 2: Orthogonal Screening for Transcription Factor Inhibitors
This protocol describes a two-tiered orthogonal screen to identify small-molecule inhibitors of the transcription factor YB-1 [117].
Primary Screen: Cell-Based Luciferase Reporter Assay
- Objective: Measure interference with YB-1's transcriptional activation function.
- Method:
- Transfert cells (e.g., HCT116) with a plasmid (e.g., pGL4.17-E2F1-728) where a YB-1-responsive promoter drives firefly luciferase expression [117].
- Dispense cells into a 384-well plate.
- Add small-molecule compounds from a library (e.g., 7360 compounds).
- After incubation (e.g., 36 hours), add a luciferase substrate (e.g., SteadyGlo) and measure luminescence. A reduction indicates a potential inhibitor [117].
Orthogonal Confirmatory Screen: AlphaScreen Protein-Binding Assay
- Objective: Confirm hits by measuring direct interference with YB-1 binding to its DNA target.
- Method:
- Conjugate anti-YB-1 antibody to AlphaScreen acceptor beads.
- Set up reactions in 96-well plates containing purified YB-1 protein and potential inhibitory compounds.
- After incubation, add the antibody-conjugated beads and a biotinylated ssDNA oligonucleotide containing the YB-1 binding site.
- Finally, add streptavidin-coated donor beads. If YB-1 binds the DNA, the beads are brought into proximity, producing a luminescent signal. Inhibition of binding reduces this signal [117].
- Compounds that show activity in both the luciferase (cellular) and AlphaScreen (biochemical) assays are considered high-confidence putative YB-1 inhibitors [117].
Protocol 3: Orthogonal Algorithm for SARS-CoV-2 Serology
This clinical diagnostic protocol uses two immunoassays against different viral targets to confirm seropositivity [116].
First-Line Test:
- Perform a qualitative IgG immunoassay against the viral nucleocapsid (N) protein (e.g., Abbott SARS-CoV-2 IgG assay) [116].
- All negative results are considered final. All initially positive results proceed to the second-line test.
Second-Line Test:
- Test the initially positive samples with a second, independent immunoassay targeting a different viral protein, such as the spike (S) protein (e.g., a laboratory-developed ELISA) [116].
- A sample is considered confirmed positive only if it is positive in both the first-line (anti-N) and second-line (anti-S) tests. This two-step algorithm dramatically improves the positive predictive value (PPV) of the final reported result [116].
Experimental Data and Performance Comparison
The quantitative performance of different orthogonal strategies is summarized in the table below.
Table 2: Performance Data from Orthogonal Assay Implementations
| Application / Assay Combination | Sensitivity (Primary/Orthogonal) | Specificity (Primary/Orthogonal) | Key Outcome |
|---|---|---|---|
| SARS-CoV-2 Serology [116]• 1st: Abbott IgG (N protein)• 2nd: LDT ELISA (S protein) | 96.4% / 100% | 99.0% / 98.4% | OTA confirmed 80% (78/98) of initial positives, drastically reducing false positives. |
| YB-1 Inhibitor Screening [117]• Primary: Luciferase Reporter• Orthogonal: AlphaScreen | N/A | N/A | Identified 3 high-confidence inhibitors from a 7360-compound library, demonstrating efficient hit confirmation. |
| Antibody Validation (Nectin-2) [114]• Orthogonal: RNA-seq data• Primary: Western Blot | N/A | N/A | Successfully correlated protein expression with independent RNA data, confirming antibody specificity. |
Visualization of Workflows and Signaling Pathways
Orthogonal Assay Strategy Workflow
The following diagram illustrates the general decision-making logic employed in a typical orthogonal assay strategy, integrating examples from the cited protocols.
Orthogonal Antibody Validation Pathway
This diagram details the specific workflow for validating an antibody using orthogonal data, as demonstrated in the Nectin-2 example [114].
Table 3: Key Reagents and Resources for Orthogonal Assay Development
| Item / Resource | Function / Description | Example Use Case |
|---|---|---|
| Public Data Repositories | Provide antibody-independent data (e.g., RNA expression, proteomics) for orthogonal comparison [114]. | Human Protein Atlas, CCLE, DepMap Portal used to select cell lines for antibody validation [114]. |
| AlphaScreen Technology | A bead-based proximity assay for detecting biomolecular interactions in a microtiter plate format [117]. | Used as an orthogonal biochemical assay to confirm inhibition of YB-1 binding to DNA [117]. |
| Luciferase Reporter System | A cell-based assay that measures transcriptional activity via luminescence output. | Served as the primary screen for YB-1 transcription factor inhibitors [117]. |
| Validated Antibodies | Reagents that have been rigorously tested for specificity in defined applications using strategies like orthogonal validation. | CST's Nectin-2/CD112 antibody was validated for WB using RNA-seq data as an orthogonal method [114]. |
| Purified Recombinant Protein | Isolated protein of interest for use in biochemical assays. | Essential for the YB-1 AlphaScreen assay to test direct binding interference [117]. |
| Cell Line Panels | A collection of characterized cell lines with known genetic and molecular profiles. | Used in binary validation strategies to test antibody performance across high/low expressors [114]. |
In the fields of drug discovery and biomedical research, the selection of an optimal assay format is a critical determinant of experimental success. Assay benchmarking is the systematic process of comparing and evaluating the performance of different assay technologies against standardized criteria and reference materials to identify the most suitable platform for specific research objectives [118]. This process is fundamental to a broader thesis on evaluating specificity and sensitivity in functional assays, as it provides the empirical framework needed to ensure that research data is reliable, reproducible, and capable of supporting robust scientific conclusions [119].
The pharmaceutical industry faces significant challenges due to irreproducible preclinical research, which can lead to compound failures in clinical trials despite promising early data [119]. Implementing rigorous benchmarking practices addresses these challenges by providing objective evidence of assay performance before critical resources are committed. For researchers and drug development professionals, selecting an assay technology without comprehensive benchmarking introduces substantial risks, including false positives/negatives, inefficient resource allocation, and ultimately, compromised research outcomes [120] [121]. This guide provides a structured approach to assay benchmarking, incorporating quantitative performance metrics, standardized experimental protocols, and decision-support frameworks to enable optimal assay selection across diverse research scenarios.
Key Performance Metrics for Assay Comparison
When comparing different assay formats and technologies, researchers must evaluate specific quantitative metrics that collectively define assay performance and suitability for intended applications. These metrics provide objective criteria for direct comparison between alternative platforms and establish whether a given assay meets the minimum requirements for reliability and precision in specific research contexts.
Critical Quantitative Metrics:
EC₅₀ and IC₅₀ Values: These values represent the concentration of a compound that produces 50% of its maximum effective response (EC₅₀) or inhibitory response (IC₅₀) [121]. They are fundamental for ranking compound potency during early-stage drug discovery. Lower EC₅₀/IC₅₀ values indicate greater potency. It is crucial to recognize that these values are not constants but can vary significantly between different assay technologies, making them essential comparator metrics when evaluating commercial assay offerings [121].
Signal-to-Background Ratio (S/B): Also known as Fold-Activation (F/A) in agonist-mode assays or Fold-Reduction (F/R) in antagonist-mode assays, this ratio normalizes raw data by comparing the receptor-specific signal from test compound-treated wells to the background signal from untreated wells [121]. A high S/B ratio indicates a strong functional response that clearly distinguishes above basal noise levels, which is a hallmark of a robust assay, particularly for agonist-mode screens [121].
Z'-Factor (Z'): This statistical parameter assesses assay suitability for screening applications by incorporating both standard deviation and signal-to-background variables into a single unitless measure ranging from 0 to 1 [121]. Assays with Z' values between 0.5 and 1.0 are considered of good-to-excellent quality and suitable for high-throughput screening, while values below 0.5 indicate poor quality suffering from high variability, low S/B, or both, rendering them unsuitable for screening purposes [121].
Table 1: Key Quantitative Metrics for Assay Benchmarking
| Metric | Definition | Interpretation | Optimal Range |
|---|---|---|---|
| EC₅₀ / IC₅₀ | Compound concentration producing 50% of maximal effect [121] | Measures compound potency; lower values indicate greater potency | Varies by target; consistent for reference compounds |
| Signal-to-Background (S/B) | Ratio of test compound signal to background signal [121] | Induces assay robustness and ability to detect true signals | >3:1 (minimum); higher values preferred |
| Z'-Factor | Statistical measure incorporating both S/B and variability [121] | Assesses assay quality and suitability for screening | 0.5-1.0 (suitable for HTS) |
Additional Performance Considerations: Beyond these core metrics, assay sensitivity (the lowest detectable concentration of an analyte) and specificity (the ability to distinguish between similar targets) are fundamental to assay capability [122]. Furthermore, researchers should evaluate robustness (resistance to small, deliberate variations in method parameters) and reproducibility (consistency of results across multiple runs, operators, and instruments) [119]. These characteristics ensure that an assay will perform reliably in different laboratory settings and over time, which is particularly important for long-term research projects and multi-site collaborations.
Benchmarking Methodologies and Experimental Design
Implementing a structured benchmarking process ensures consistent, comparable results across different assay technologies. The following methodology, adapted from established benchmarking principles and tailored specifically for assay comparison, provides a rigorous framework for evaluation [118] [119].
The Benchmarking Process
A systematic, multi-stage approach to assay benchmarking minimizes bias and ensures all relevant performance aspects are evaluated:
Identify Specific Benchmarking Objectives: Clearly define the scientific questions the assay must answer and the key performance requirements [119]. Document whether the assay will be used for primary screening, mechanism-of-action studies, or diagnostic development, as each application has distinct requirements for throughput, sensitivity, and precision.
Select Appropriate Benchmarking Partners: Identify and acquire relevant assay technologies for comparison, which may include commercial kits, internally developed assays, or emerging technologies [118]. Selection should consider factors including the assay's detection mechanism (e.g., luminescence, fluorescence, colorimetry), required instrumentation, and compatibility with existing laboratory workflows.
Collect and Analyze Standardized Data: Using standardized reference materials and validated protocols, generate comparable performance data across all assay platforms [118] [122]. This stage should include testing against well-characterized control compounds with known response profiles to establish baseline performance metrics for each platform.
Compare and Evaluate Performance: Systematically analyze collected data using the key metrics outlined in Section 2, identifying relative strengths and weaknesses of each platform [118]. This comparative analysis should extend beyond pure performance numbers to include practical considerations such as required hands-on time, cost per sample, and compatibility with automation systems.
Implement Improvements and Select Optimal Format: Based on benchmarking results, refine assay protocols or select the best-performing technology for the intended application [118]. Document all benchmarking procedures and outcomes to support future technology evaluations and provide justification for assay selection decisions.
Statistical Rigor and Experimental Design
Robust benchmarking requires careful experimental design to generate statistically meaningful results. The Assay Capability Tool, developed through collaboration between preclinical statisticians and scientists, provides a framework of 13 critical questions that guide proper assay development and validation [119]. Key considerations include:
Managing Variation: Identify and control for sources of variability through appropriate experimental design techniques such as randomization, blocking, and blinding [119]. Understanding the major sources of variation in an assay is critical to achieving required precision in key endpoints.
Sample Size Determination: Ensure sufficient replication to detect biologically relevant effects with appropriate statistical power [119]. Sample size calculations should be based on the assay's known variability in the specific laboratory where it will be run, rather than relying exclusively on historical precedent or published values.
Quality Control and Monitoring: Implement procedures to monitor assay performance over time, using quality control charts to track the consistency of controls and standards [119]. This ongoing monitoring is essential for detecting changing conditions that may affect result interpretation.
Table 2: Essential Research Reagent Solutions for Assay Benchmarking
| Reagent Category | Specific Examples | Function in Benchmarking |
|---|---|---|
| Quantified Reference Materials | QUANTDx pathogen panels (fungal, respiratory, STI) [122] | Provide standardized, quantified targets for assessing assay sensitivity, specificity, and limit of detection |
| Validated Control Compounds | Compounds with established EC₅₀/IC₅₀ values [121] | Enable normalization across platforms and verification of potency measurements |
| Cell-Based Assay Systems | Luciferase-based reporter assays [121] | Facilitate functional assessment of biological pathways and compound effects |
| Detection Reagents | ATP assay consumables, luciferase substrates [123] [121] | Generate measurable signals for quantifying biological responses |
Comparative Analysis of Major Assay Technologies
Different assay technologies offer distinct advantages and limitations depending on the research context. The following comparison highlights key characteristics of major assay formats relevant to drug discovery and development.
Table 3: Comparative Analysis of Major Assay Technologies
| Assay Technology | Key Advantages | Key Limitations | Optimal Application Context |
|---|---|---|---|
| Cell-Based Assays | Functional relevance, pathway analysis capability [120] | Higher variability, more complex protocols [121] | Target validation, mechanism of action studies [120] |
| ATP Assays | Universal cell viability measure, high sensitivity [123] | Limited to metabolic activity readout | High-throughput screening, cytotoxicity testing [123] |
| Luminometric Assays | High sensitivity, broad dynamic range [123] | Signal stability issues, reagent costs | Reporter gene assays, low abundance targets |
| Enzymatic Assays | Cost-effective, straightforward protocols | Lower sensitivity compared to luminescence | Enzyme kinetic studies, high-volume screening |
Technology-Specific Considerations:
Cell-Based Assays: These platforms provide physiologically relevant data by measuring functional responses in living systems, making them invaluable for studying complex biological pathways and therapeutic mechanisms [120]. The cell-based ATP assay segment is experiencing significant growth (approximately 8% annually), driven by its ability to deliver quantitative, reproducible results with minimal sample preparation, particularly in high-throughput workflows [123].
ATP Assays: As valued tools in viability and cytotoxicity assessment, ATP assays market is expanding steadily, with the U.S. market projected to grow from USD 1.6 billion in 2025 to USD 3.1 billion by 2034 at a CAGR of 7.6% [123]. These assays are particularly valuable in pharmaceutical quality control, where they are increasingly integrated into drug production workflows for contamination control and sterility assurance [123].
Emerging Trends: The assay technology landscape is evolving toward increased automation, miniaturization, and multiplexing capabilities [120] [123]. Leading vendors are focusing on developing compact assay formats that allow simultaneous measurement of multiple cellular parameters, reducing reagent consumption while increasing throughput [123]. Furthermore, integration of AI-powered platforms providing predictive analytics and automated anomaly detection is becoming more prevalent in top pharmaceutical research laboratories [123].
Decision Framework for Assay Selection
Selecting the optimal assay technology requires matching technical capabilities with specific research requirements and constraints. The following decision framework provides a structured approach to assay selection based on benchmarking data.
Scenario-Based Recommendations:
High-Throughput Compound Screening: For applications requiring rapid screening of large compound libraries, prioritize assays with robust Z' factors (>0.5), high signal-to-background ratios, and compatibility with automation systems [121]. Cell-based assays optimized for high-throughput screening with minimal hands-on time are particularly valuable in this context, with luminometric detection often providing the required sensitivity and dynamic range [123].
Mechanism of Action Studies: When investigating detailed biological mechanisms or pathway interactions, focus on cell-based assays that provide functional relevance and pathway analysis capability [120]. These applications may sacrifice some throughput for biological relevance, making more complex assay systems potentially appropriate if they provide richer biological insights.
Diagnostic Assay Development: For diagnostic applications, emphasize reproducibility, sensitivity, and specificity, often requiring rigorous validation using standardized reference materials [122]. Assays must demonstrate consistent performance across multiple lots and operators, with well-established stability profiles.
Resource-Constrained Environments: In academic or startup settings with limited budgets, consider factors including initial instrumentation costs, reagent expenses, and required technical expertise [120]. In these contexts, enzymatic assays or simpler colorimetric methods may provide the most practical solution despite potential limitations in sensitivity.
Implementation Strategy: After selecting an assay technology, develop a comprehensive protocol detailing study objectives, key endpoints, experimental design, analysis methods, and a timetable of activities [119]. This protocol should specify methods to control variation (e.g., randomization, blocking, blinding) and include predefined criteria for the inclusion/exclusion of experimental units, processing of raw data, treatment of outliers, and statistical analysis approaches [119].
Assay benchmarking represents a critical foundation for rigorous biological research and effective drug development. By implementing a systematic approach to technology comparison—incorporating quantitative performance metrics, standardized experimental protocols, and scenario-based decision frameworks—researchers can make informed selections that align assay capabilities with specific research objectives. The evolving landscape of assay technologies, characterized by increasing automation, miniaturization, and data integration capabilities, offers exciting opportunities to enhance research productivity and reliability [120] [123].
As the field advances toward more predictive and physiologically relevant models, the importance of robust benchmarking practices will only increase. By establishing rigorous comparison standards and validation frameworks today, researchers contribute to the broader scientific goal of enhancing research reproducibility and translation of preclinical findings to clinical success [119]. Through the disciplined application of the principles outlined in this guide, scientists can navigate the complex assay technology landscape with confidence, selecting optimal platforms that generate reliable, actionable data to advance their research objectives.
Conclusion
A rigorous, multi-faceted approach to evaluating sensitivity and specificity is fundamental to developing functional assays that yield reliable and actionable data. Mastering the foundational principles, applying robust methodological practices, proactively troubleshooting, and adhering to structured validation frameworks are all critical for success. The future of functional assays lies in the continued integration of automation, advanced data management, and the development of more physiologically relevant models, such as 3D cell cultures. By embracing these comprehensive evaluation strategies, researchers can significantly accelerate drug discovery, improve diagnostic accuracy, and ultimately enhance patient outcomes in biomedical and clinical research.
References
- 1. Analytical vs Diagnostic Sensitivity and Specificity [https://www.immqas.org.uk/news/analytical-vs-clinical-sensitivity-and-specificity/]
- 2. the meaning of these terms in analytical and diagnostic settings [https://pubmed.ncbi.nlm.nih.gov/8992938/]
- 3. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 4. How do analytical, diagnostical, and functional sensitivity differ? [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/sensitivities]
- 5. Specificity in Preclinical Drug Development Models [https://emulatebio.com/specificity-in-preclinical-drug-development-models-organ-chips/]
- 6. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 7. Molecular Diagnostics - Part 5: Analytical Sensitivity and ... [https://blog.seracare.com/molecular-serology-blog/verification-part5]
- 8. Getting Sensitive: Diagnostic Sensitivity and Specificity ... [https://bitesizebio.com/44620/getting-sensitive-diagnostic-sensitivity-and-specificity-simplified/]
- 9. Assay Optimization 101: Enhancing Sensitivity, Specificity, ... [https://dispendix.com/blog/assay-optimization-101-enhancing-sensitivity-specificity-and-reproducibility]
- 10. Behavior of test specificity under an imperfect gold standard [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125893/]
- 11. Assay Validation - Cytometry [https://cytometry.mlsascp.com/assay-validation.html]
- 12. Model and Assay Validation and Acceptance - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK424977/]
- 13. Comparative diagnostic accuracy studies with an imperfect ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01255-4]
- 14. Functional assays provide a robust tool for the clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5539989/]
- 15. Integration of functional assay data results provides strong ... [https://www.nature.com/articles/s41436-020-00991-0]
- 16. False positives and false negatives [https://en.wikipedia.org/wiki/False_positives_and_false_negatives]
- 17. Thresholds and the confusion matrix | Machine Learning [https://developers.google.com/machine-learning/crash-course/classification/thresholding]
- 18. Confusion matrix [https://en.wikipedia.org/wiki/Confusion_matrix]
- 19. Receiver operating characteristic curve: overview and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8831439/]
- 20. Strategic publishing: Comparing Journals - Library guides [https://libguides.victoria.ac.nz/strategic-publishing/comparing-journals]
- 21. Research Tools and Resources [https://www.fda.gov/drugs/science-and-research-drugs/research-tools-and-resources]
- 22. Understanding and using sensitivity, specificity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2636062/]
- 23. Sensitivity, Specificity, and Predictive Values: Foundations, ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2017.00307/full]
- 24. Sensitivity and Specificity - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/sensitivity-and-specificity]
- 25. Trade off between sensitivity and specificity [https://medium.com/@abhi.roop18/trade-off-between-sensitivity-and-specificity-ada8e92800f5]
- 26. Sensitivity and Specificity: A Complete Guide [https://www.datacamp.com/tutorial/sensitivity-specificity-complete-guide]
- 27. Statistics | Sensitivity, Specificity, PPV and NPV [https://geekymedics.com/sensitivity-specificity-ppv-and-npv/]
- 28. The “Testy” Test Characteristics Part II: Positive Predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10293502/]
- 29. 統計學和醫學中的貝葉斯(Bayes)推理 [https://unaettie.com/zh-tw/pz/bayes_math.php]
- 30. Why PPV and NPV Should be Considered When Setting ... [https://qservegroup.com/blog/en/why-ppv-and-npv-should-be-considered-when-setting-sensitivity-and-specificity-requirements]
- 31. Prevalence - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK430867/]
- 32. Positive and negative predictive values [https://en.wikipedia.org/wiki/Positive_and_negative_predictive_values]
- 33. 诊断性研究中的ROC曲线分析 [https://www.lcgdbzz.org/en/custom/news/id/6991]
- 34. Estimating sensitivity and specificity from positive predictive ... [https://www.sciencedirect.com/science/article/abs/pii/S0195670108001047]
- 35. 阴性预测值(NPV)等指标及置信区间计算(附R语言代码) [https://blog.csdn.net/Mrrunsen/article/details/128806053]
- 36. Standardization of Negative Controls in Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4206554/]
- 37. Positive and Negative Controls [https://www.rockland.com/resources/positive-and-negative-controls/?srsltid=AfmBOooVTSj6fRPjndeHNLhfrvykUTw5XbmW6_kJD8OyCoIB1Bju4mDb]
- 38. Positive and negative controls for antibody validation [https://www.euromabnet.com/guidelines/positive-negative-controls.php]
- 39. SPR vs ELISA | Comparing techniques for biomolecular ... [https://nicoyalife.com/blog/spr-vs-elisa-comparing-techniques-for-biomolecular-detection/]
- 40. Comparison of in-house enzyme-linked immunosorbent ... [https://pubmed.ncbi.nlm.nih.gov/39111714]
- 41. The How and Why of Limit of Detection [https://bitesizebio.com/44092/how-to-calculate-the-limit-of-detection-for-an-assay-and-why-youd-want-to/]
- 42. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 43. Sensitivity and Limit of Detection [https://www.sciencedirect.com/science/article/abs/pii/S092234870870220X]
- 44. Limit of Detection | National Exposure Report [https://www.cdc.gov/environmental-exposure-report/php/about-the-data/limit-of-detection.html]
- 45. Comparison of approaches for assessing detection and ... [https://www.nature.com/articles/s41598-024-83474-5]
- 46. Sensitivity analysis of limit of detection estimation using ... [https://pubmed.ncbi.nlm.nih.gov/41240387/]
- 47. Method Detection Limit - Frequent Questions [https://www.epa.gov/cwa-methods/method-detection-limit-frequent-questions]
- 48. Specificity and Cross-Reactivity - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK2396/]
- 49. Solutions to immunoassay interference, cross reactivity and ... [https://www.gyrosproteintechnologies.com/spinblog/immunoassay-interference-crossreactivity-challenges]
- 50. Cross-Reactivity - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/cross-reactivity]
- 51. Sample Size, Replicability, and Pre-Test Likelihoods ... [https://pubmed.ncbi.nlm.nih.gov/37125444/]
- 52. What do we mean by 'replication' and 'validation' in ... [https://pubmed.ncbi.nlm.nih.gov/18931511/]
- 53. Replication and validation in -omics studies - just as ... [https://simplystatistics.org/posts/2012-07-03-replication-and-validation-in-omics-studies-just-as/]
- 54. Extended sample size calculations for evaluation of prediction ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02592-4]
- 55. Sample size in quantitative instrument validation studies [https://www.sciencedirect.com/science/article/pii/S2405844022035113]
- 56. Cell-based Assays Market | USD 45.16 Billion by 2034 [https://www.novaoneadvisor.com/report/cell-based-assays-market]
- 57. Cell Based Assays 2025-2033 Trends: Unveiling Growth ... [https://www.archivemarketresearch.com/reports/cell-based-assays-140048]
- 58. Choosing Between Immunoassays and Molecular Assays [https://ifyber.com/choosing-immunoassays-v-molecular-assays/]
- 59. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 60. Comparative Analysis of RT-PCR and a Colloidal Gold ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154499/]
- 61. Comparative Diagnostic Evaluation of Real-Time PCR and ... [https://www.medrxiv.org/content/10.1101/2025.08.26.25334225v1]
- 62. Comparison of three multiplex immunoassays for ... [https://www.nature.com/articles/s41598-025-23579-7]
- 63. Comparison of false positive and false negative rates ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2023.1132128/full]
- 64. 1 Data visualization - R for Data Science (2e) - Hadley Wickham [https://r4ds.hadley.nz/data-visualize.html]
- 65. Sensitivity and specificity of various lung function ... [https://pubmed.ncbi.nlm.nih.gov/40659254/]
- 66. Lot-to-Lot Variation - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6223607/]
- 67. Lot-to-Lot Variance in Immunoassays—Causes, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10252387/]
- 68. Antibody Critical Reagents: Challenges and Risks in Their ... [https://www.labcorp.com/education-events/articles/antibody-critical-reagents-challenges-and-risks-their-lifecycle-management]
- 69. Analysis of Reagent Lot-to-Lot Comparability Tests in Five ... [http://www.annclinlabsci.org/content/42/2/165.full]
- 70. Managing Reagent Lot to Lot Variability [https://myadlm.org/science-and-research/clinical-chemistry/clinical-chemistry-trainee-council/pearls-of-laboratory-medicine-in-english/2015/managing-reagent-lot-to-lot-variability]
- 71. Ligand Binding Assay Critical Reagents and Their Stability [https://pmc.ncbi.nlm.nih.gov/articles/PMC4012044/]
- 72. Biological Reagents 2025-2033 Analysis: Trends, ... [https://www.datainsightsmarket.com/reports/biological-reagents-196921]
- 73. Bayesian statistical approaches to drug product variability ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517322005920]
- 74. ELISA Development and Optimization [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/elisa-development-optimization.html]
- 75. Enzyme Linked Immunosorbent Assay - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK555922/]
- 76. Troubleshooting and Optimizing a Western Blot [https://blog.addgene.org/troubleshooting-and-optimizing-a-western-blot]
- 77. Comprehensive Optimization of Western Blotting - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10453944/]
- 78. qPCR primer design revisited [https://www.sciencedirect.com/science/article/pii/S221475351730181X]
- 79. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 80. Model: Bayesian Optimisation for Biology | Imperial - iGEM 2025 [https://2025.igem.wiki/imperial/Model]
- 81. A comprehensive review of competitive lateral flow assays ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc01075b]
- 82. A practical deep learning model for core temperature ... [https://www.sciencedirect.com/science/article/abs/pii/S0306456525000361]
- 83. What is Matrix Interference and How Does It Affect Testing? [https://www.arborassays.com/what-is-matrix-interference/?srsltid=AfmBOoo641mc0a_Bz1iL6lZjwIhzLJInOVZkIKblRTfNCTHzEYNSjCqj]
- 84. Biological Matrix Effects in Quantitative Tandem Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4695332/]
- 85. Matrix Effects on Quantitation in Liquid Chromatography [https://www.chromatographyonline.com/view/matrix-effects-on-quantitation-in-liquid-chromatography-sources-and-solutions]
- 86. Antibody Surface Coverage Drives Matrix Interference in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8741144/]
- 87. Overcoming Matrix Effects in Non-Target Screening [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224152/]
- 88. Matrix Effects—A Challenge toward Automation of ... [https://www.sciencedirect.com/science/article/pii/S1535553510000158]
- 89. Recent progress on media for biological sample preparation [https://www.sciencedirect.com/science/article/abs/pii/S0021967324006678]
- 90. Matrix isolation with an ion transfer device for interference ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914016306622]
- 91. U.S. ATP Assay Market Trend Analysis Report 2025-2034: [https://www.globenewswire.com/news-release/2025/09/26/3156854/28124/en/U-S-ATP-Assay-Market-Trend-Analysis-Report-2025-2034-Precision-Medicine-Adoption-and-Regulatory-Changes-Pharma-Biotech-Dominate-with-Increasing-Demand-for-Cell-Based-Assays.html]
- 92. How to ensure lab reproducibility with automation [https://automata.tech/blog/how-to-ensure-lab-reproducibility-with-automation/]
- 93. Lab Automation in R&D: Why Adaptability Is the New ... [https://www.labmanager.com/lab-automation-in-r-d-why-adaptability-is-the-new-throughput-34116]
- 94. Diagnostic Labs Market Research and Forecast 2025-2030 [https://finance.yahoo.com/news/diagnostic-labs-market-research-forecast-100800370.html]
- 95. Best Test Automation Tools: Complete Enterprise Platform ... [https://www.virtuosoqa.com/post/best-test-automation-tools-complete-enterprise-platform-comparison-guide]
- 96. A detailed comparison of top Automation testing Tools (2025) [https://www.browserstack.com/guide/automated-test-tools-comparison]
- 97. Top 12 Test Automation Tools of 2025 [https://www.accelq.com/blog/test-automation-tools/]
- 98. Creating an atlas of variant effects to resolve variants of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12434709/]
- 99. Clinical Variant Interpretation: 5 Easy Tiers [https://lifebit.ai/blog/clinical-variant-interpretation-complete-guide/]
- 100. Functional evaluation and clinical classification of BRCA2 ... [https://www.nature.com/articles/s41586-024-08388-8]
- 101. HTS Assay Validation - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK83783/]
- 102. CLIA, COLA & CAP: What's the Difference? [https://www.bioagilytix.com/blog/clia-cola-cap-whats-the-difference/]
- 103. CLIA and CAP: What You Need to Know [https://www.foregenomics.com/blog/clia-cap?srsltid=AfmBOooZPQBupC6RCZhXPxhNNwUN1tSMavulKbYKAA_1ItgJZZaJ-JLg]
- 104. April 8, 2025 [https://www.cap.org/advocacy/latest-news-and-practice-data/april-8-2025]
- 105. Laboratory Developed Tests [https://www.fda.gov/medical-devices/in-vitro-diagnostics/laboratory-developed-tests]
- 106. Regulatory News and Updates for Laboratories [https://www.cap.org/laboratory-improvement/regulatory-news-and-updates-for-laboratories]
- 107. FDA and CLIA Compliant Lab Equipment: 2025 Updates ... [https://labequipmentdirect.com/blogs/regulatory-and-compliance/fda-clia-compliant-lab-equipment?srsltid=AfmBOopXLqqMNlS4QbL1A5TW8_bMD47wqXlKNoOuGBACGIhHWla_WqHe]
- 108. Top 5 Takeaways on FDA LDT Risk Classification [https://www.cap.org/member-resources/articles/top-5-takeaways-on-fda-ldt-risk-classification]
- 109. 2025 CLIA Acceptance Limits for Proficiency Testing [https://www.westgard.com/clia-a-quality/quality-requirements/2024-clia-requirements.html]
- 110. 2025 Changes to Point-of-Care Testing Regulatory ... [https://myadlm.org/education/point-of-care-testing-professional-certification/the-point/articles/2025/may]
- 111. A novel statistical method for interpreting the pathogenicity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7796914/]
- 112. Extracting and calibrating evidence of variant pathogenicity ... [https://www.sciencedirect.com/science/article/pii/S0002929725002435]
- 113. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 114. Antibody Validation Essentials: Orthogonal Strategy - CST Blog [https://blog.cellsignal.com/hallmarks-of-validation-orthogonal-strategy]
- 115. Improving Therapeutics Discovery with Orthogonal Assay ... [https://revvitysignals.com/article/blog/improving-therapeutics-discovery-orthogonal-assay-data]
- 116. Evaluation of Orthogonal Testing Algorithm for Detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7499512/]
- 117. Orthogonal assays for the identification of inhibitors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6804448/]
- 118. Understanding Benchmarking Analysis: A Step-by- ... [https://www.comparables.ai/articles/understanding-benchmarking-analysis-step-by-step-guide]
- 119. Helping to drive the robustness of preclinical research [https://pmc.ncbi.nlm.nih.gov/articles/PMC4520620/]
- 120. Top Cell-based Assay Companies & How to Compare ... [https://www.linkedin.com/pulse/top-cell-based-assay-companies-how-compare-them-2025-0bhme/]
- 121. Understanding Assay Performance Metrics [https://indigobiosciences.com/understanding-assay-performance-metrics/]
- 122. Reference Materials – Benchmark Assay Performance with ... [https://microbix.com/products/reference-materials/]
- 123. U.S. ATP Assay Market Analysis & Outlook 2025–2034 [https://www.gminsights.com/industry-analysis/us-atp-assay-market]