Functional Validation of Genetic Variants: From VUS to Pathogenicity in Biomedical Research
This article provides a comprehensive guide to the functional validation of genetic variants for researchers and drug development professionals.
Functional Validation of Genetic Variants: From VUS to Pathogenicity in Biomedical Research
Abstract
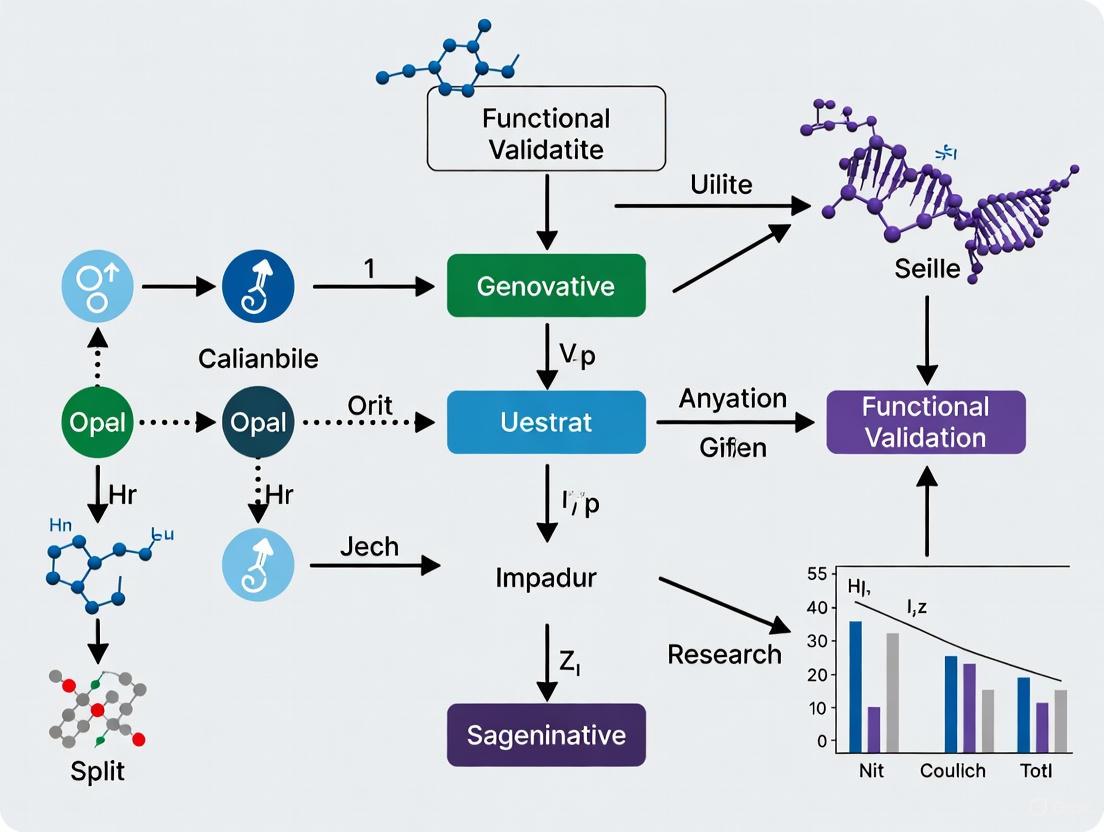
This article provides a comprehensive guide to the functional validation of genetic variants for researchers and drug development professionals. It covers the critical challenge of interpreting Variants of Uncertain Significance (VUS) discovered via next-generation sequencing and outlines a complete workflow from foundational concepts to advanced applications. The content explores established and emerging methodological approaches, including specific biochemical, cellular, and computational assays. It also addresses common troubleshooting and optimization strategies for validation pipelines and concludes with frameworks for rigorous validation and comparative analysis to ensure results are clinically actionable and reproducible.
The VUS Challenge: Establishing the Need for Functional Validation
Defining Variants of Uncertain Significance (VUS) and Their Clinical Impact
A Variant of Uncertain Significance (VUS) is a genetic alteration for which the impact on health and disease risk is currently unknown [1]. These variants represent a significant bottleneck in clinical genetics, as they cannot be definitively classified as either pathogenic or benign based on existing evidence. The high likelihood that a newly observed variant will be a VUS has made interpretation of genetic variants a substantial challenge in clinical practice [2]. Furthermore, variants identified in individuals of non-European ancestries are often confounded by the limited diversity of population databases, causing substantial inequity in diagnosis and treatment [3] [2].
The American College of Medical Genetics and Genomics (ACMG), the Association for Molecular Pathology (AMP), and the Association for Clinical Science (ACGS) have established standard guidelines for interpreting variants, introducing clear categories: benign, likely benign, pathogenic, likely pathogenic, and VUS [1]. These classifications are based on multiple factors including population data, computational predictions, functional evidence, and segregation data. As of October 2024, the majority of variants associated with rare diseases in the ClinVar database were categorized as VUS, highlighting the critical need for improved classification strategies [1].
Clinical Challenges and Impact of VUS
Prevalence and Reclassification Rates
VUS prevalence varies significantly across populations, with underrepresented groups often experiencing higher rates due to limited representation in genomic databases [3]. The table below summarizes key findings from recent studies on VUS prevalence and reclassification:
Table 1: VUS Prevalence and Reclassification Data from Recent Studies
| Study Population | VUS Prevalence | Reclassification Rate | Key Findings | Citation |
|---|---|---|---|---|
| Levantine HBOC patients | 40% of participants had non-informative results (VUS) | 32.5% of VUS reclassified | 4 VUS upgraded to Pathogenic/Likely Pathogenic; median of 4 total VUS per patient | [3] |
| Seven tumor suppressor genes (NF1, TSC1, etc.) | 128 unique VUS from 145 carriers | 31.4% reclassified as Likely Pathogenic using new criteria | STK11 showed highest reclassification rate (88.9%) | [4] |
| TP53 germline variants (Li-Fraumeni syndrome) | Specific rate not provided | Updated specifications led to clinically meaningful classifications for 93% of pilot variants | New Bayesian-informed approach reduced VUS rates and increased certainty | [5] |
Psychological and Clinical Management Challenges
The disclosure of uncertain genetic results exacerbates the psychological burden associated with genetic testing. Ambiguous testing results are associated with negative patient reactions including:
- Over-interpretation and anxiety about disease risk
- Frustration and hopelessness regarding preventive measures
- Decisional regret about treatment choices [3]
Studies show that participants with uncertain results have higher difficulty understanding and recalling the outcome of their genetic tests [3]. Negative reactions are particularly prevalent in cancer patients, possibly due to heightened anxiety about the disease, uncertainty in decision-making regarding treatment or prophylactic surgery, and the emotional burden of hereditary risks [3].
From a clinical management perspective, VUS create significant challenges for:
- Treatment decisions: Physicians are often hesitant to implement aggressive preventive measures based on VUS results
- Family screening: Relatives cannot be effectively tested for a VUS with unclear significance
- Resource utilization: VUS require ongoing reinterpretation and tracking, consuming substantial healthcare resources
Misinterpretation of VUS as pathogenic or benign variants is common, resulting in erroneous expectations of their clinical impact [3]. This highlights the critical need for improved functional validation strategies to resolve VUS classifications.
Experimental Approaches for VUS Resolution
Single-Cell Multi-Omic Technologies
Single-cell DNA–RNA sequencing (SDR-seq) is a recently developed technology that enables simultaneous profiling of up to 480 genomic DNA loci and genes in thousands of single cells [6]. This method allows accurate determination of coding and noncoding variant zygosity alongside associated gene expression changes, providing a powerful platform to dissect regulatory mechanisms encoded by genetic variants.
Table 2: Key Research Reagent Solutions for Functional Genomics
| Research Reagent | Function/Application | Utility in VUS Resolution | |
|---|---|---|---|
| Tapestri Technology (Mission Bio) | Microfluidic platform for single-cell multi-omics | Enables high-throughput targeted DNA and RNA sequencing at single-cell resolution | [6] |
| Prime Editing Systems | Precise genome editing without double-strand breaks | Scalable introduction of variants in endogenous genomic context for functional assessment | [7] |
| gnomAD Database | Population frequency data for genetic variants | Provides essential allele frequency data for PM2/BS1 ACMG criteria application | [3] [5] |
| REVEL & SpliceAI | In silico prediction algorithms | Computational prediction of variant deleteriousness and splice effects | [4] |
| ClinGen ER (Evidence Repository) | Centralized database for variant evidence | Enables collaborative curation and evidence sharing across institutions | [5] |
SDR-seq Experimental Workflow:
- Cell Preparation: Cells are dissociated into a single-cell suspension, fixed with paraformaldehyde or glyoxal, and permeabilized
- In Situ Reverse Transcription: Custom poly(dT) primers add unique molecular identifiers (UMIs), sample barcodes, and capture sequences to cDNA molecules
- Droplet Generation: Cells containing cDNA and gDNA are loaded onto the Tapestri platform for first droplet generation
- Cell Lysis: Cells are lysed and treated with proteinase K, then mixed with reverse primers for each intended gDNA or RNA target
- Second Droplet Generation: Forward primers with capture sequence overhangs, PCR reagents, and barcoding beads are introduced
- Multiplexed PCR: Amplification of both gDNA and RNA targets within each droplet enables cell barcoding
- Library Preparation: Sequencing-ready libraries are generated with distinct overhangs for gDNA and RNA targets to optimize sequencing [6]
This methodology enables highly sensitive detection of DNA and RNA targets across thousands of single cells in a single experiment, with minimal cross-contamination between cells (<0.16% for gDNA, 0.8-1.6% for RNA) [6].
Multiplexed Assays of Variant Effect (MAVEs)
Multiplexed Assays of Variant Effect (MAVEs) enable scalable functional assessment of nearly all possible coding variants in a target sequence, offering a proactive approach to resolving VUS [8]. These high-throughput methods systematically measure the functional impact of thousands of variants in parallel, creating comprehensive maps of variant effects.
Prime Editing MAVE Protocol:
- Platform Development: Establish a pooled prime editing platform in HAP1 cells to assay variants in their endogenous genomic context
- pegRNA Optimization: Design and test prime editing guide RNA (pegRNA) configurations for efficient variant installation
- Cell Enrichment: Implement co-selection strategies for edited cells and include surrogate targets to enhance data quality
- Selection Screening:
- Negative Selection: Screen for loss-of-function variants by measuring depletion of efficiently installed variants (e.g., >7,500 pegRNAs targeting SMARCB1)
- Positive Selection: Identify functional variants under selective pressure (e.g., 6-thioguanine selection for MLH1 LoF variants)
- Variant Assessment: Test both coding and non-coding variants, including a high proportion of all possible single nucleotide variants (SNVs) in target regions [7]
This platform has demonstrated high accuracy for discriminating pathogenic variants, making it valuable for identifying new disease-associated variants across large genomic regions [7].
Updated Variant Classification Frameworks
Recent advances in variant classification include updated, quantitative frameworks that incorporate Bayesian approaches and gene-specific specifications:
ClinGen TP53 VCEP v2 Specifications:
- Population Data (PM2): Updated thresholds for variant rarity (PM2 allele frequency < 0.00003) with adjustments for clonal hematopoiesis by examining variant allele fraction (VAF > 0.35)
- Functional Data (PS3/BS3): Incorporation of quantitative likelihood ratios from multiplexed functional assays
- Phenotype Evidence (PP4): Reintroduction of phenotype specificity criteria with modified scoring based on disease-specific diagnostic yields
- Computational Evidence (PP3/BP4): Updated thresholds for REVEL (≥0.7 for PP3, <0.2 for BP4) and SpliceAI (≥0.2 for PP3, <0.1 for BP4) predictions [4] [5]
New ClinGen PP1/PP4 Criteria: The updated PP1/PP4 criteria incorporate a point-based system that assigns higher scores based on phenotype specificity when phenotypes are highly specific to the gene of interest [4]. This approach has demonstrated significant improvements in VUS reclassification rates, particularly for tumor suppressor genes with characteristic phenotypes such as NF1, TSC1/TSC2, and STK11 [4].
Emerging Solutions and Future Directions
International Standards and Data Sharing
The ClinGen/AVE Functional Data Working Group, comprising over 25 international members from academia, government, and industry, is developing more definitive guidelines for genetic variant classification [2]. Key objectives include:
- Developing clear, robust guidelines acceptable to clinical diagnostic scientists and clinicians
- Fostering partnerships with Variant Curation Expert Panels (VCEPs) to enable utilization of multiplexed functional data
- Providing educational outreach to ensure MAVE data accessibility and clinical uptake [2]
Major initiatives like the Atlas of Variant Effects (AVE) Alliance are working to systematize the clinical validation of functional assay data, though challenges remain in funding labor-intensive curation efforts and developing flexible approaches to assay validation [2].
Computational and Modeling Approaches
Advanced computational methods are increasingly important for VUS interpretation:
- Machine Learning Models: Decision trees, SVM, and random forests for structured data classification tasks
- Deep Learning Models: CNNs and RNNs for large-scale unstructured data, though requiring substantial computational resources
- Mathematical Modeling: Equations and algorithms to simulate medical outcomes and biological behavior, with approximately 21% of recent medical manuscripts utilizing mathematical modeling approaches [1]
These computational approaches are particularly valuable for interpreting the functional impact of non-coding variants, which constitute over 90% of genome-wide association study variants for common diseases but remain challenging to assess [6].
The resolution of Variants of Uncertain Significance (VUS) represents a critical challenge in modern genomic medicine, with significant implications for patient diagnosis, risk assessment, and clinical management. Recent advances in single-cell multi-omics, multiplexed functional assays, and updated classification frameworks are substantially improving our ability to resolve these ambiguous variants. The development of international standards through initiatives like the AVE Alliance and implementation of quantitative, Bayesian-informed approaches to variant classification are further accelerating progress in this field.
As these technologies and frameworks continue to evolve, they promise to reduce diagnostic odysseys for patients with rare diseases, improve equity in genomic medicine across diverse populations, and ultimately enhance the clinical utility of genetic testing across a broad spectrum of human diseases.
Next-generation sequencing (NGS) has revolutionized molecular diagnostics, providing an unparalleled capacity to detect millions of genetic variants rapidly and cost-effectively [9]. This technology has transformed disease diagnosis, particularly in oncology and rare genetic disorders, by moving beyond single-gene tests to comprehensive multigene analysis and whole-exome or whole-genome sequencing [9] [10]. However, a critical diagnostic limitation persists: the detection of a genetic variant does not automatically elucidate its functional or pathological significance. The vast majority of variants identified through NGS are classified as variants of uncertain significance (VUS), creating profound challenges for clinical interpretation and patient management [11]. This application note examines the inherent limitations of NGS-based identification and establishes why functional validation represents an indispensable next step for translating genomic findings into clinically actionable insights, particularly within the context of drug development and personalized therapeutic strategies.
Table 1: Core Limitations of NGS in Clinical Diagnostics
| Limitation Category | Specific Challenge | Impact on Diagnostic Interpretation |
|---|---|---|
| Variant Classification | High rate of Variants of Uncertain Significance (VUS) | Inconclusive test results, preventing definitive diagnosis and management [11] |
| Technical Constraints | Short-read limitations in complex genomic regions | Incomplete or inaccurate variant calling in repetitive, homologous, or structurally complex areas [9] |
| Contextual Interpretation | Inability to determine variant impact on protein function | Known variants may be detected, but their pathological effect on gene/protein activity remains unknown [11] |
| Data Integration | Lack of robust, validated functional databases | Difficulties in matching novel variants to established phenotypic patterns without functional correlates [12] |
Key Limitations of NGS in Clinical Diagnostics
The Challenge of Variant Interpretation and VUS
The primary challenge in clinical NGS application lies not in variant detection, but in biological interpretation. The American College of Medical Genetics and Genomics (ACMG) and the Association for Molecular Pathology (AMP) have established guidelines for variant classification, which include criteria for functional evidence [11]. Despite this framework, differences in the application of functional evidence codes (PS3/BS3) remain a significant source of discordance between laboratories [11]. The fundamental issue is that NGS identifies sequence changes but cannot discern whether those changes are pathogenic, benign, or functionally neutral without additional evidence. This diagnostic uncertainty directly impacts patient care, as clinicians cannot base definitive treatment or surveillance strategies on VUS findings.
Technical and Analytical Constraints
NGS technologies, particularly dominant short-read platforms, face inherent technical limitations that affect diagnostic comprehensiveness. Short-read sequencing (50-600 base pairs) struggles with complex genomic regions containing repetitive sequences, paralogous genes, or structural variations [9]. These limitations can lead to ambiguous mapping, coverage gaps, and false positives/negatives in variant calling. While long-read sequencing technologies (e.g., SMRT, Nanopore) address some of these issues by generating reads thousands of base pairs long, they have historically faced higher error rates and are not yet the clinical standard [9]. Furthermore, NGS assays require complex bioinformatic pipelines for data analysis, and variations in these pipelines, coupled with a lack of standardized validation approaches across laboratories, can lead to inconsistent results [12].
The Critical Role of Functional Validation
Functional validation moves beyond sequence observation to experimentally determine the biochemical consequences of a genetic variant. It bridges the gap between variant identification and understanding its role in disease pathogenesis.
Establishing a Framework for Functional Evidence
The ClinGen Sequence Variant Interpretation (SVI) Working Group has developed a refined, structured framework for evaluating functional data for clinical variant interpretation [11]. This framework provides critical guidance for applying the PS3/BS3 evidence codes and involves a four-step process:
- Define the disease mechanism (e.g., loss-of-function, gain-of-function).
- Evaluate the applicability of general classes of assays used in the field.
- Evaluate the validity of specific assay instances, including design, controls, and statistical rigor.
- Apply evidence to individual variant interpretation.
This process emphasizes that a "well-established" functional assay must be robustly validated with a sufficient number of known pathogenic and benign control variants to demonstrate its predictive power. It is estimated that a minimum of 11 total pathogenic and benign variant controls are required to achieve moderate-level evidence in the absence of rigorous statistical analysis [11].
Integrated Approaches for Variant Resolution
Cutting-edge research now combines NGS with advanced computational and experimental methods to resolve VUS. For example, a 2025 study on Colombian colorectal cancer patients integrated NGS with artificial intelligence to identify pathogenic germline variants [10]. The researchers used the BoostDM AI model to identify oncodriver germline variants with potential implications for disease progression, achieving an area under the curve (AUC) of 0.803 for the genes in their panel, demonstrating high predictive accuracy [10]. This highlights how AI can prioritize variants for functional testing. Furthermore, for non-coding or splice-site variants, the same study employed minigene assays for functional validation, which successfully revealed the generation of aberrant transcripts, thereby clarifying the molecular etiology of the disease [10]. The integration of NGS, AI, and functional assays represents a powerful, multi-faceted approach to overcoming the diagnostic limitations of NGS alone.
Experimental Protocols for Functional Validation
Protocol: Saturation Genome Editing (SGE) for Functional Variant Assessment
Saturation Genome Editing (SGE) is a high-throughput method that uses CRISPR-Cas9 and homology-directed repair (HDR) to introduce exhaustive nucleotide modifications at a specific genomic locus, enabling the functional assessment of nearly all possible variants in a gene while preserving their native genomic context [13].
Table 2: Research Reagent Solutions for Saturation Genome Editing
| Reagent/Material | Function/Description |
|---|---|
| HAP1-A5 Cells | Near-haploid human cell line that facilitates the functional study of recessive alleles [13]. |
| CRISPR-Cas9 System | RNA-guided genome editing system comprising Cas9 nuclease and single-guide RNA (sgRNA) for targeted DNA cleavage. |
| Variant Library | A complex pool of DNA templates (donor oligos) designed to introduce every possible single nucleotide variant or amino acid substitution in the target exon. |
| NGS Library Prep Kit | Reagents for preparing sequencing libraries from the amplified target region post-selection to determine variant frequencies. |
Detailed Methodology:
Library and sgRNA Design:
- Design a library of donor oligonucleotides encompassing all possible nucleotide substitutions at the target genomic region(s).
- Design and validate a highly efficient sgRNA that cleaves adjacent to the target site for efficient HDR.
Cell Transduction and Editing:
- Transduce HAP1-A5 cells with the Cas9/sgRNA ribonucleoprotein (RNP) complex and the variant library donor templates.
- Allow time for HDR-mediated integration of the variant library into the native genomic locus.
Selection and Harvest:
- Apply a functional selection pressure that enriches for cells with wild-type (or mutant) protein activity, or use a fluorescence-activated cell sorting (FACS)-based assay to separate cell populations based on phenotype.
- Harvest genomic DNA from the pre-selection population and the post-selection population(s).
NGS Library Preparation and Analysis:
- Amplify the target genomic region from all population samples via PCR and prepare NGS libraries.
- Sequence the libraries on a high-throughput NGS platform.
- Quantify the abundance of each variant in the pre- and post-selection samples. A significant depletion of a variant after selection indicates a deleterious functional impact.
The workflow for this functional validation protocol is systematic and high-throughput, as illustrated below:
Protocol: Minigene Splicing Assay for Intronic Variants
The minigene assay is a powerful method to experimentally determine the impact of intronic or exonic variants on mRNA splicing, a common disease mechanism that is often difficult to predict computationally.
Detailed Methodology:
Vector and Construct Design:
- Clone a genomic fragment of interest (containing the exon with its flanking intronic sequences, including the variant under investigation) into an exon-trapping vector (e.g., pSPL3).
- Create two constructs: one with the wild-type sequence and one with the patient-derived mutant sequence.
Cell Transfection and RNA Harvest:
- Transfect the wild-type and mutant minigene constructs into a suitable mammalian cell line (e.g., HEK293T).
- Incubate for 24-48 hours to allow for transcription and splicing.
- Harvest total RNA from the transfected cells and perform reverse transcription to generate cDNA.
PCR and Analysis:
- Amplify the cDNA using vector-specific primers that flank the cloned insert.
- Analyze the PCR products by gel electrophoresis. Splicing patterns will appear as bands of different sizes.
- Sequence the individual PCR bands to confirm the exact exon-intron structure and identify aberrant splicing events (e.g., exon skipping, intron retention, cryptic splice site usage).
The logical flow for validating splicing defects is as follows:
The diagnostic limitation of NGS is unequivocal: identification is not synonymous with understanding. To realize the full promise of precision medicine, the research and clinical diagnostics communities must adopt an integrated framework that couples comprehensive genomic sequencing with rigorous functional validation. The experimental protocols and frameworks outlined here, including SGE and minigene assays, provide a pathway to resolve VUS, refine clinical classifications, and generate biologically meaningful data. For drug development professionals, this integrated approach is particularly critical, as targeting a genetically defined patient population with a therapy requires high confidence in the pathogenicity of the targeted variant. Moving forward, the continued development, standardization, and implementation of high-throughput functional assays will be essential to bridge the gap between genomic discovery and actionable clinical insight, ultimately ensuring that NGS fulfills its potential as a transformative diagnostic tool.
The 2015 guidelines from the American College of Medical Genetics and Genomics and the Association for Molecular Pathology (ACMG/AMP) established a standardized framework for interpreting sequence variants in Mendelian disorders [14]. Within this framework, functional studies represent a powerful form of evidence, categorized under the strong evidence codes PS3 and BS3. The PS3 code supports pathogenicity for "well-established" functional assays demonstrating a variant has abnormal gene/protein function, while BS3 supports benignity for assays showing normal function [15] [11].
Despite their potential, the original guidelines provided limited detailed guidance on how to evaluate functional assays, leading to significant inconsistencies in their application across clinical laboratories [15] [16] [11]. This document outlines structured protocols and application notes for implementing functional evidence criteria within the ACMG/AMP framework, providing researchers and clinicians with standardized approaches for assay validation and variant interpretation.
Theoretical Framework: Validating Functional Assays
The Four-Step Evaluation Framework
The Clinical Genome Resource (ClinGen) Sequence Variant Interpretation (SVI) Working Group developed a provisional four-step framework to determine the appropriate strength of evidence for functional assays [15] [11]. This systematic approach ensures that experimental data cited in clinical variant interpretation meets baseline quality standards.
Step 1: Define the disease mechanism - Precise understanding of the molecular basis of disease is foundational. This includes determining whether the disorder results from loss-of-function or gain-of-function mechanisms, the relevant protein domains and critical functional regions, and the appropriate model systems that recapitulate the disease biology [15] [11].
Step 2: Evaluate the applicability of general classes of assays - Researchers should assess how closely the assay reflects the biological environment, whether it captures the full spectrum of protein function, and the technical parameters including throughput, quantitative output, and dynamic range [15].
Step 3: Evaluate the validity of specific instances of assays - This involves rigorous validation of individual assay implementations through statistical analysis of performance metrics, inclusion of appropriate control variants, and demonstration of reproducibility across experimental replicates [15] [11].
Step 4: Apply evidence to individual variant interpretation - Finally, validated assays are applied to variant classification, with careful consideration of whether the evidence strength should be supporting, moderate, or strong based on the assay's validation data and performance characteristics [15].
Minimum Control Requirements for Evidence Strength
The stringency of evidence applied to functional data (supporting, moderate, or strong) depends heavily on the number and quality of control variants used during assay validation. The SVI Working Group performed quantitative analyses to establish minimum control requirements.
Table 1: Minimum Control Requirements for Functional Evidence Strength
| Evidence Strength | Minimum Control Variants | Pathogenic Controls | Benign Controls | Statistical Requirements |
|---|---|---|---|---|
| Supporting | 6 total | ≥3 pathogenic | ≥3 benign | No rigorous statistical analysis required |
| Moderate | 11 total | ≥5 pathogenic | ≥5 benign | OR ≥3 with 95% CI ≥1.5 in case-control studies |
| Strong (PS3/BS3) | 18 total | ≥9 pathogenic | ≥9 benign | Robust statistical validation with high confidence intervals |
The SVI Working Group determined that a minimum of 11 total pathogenic and benign variant controls are required to reach moderate-level evidence in the absence of rigorous statistical analysis [15] [11]. For strong-level evidence (the traditional PS3/BS3 criteria), more extensive validation with approximately 18 well-characterized control variants is recommended [15].
Practical Implementation: Gene-Specific Specifications
PALB2 Case Study: Limitations on Functional Evidence
The Hereditary Breast, Ovarian and Pancreatic Cancer (HBOP) Variant Curation Expert Panel (VCEP) developed gene-specific specifications for PALB2, demonstrating how general ACMG/AMP guidelines require refinement for individual genes.
Table 2: PALB2-Specific Modifications to ACMG/AMP Functional Evidence Criteria
| ACMG/AMP Code | Original Definition | PALB2-Modified Application | Rationale |
|---|---|---|---|
| PS3 | Well-established functional studies supportive of damaging effect | Not used for any variant type | Lack of known pathogenic missense variants for assay validation |
| BS3 | Well-established functional studies show no damaging effect | Not used for any variant type | Same rationale as PS3 |
| PM1 | Located in mutational hot spot/well-established functional domain | Not used | Missense pathogenic variation not confirmed as disease mechanism |
| BP4 | Multiple lines of computational evidence suggest no impact | Not used for missense variants | Supportive evidence only for in-frame indels/extension codes |
For PALB2, the HBOP VCEP recommended against using PS3, BS3, and several other codes entirely due to the lack of established pathogenic missense variants needed for functional assay validation [17]. This conservative approach highlights the critical importance of gene-disease mechanism understanding when applying functional evidence criteria.
Experimental Protocols for Validated Functional Assays
Splicing Assay Protocol
Purpose: To experimentally determine the impact of genomic variants on mRNA splicing patterns.
Methodology:
- RNA Extraction: Isolate high-quality RNA from patient-derived cells (lymphocytes, fibroblasts, or tissue-specific cell types) using commercial RNA extraction kits with DNase I treatment to remove genomic DNA contamination.
- cDNA Synthesis: Perform reverse transcription using gene-specific primers or random hexamers with controls to ensure no genomic DNA amplification.
- PCR Amplification: Design primers spanning the exonic region of interest with appropriate positive and negative controls. Include samples from known pathogenic splice variants, benign controls, and wild-type references.
- Product Analysis: Separate PCR products by capillary electrophoresis or agarose gel electrophoresis; quantify aberrant vs. normal splicing ratios; confirm novel splice products by Sanger sequencing.
Interpretation Criteria: >10% aberrant splicing compared to wild-type constitutes abnormal splicing; <5% is considered within normal technical variation; results between 5-10% require additional supporting evidence [17].
Functional Complementation Assay Protocol
Purpose: To assess the functional impact of variants in DNA repair genes like PALB2 through rescue of DNA damage sensitivity.
Methodology:
- Cell Line Establishment: Use PALB2-deficient mammalian cell lines with demonstrated sensitivity to DNA damaging agents (e.g., mitomycin C).
- Vector Construction: Clone wild-type and variant PALB2 cDNA into mammalian expression vectors with selectable markers; verify sequence integrity.
- Transfection & Selection: Transfect PALB2-deficient cells with wild-type, variant, and empty vector controls; select stable pools or clones using appropriate antibiotics.
- Viability Assessment: Treat cells with increasing concentrations of DNA damaging agents; measure cell viability by MTT assay or colony formation after 5-7 days; normalize to untreated controls.
Interpretation Criteria: Variants demonstrating <20% of wild-type rescue activity are considered functionally abnormal; variants with >60% activity are considered functionally normal; intermediate values (20-60%) require additional evidence [17].
Research Reagent Solutions for Functional Studies
Table 3: Essential Research Reagents for Functional Assays
| Reagent Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Cell Lines | PALB2-deficient mammalian cells (e.g., EUFA1341), HEK293T, Patient-derived lymphoblastoids | Provide cellular context for functional complementation and splicing assays | Verify authenticity by STR profiling; monitor mycoplasma contamination |
| Expression Vectors | Mammalian cDNA expression vectors (e.g., pCMV6, pCDH), Minigene splicing constructs (e.g., pSPL3) | Express wild-type and variant sequences in cellular models | Include selectable markers; verify cloning by full insert sequencing |
| DNA Damage Agents | Mitomycin C, Olaparib, Cisplatin, Hydrogen Peroxide | Challenge DNA repair pathways to assess functional impact | Titrate concentrations carefully; include dose-response curves |
| Antibodies | PALB2-specific antibodies, BRCA2 antibodies for co-immunoprecipitation, Loading control antibodies (e.g., GAPDH, Tubulin) | Detect protein expression, localization, and interactions | Validate specificity using knockout cell lines; optimize dilution factors |
Data Integration and Evidence Synthesis
Integrating Functional Evidence with Other Data Types
Functional evidence should never be interpreted in isolation. The ACMG/AMP framework provides specific guidance on combining functional data with other evidence types to reach variant classifications.
The integration of functional evidence with clinical and genetic data follows specific rules within the ACMG/AMP framework. For example, functional data may be combined with population data (PM2/BS1), computational predictions (PP3/BP4), segregation data (PP1), and de novo observations (PS2) to strengthen variant classification [17] [14]. However, circular reasoning must be avoided—functional data should not be combined with the same patient's clinical data (PP4) if that clinical data was used to establish the assay's clinical validity [15].
Current Challenges and Future Directions
Despite standardization efforts, significant challenges remain in the consistent application of functional evidence. A recent consultation identified several barriers to effective use of functional evidence in variant classification, including inaccessibility of published data, lack of standardization across assays, and difficulties in integrating functional data into clinical workflows [18].
Future directions focus on developing higher-throughput functional assays, creating centralized databases for functional data, and establishing more quantitative frameworks for evidence integration. Multiplex Assays of Variant Effect (MAVEs) show particular promise for systematically measuring the functional impact of thousands of variants in parallel [18].
The evolution of functional evidence application continues, with the recent retirement of the ClinGen Sequence Variant Interpretation Working Group in April 2025 and the transition to consolidated variant classification guidance [19]. This transition represents the maturation of variant interpretation standards and the integration of functional evidence into mainstream clinical practice.
Functional evidence remains a powerful component of variant classification within the ACMG/AMP framework when applied systematically and with appropriate validation. The protocols and specifications outlined here provide researchers and clinical laboratories with standardized approaches for implementing functional evidence criteria, ultimately leading to more consistent and accurate variant interpretation across the genetics community. As functional technologies continue to evolve, these guidelines will require ongoing refinement to incorporate new assay methodologies and expanding validation datasets.
The advent of high-throughput sequencing technologies has revolutionized molecular genetics, enabling the rapid identification of millions of genetic variants. However, a significant bottleneck has emerged in distinguishing causal disease variants from benign background variation. Functional genomics addresses this challenge by moving beyond correlation to establish causation, providing the experimental evidence needed to determine the pathological impact of genetic variants. In the clinical interpretation of variants identified through whole exome or whole genome sequencing (WES/WGS), the majority fall into the category of "variants of unknown significance" (VUS), creating uncertainty for diagnosis and treatment [20]. The American College of Medical Genetics and Genomics (ACMG) has established the PS3/BS3 criterion as strong evidence for variant classification, but differences in applying these functional evidence codes have contributed to interpretation discordance between laboratories [11]. This framework outlines standardized approaches for functional validation of genetic variants, providing researchers with clear protocols to bridge the gap between variant discovery and clinical application.
Quantitative Landscape of Functional Genomics
Outcomes from Genomic Sequencing Studies
Table 1: Distribution of Possible Outcomes from WES/WGS Analyses
| Outcome Number | Variant Type | Gene Association | Phenotype Match | Diagnostic Certainty |
|---|---|---|---|---|
| 1 | Known disease-causing variant | Known disease gene | Matching | Definitive diagnosis |
| 2 | Unknown variant | Known disease gene | Matching | Likely diagnosis (requires validation) |
| 3 | Known variant | Known disease gene | Non-matching | Uncertain significance |
| 4 | Unknown variant | Known disease gene | Non-matching | Uncertain significance |
| 5 | Unknown variant | Gene not associated with disease | Unknown | Uncertain significance |
| 6 | No explanatory variant found | N/A | N/A | No diagnosis |
Current data indicates that in the majority of investigations (approximately 60-75%), WES or WGS does not yield a definitive genetic diagnosis, primarily due to the challenge of VUS interpretation [20]. The success of functional genomics lies in its ability to reclassify these VUS into definitive diagnostic categories.
Evidence Thresholds for Functional Validation
Table 2: Control Requirements for Functional Assay Evidence Strength
| Evidence Strength | Minimum Pathogenic Controls | Minimum Benign Controls | Total Variant Controls | Statistical Requirement |
|---|---|---|---|---|
| Supporting | 2 | 2 | 4 | Not required |
| Moderate | 5 | 6 | 11 | Not required |
| Strong | 8 | 9 | 17 | Not required |
| Very Strong | 12 | 13 | 25 | Not required |
The Clinical Genome Resource (ClinGen) Sequence Variant Interpretation Working Group has established these minimum control requirements to standardize the application of the PS3/BS3 ACMG/AMP criterion [11]. These thresholds ensure that functional evidence meets a baseline quality level before being applied in clinical variant interpretation.
Advanced Methodologies in Functional Genomics
Single-Cell DNA–RNA Sequencing (SDR-seq)
Protocol: SDR-seq for Functional Phenotyping of Genomic Variants
Principle: SDR-seq simultaneously profiles genomic DNA loci and gene expression in thousands of single cells, enabling accurate determination of coding and noncoding variant zygosity alongside associated transcriptional changes [6].
Workflow:
Cell Preparation:
- Dissociate cells into a single-cell suspension.
- Fix cells using paraformaldehyde (PFA) or glyoxal (glyoxal is preferred for reduced nucleic acid cross-linking).
- Permeabilize cells to allow reagent entry.
In Situ Reverse Transcription:
- Perform reverse transcription using custom poly(dT) primers.
- Primers add a Unique Molecular Identifier (UMI), sample barcode, and capture sequence to cDNA molecules.
Droplet Generation and Lysis:
- Load cells onto microfluidic platform (e.g., Tapestri from Mission Bio).
- Generate first droplet emulsion.
- Lyse cells within droplets using proteinase K treatment.
Multiplexed PCR Amplification:
- Mix cell lysate with reverse primers for each gDNA and RNA target.
- Generate second droplet containing forward primers with capture sequence overhang, PCR reagents, and barcoding beads with cell barcode oligonucleotides.
- Perform multiplexed PCR to co-amplify gDNA and RNA targets.
Library Preparation and Sequencing:
- Break emulsions and pool amplification products.
- Use distinct overhangs on gDNA (R2N) and RNA (R2) reverse primers to separate and prepare NGS libraries.
- Sequence gDNA libraries for full-length variant information and RNA libraries for transcript expression quantification.
Validation: In proof-of-concept experiments, SDR-seq detected 82% of gDNA targets (23 of 28) with high coverage across the majority of cells, while RNA targets showed varying expression levels consistent with expected patterns [6]. The method demonstrates minimal cross-contamination (<0.16% for gDNA, 0.8-1.6% for RNA) and scales effectively to panels of 480 simultaneous targets.
CRISPR Editing and Transcriptomic Profiling
Protocol: Functional Validation of VUS Using CRISPR in Cell Models
Principle: Introduction of specific VUS into cell lines using CRISPR-Cas9 followed by genome-wide transcriptomic profiling to identify disease-relevant pathway disruptions [21].
Workflow:
Guide RNA Design and Synthesis:
- Design sgRNAs flanking the genomic location of the VUS.
- Include homologous repair templates containing the specific nucleotide change.
- Synthesize and validate sgRNAs and repair templates.
Cell Transfection and Selection:
- Transfect HEK293T or other relevant cell lines with Cas9-sgRNA ribonucleoprotein complexes and repair templates.
- Apply antibiotic selection (e.g., puromycin) 48 hours post-transfection.
- Isolate single-cell clones by serial dilution or fluorescence-activated cell sorting (FACS).
Genotype Validation:
- Expand single-cell clones for 2-3 weeks.
- Extract genomic DNA and perform PCR amplification of the target region.
- Confirm precise editing via Sanger sequencing or next-generation sequencing.
Functional Phenotyping:
- Passage validated clones and analyze using RNA-seq for transcriptomic profiling.
- Process RNA-seq data through bioinformatic pipelines for quality control, alignment, and differential expression analysis.
- Perform gene set enrichment analysis (GSEA) and pathway analysis to identify disrupted biological processes.
Data Integration:
- Compare expression profiles to known disease signatures.
- Corrogate pathway disruptions with clinical disease phenotypes.
Application: In a proof-of-concept study introducing an EHMT1 variant into HEK293T cells, this approach identified changes in cell cycle regulation, neural gene expression, and chromosome-specific expression suppression consistent with Kleefstra syndrome phenotypes [21].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Functional Genomics
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Gene Editing Systems | CRISPR-Cas9, Prime Editing | Precise introduction of genetic variants into cellular models or model organisms. |
| Single-Cell Platforms | 10x Genomics, Tapestri Mission Bio | High-throughput single-cell analysis enabling simultaneous DNA and RNA profiling. |
| Sequencing Reagents | Illumina Nextera, TruSeq | Library preparation for next-generation sequencing of genomic DNA and transcriptomes. |
| Cell Culture Models | HEK293T, iPSCs, Primary cells | Cellular context for evaluating variant effects in relevant biological systems. |
| Fixation Agents | Paraformaldehyde (PFA), Glyoxal | Cell fixation and permeabilization for nucleic acid preservation in single-cell assays. |
| Bioinformatic Tools | GATK, Seurat, DTOM | Data analysis pipelines for variant calling, single-cell analysis, and causal inference. |
Analytical Framework for Functional Evidence
Causal Discovery Using Directed Topological Overlap Matrix (DTOM)
Principle: Moving beyond correlation analysis, DTOM provides a more flexible approach to causal discovery that is robust to measurement errors, averaging effects, and feedback loops [22]. This method relaxes the local causal Markov condition and uses Reichenbach's common cause principle instead, providing significant improvements in sample efficiency.
Application: DTOM has demonstrated utility in distinguishing myostatin mutation status in cattle based on muscle transcriptomes, identifying deleted genes in yeast deletion studies using differentially expressed gene sets, and elucidating causal genes in Alzheimer's disease progression [22].
Four-Step Framework for Functional Evidence Evaluation
The ClinGen SVI Working Group recommends a structured approach for assessing functional assays:
Define Disease Mechanism: Establish the expected molecular consequence of pathogenic variants (e.g., loss-of-function, gain-of-function, dominant-negative).
Evaluate General Assay Classes: Determine which general classes of assays (e.g., splicing, enzymatic, protein localization, transcriptional activation) are appropriate for the disease mechanism.
Validate Specific Assay Instances: Assess the technical validation of specific assay implementations using established control requirements and performance metrics.
Apply to Variant Interpretation: Assign appropriate evidence strength based on assay validation and result concordance with expected functional impact.
This framework ensures functional data meets baseline quality standards before application in clinical variant interpretation [11].
Functional genomics represents the essential bridge between variant detection and clinical application, providing the causal evidence required to move from correlation to causation. The methodologies outlined here—from single-cell multi-omics to CRISPR-based functional phenotyping and advanced causal inference algorithms—provide researchers with standardized approaches for variant interpretation. As these technologies continue to evolve, they will increasingly enable the resolution of variants of unknown significance, ultimately improving diagnostic yields and advancing personalized medicine approaches for rare and common genetic diseases. The future of functional genomics lies in the continued development of scalable, quantitative assays that can be systematically validated and standardized across laboratories, ultimately benefiting patients through more accurate genetic diagnoses.
A Toolkit for Validation: From Bench Assays to Bioinformatics
Cell-based assays are indispensable tools in functional genomics and immunology, enabling researchers to connect genetic findings to phenotypic outcomes. In the context of validating genetic variants in immune dysfunction disorders, assays that probe specific cellular signaling pathways and effector functions are particularly valuable. This application note details two essential methodologies: the Phospho-STAT1 (Tyr701) AlphaLISA assay for interrogating JAK/STAT signaling pathway integrity, and the Dihydrorhodamine (DHR) assay for assessing phagocytic function in Chronic Granulomatous Disease (CGD). These assays provide critical functional data that can help determine the pathogenicity of variants of uncertain significance (VUS) in immunologically relevant genes, bridging the gap between genomic sequencing and clinical manifestation [23].
The integration of such functional assays is becoming increasingly important as genomic studies reveal numerous VUS whose clinical significance remains ambiguous. Without functional validation, these variants pose challenges for genetic counseling and personalized treatment strategies [23]. The pSTAT1 and DHR assays described herein offer robust, quantitative approaches to characterize immune dysfunction at the cellular level, providing insights into disease mechanisms and potential therapeutic avenues.
Phospho-STAT1 (Tyr701) Assay for JAK/STAT Signaling Assessment
Background and Principle
Signal Transducer and Activator of Transcription 1 (STAT1) is a crucial transcription factor in the JAK/STAT signaling pathway, playing a central role in mediating interferon responses, immune regulation, and cell growth control [24]. Activation of STAT1 occurs through phosphorylation at tyrosine residue 701 (Tyr701), which is essential for STAT1 dimerization, nuclear translocation, and subsequent transcriptional activity [24]. Dysregulation of STAT1 signaling is implicated in various pathological conditions, including recent findings that the EGFR-STAT1 pathway drives fibrosis initiation in fibroinflammatory skin diseases [25]. This pathway represents a novel interferon-independent function of STAT1 in mediating fibrotic skin conditions [25].
The AlphaLISA SureFire Ultra Phospho-STAT1 (Tyr701) assay is a sandwich immunoassay that enables quantitative detection of phosphorylated STAT1 in cellular lysates using Alpha technology [24]. This homogeneous, no-wash assay is particularly suitable for research investigating immune signaling dysregulation potentially stemming from genetic variants in STAT1 or related pathway components.
Detailed Protocol
Cell Culture and Treatment
- Cell Preparation: Plate appropriate cells (e.g., THP-1 cells, primary macrophages, or patient-derived cells) in complete medium. For THP-1 cells, seed at 100,000 cells/well in a 96-well plate containing 100 nM PMA and incubate for 24 hours at 37°C, 5% CO₂ to differentiate into macrophages [24].
- Serum Starvation: Replace medium with starvation medium (e.g., HBSS + 0.1% BSA) for 2 hours to minimize basal signaling activity.
- Stimulation: Treat cells with IFNγ (typically 0.1-100 ng/mL) or other relevant stimuli for 15-20 minutes to induce STAT1 phosphorylation. Include appropriate controls (unstimulated and maximum stimulation).
Cell Lysis
- Immediately after stimulation, remove treatment medium and lyse cells with recommended Lysis Buffer (e.g., 60-150 μL depending on cell density) for 10 minutes at room temperature with shaking at 350 rpm [24].
- Note: The lysates can be used immediately or stored at -80°C for future analysis.
Detection Procedure
- Transfer 10 μL of cell lysate to a 384-well white OptiPlate.
- Add 5 μL of Acceptor Mix and incubate for 1 hour at room temperature.
- Add 5 μL of Donor Mix and incubate for 1 hour at room temperature in the dark.
- Read the plate using an EnVision or compatible plate reader with standard AlphaLISA settings.
Assay Validation Data
The Phospho-STAT1 assay demonstrates robust performance characteristics as validated in multiple cell models:
Table 1: Validation data for Phospho-STAT1 (Tyr701) AlphaLISA assay
| Cell Type | Stimulus | EC₅₀ | Dynamic Range | Key Findings |
|---|---|---|---|---|
| Primary human macrophages | IFNα | ~1-10 ng/mL | >100-fold | Dose-dependent phosphorylation; specific for pSTAT1 without affecting total STAT1 [24] |
| Primary human macrophages | IFNγ | ~0.1-10 ng/mL | >100-fold | Strong phosphorylation response; pathway specificity confirmed [24] |
| THP-1-derived macrophages | IFNγ | ~0.1-10 ng/mL | >50-fold | Reproducible dose response; minimal inter-assay variability [24] |
| RAW 264.7 mouse macrophages | Mouse IFNγ | ~0.1-10 ng/mL | >50-fold | Cross-species reactivity confirmed; similar performance in mouse cells [24] |
Research Applications in Functional Genomics
The pSTAT1 assay provides critical functional data for evaluating variants in STAT1 and related pathway genes. Recent research has highlighted the importance of STAT1 in fibroinflammatory skin diseases, where single-cell RNA sequencing analysis revealed that STAT1 is the most significantly upregulated transcription factor in SFRP2+ profibrotic fibroblasts across multiple fibroinflammatory conditions [25]. This assay can help determine whether genetic variants affect STAT1 phosphorylation kinetics, magnitude, or duration, thereby establishing potential pathogenicity.
Furthermore, the discovery that EGFR can directly activate STAT1 in a JAK-independent manner in fibrotic skin diseases [25] opens new avenues for investigating crosstalk between signaling pathways that may be disrupted by genetic variants. This assay can be adapted to test activation by alternative stimuli beyond interferons, including EGF family ligands.
DHR Assay for Chronic Granulomatous Disease (CGD) Diagnosis
Background and Principle
Chronic Granulomatous Disease (CGD) is an inherited phagocytic disorder characterized by recurrent, life-threatening pyogenic infections and granulomatous inflammation. The disease arises from defects in the phagocytic nicotinamide dinucleotide phosphate (NADPH) oxidase complex, resulting in reduced or absent production of microbicidal reactive oxygen species (ROS) during phagocytosis [26]. The DHR assay indirectly measures ROS production by monitoring the oxidation of dihydrorhodamine 123 to its fluorescent form, rhodamine, providing a robust flow cytometry-based screening method for CGD [26].
The NADPH oxidase complex consists of five subunit proteins: two membrane components (gp91phox, p22phox) and three cytosolic components (p47phox, p67phox, p40phox). Genetic defects in any of these components can cause CGD, with approximately 60% of cases resulting from X-linked mutations in the CYBB gene encoding gp91phox, and 30% from autosomal recessive mutations in the NCF1 gene encoding p47phox [26]. The DHR assay can detect CGD patients, carriers, and can suggest the underlying genotype based on the pattern of oxidative activity.
Detailed Protocol
Reagent Preparation
- DHR123 Stock Solution: Prepare at 2500 μg/mL in DMSO. Aliquot into 35 μL volumes and store at -20°C.
- PMA Stock Solution: Prepare at 100 μg/mL in DMSO. Aliquot into 30 μL volumes and store at -20°C.
- Working Solutions: On the day of assay, prepare DHR123 working solution at 15 μg/mL and PMA working solution at 300 ng/mL in phosphate-buffered saline with azide (PBA).
Sample Preparation and Staining
- Collect fresh heparinized blood and dilute 1:10 with PBA.
- Set up three tubes for each patient and control:
- Unstained Control: 100 μL diluted blood
- DHR-Loaded Control: 100 μL diluted blood + 25 μL DHR123 working solution
- Stimulated Test: 100 μL diluted blood + 25 μL DHR123 working solution + 100 μL PMA working solution
- Incubate all tubes in a 37°C water bath for 15 minutes to load DHR123.
- Add PMA to tube 3 only and incubate all tubes for an additional 15 minutes at 37°C.
Sample Processing and Analysis
- Wash samples with PBS and centrifuge.
- Lyse red blood cells using ammonium chloride solution (e.g., Pharm Lyse) for 10 minutes in the dark.
- Wash, centrifuge, and fix cells in 1% formalin.
- Analyze by flow cytometry using the 488nm laser and FITC filter set.
- Gate on neutrophil population based on FSC vs SSC characteristics.
- Calculate Neutrophil Oxidative Index (NOI) as the ratio of mean peak channel fluorescence (MPC-FL) of PMA-stimulated samples to unstimulated samples.
Assay Performance and Interpretation
The DHR assay demonstrates distinct fluorescence patterns that correlate with CGD subtype and severity:
Table 2: DHR assay interpretation guide for CGD diagnosis
| Pattern | NOI Range | Histogram Profile | Possible Genotype | Carrier Detection |
|---|---|---|---|---|
| Normal | >100 (typically 1000+) | Sharp, unimodal peak | Normal | Not applicable |
| X-linked CGD (severe) | 1-2 | Completely flat | CYBB null mutation | Bimodal distribution (mosaic pattern) |
| X-linked CGD (moderate) | 3-50 | Broad, low peak | CYBB hypomorphic mutation | Partial bimodal distribution |
| p47phox-deficient CGD | 3-50 | Broad, low peak | NCF1 mutation | Not typically detectable (autosomal recessive) |
| Other AR CGD (p22phox, p67phox) | 1-50 | Variable | CYBA, NCF2 mutations | Not typically detectable (autosomal recessive) |
Recent advancements include the development of a DHR-ELISA method that offers a rapid, cost-effective alternative for CGD screening, particularly in resource-limited settings. This method demonstrated 90% specificity and 90.5-100% sensitivity in detecting CGD compared to genetic testing [27].
Research Applications in Functional Genomics
The DHR assay serves as a crucial functional validation tool for variants in NADPH oxidase complex genes. With the expanding use of next-generation sequencing, numerous VUS are being identified in CGD-associated genes. The DHR assay provides a direct measurement of the functional consequences of these variants on phagocyte function.
In a recent study of 72 children suspected of having CGD, genetic testing revealed mutations in CYBB (71.0%), NCF1 (15.8%), CYBA (7.9%), and NCF2 (5.3%) genes [27]. The DHR assay confirmed the functional impact of these mutations, with patients showing significantly reduced enzymatic activity compared to healthy controls. This integration of genetic and functional analysis provides a comprehensive diagnostic approach and helps establish pathogenicity for novel variants.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key reagents and resources for pSTAT1 and DHR assays
| Category | Specific Product | Application | Key Features |
|---|---|---|---|
| pSTAT1 Detection | AlphaLISA SureFire Ultra Phospho-STAT1 (Tyr701) Detection Kit [24] | Quantifying STAT1 phosphorylation | Homogeneous, no-wash assay; 10 μL sample volume; compatible with cell lysates |
| Cell Stimulation | Recombinant Human IFNγ | STAT1 pathway activation | High-purity; dose-dependent response (0.1-100 ng/mL) |
| DHR Assay | Dihydrorhodamine 123 (DHR123) [26] | Measuring oxidative burst in phagocytes | Oxidation to fluorescent rhodamine; 375 ng/mL final concentration |
| DHR Stimulation | Phorbol 12-myristate 13-acetate (PMA) [26] | Activating NADPH oxidase complex | Potent PKC activator; 30 ng/mL final concentration |
| DHR Alternative | DHR-ELISA method [27] | CGD screening without flow cytometry | 90% specificity, 90.5-100% sensitivity; cost-effective |
| Advanced Genomics | Single-cell DNA-RNA sequencing (SDR-seq) [6] | Linking genotypes to cellular phenotypes | Simultaneous profiling of 480 genomic DNA loci and genes in single cells |
Experimental Workflows
pSTAT1 Assay Workflow
DHR Assay Workflow
STAT1 Signaling Pathway
The pSTAT1 and DHR assays represent powerful approaches for functionally validating genetic variants associated with immune dysfunction. The pSTAT1 assay provides insights into signaling pathway integrity, with recent research revealing its importance in both canonical interferon signaling and novel pathways such as EGFR-mediated fibrosis [25]. Meanwhile, the DHR assay offers a direct measurement of phagocyte function, essential for diagnosing CGD and validating variants in NADPH oxidase complex genes [26].
These assays bridge the critical gap between genetic identification and functional consequence, enabling researchers to establish pathogenicity for VUS in immunologically relevant genes. As functional genomics advances, integration of such cell-based assays with emerging technologies like single-cell multi-omics [6] will enhance our ability to dissect the mechanistic consequences of genetic variation in immune disorders, ultimately advancing both diagnostic capabilities and therapeutic development.
CRISPR-Cas9 technology has revolutionized functional genomics by enabling precise genetic modifications in a wide range of cell types and organisms. For researchers investigating the functional validation of genetic variants, CRISPR-mediated knock-in and knock-out studies provide powerful tools to establish causal relationships between genetic alterations and phenotypic outcomes. These techniques are particularly valuable in disease modeling, drug target validation, and elucidating mechanisms underlying pathological conditions [28] [29].
The fundamental principle involves using a guide RNA (gRNA) to direct the Cas9 nuclease to specific genomic locations, creating double-strand breaks (DSBs) that are subsequently repaired by cellular mechanisms. While non-homologous end joining (NHEJ) typically results in gene knock-outs through insertions or deletions (indels), homology-directed repair (HDR) enables precise knock-ins using donor DNA templates [28] [29]. Understanding and controlling these repair pathways is essential for successful functional studies of genetic variants.
Fundamental Principles of CRISPR Knock-in/Knock-out
Molecular Mechanisms of DNA Repair Pathways
The cellular response to CRISPR-induced DSBs determines the editing outcome. Non-homologous end joining (NHEJ) is an error-prone repair pathway active throughout the cell cycle, resulting in small insertions or deletions (indels) that often disrupt gene function—making it ideal for knock-out studies [28] [29]. In contrast, homology-directed repair (HDR) uses a donor DNA template for precise repair and is restricted primarily to the S and G2 phases of the cell cycle, enabling precise knock-in modifications [28].
Recent research reveals that DNA repair pathways differ significantly between cell types. Dividing cells such as iPSCs utilize both NHEJ and microhomology-mediated end joining (MMEJ), producing a broad range of indel outcomes. Conversely, postmitotic cells like neurons and cardiomyocytes predominantly employ classical NHEJ, resulting primarily in smaller indels, and exhibit prolonged DSB resolution timelines extending up to two weeks [30].
Advanced CRISPR Systems
Beyond standard CRISPR-Cas9, several advanced systems have expanded gene-editing capabilities:
- Base editing enables direct chemical conversion of one DNA base to another without inducing DSBs, using fusion proteins comprising a catalytically impaired Cas9 and a deaminase enzyme. Cytidine base editors (CBEs) convert C•G to T•A base pairs, while adenine base editors (ABEs) convert A•T to G•C base pairs [29].
- Prime editing offers greater versatility by using a Cas9 nickase-reverse transcriptase fusion and a prime editing guide RNA (pegRNA) to directly write new genetic information into a target DNA site without DSB formation [29].
- Artificial intelligence-designed editors represent the cutting edge, with models like OpenCRISPR-1 showing comparable or improved activity and specificity relative to SpCas9 while being highly divergent in sequence [31].
Experimental Design and Optimization
gRNA Design and Validation
Effective gRNA design is critical for successful knock-in/knock-out experiments. sgRNAs consist of a ~20 nucleotide spacer sequence defining the target site and a scaffold sequence for Cas9 binding. The target site must be immediately adjacent to a protospacer adjacent motif (PAM); for the most commonly used SpCas9, this is 5'-NGG-3' [28].
Comparative analyses of gRNA design tools indicate that Benchling provides the most accurate predictions of editing efficiency [32]. However, computational predictions require experimental validation, as some sgRNAs with high predicted scores may be ineffective—for instance, an sgRNA targeting exon 2 of ACE2 exhibited 80% INDELs but retained ACE2 protein expression [32].
Validation methods include:
- T7 endonuclease I (T7EI) assay detects mismatches in heteroduplex DNA formed by annealing wild-type and edited sequences [33]
- Tracking of Indels by Decomposition (TIDE) analyzes Sanger sequencing chromatograms to quantify editing efficiencies [32]
- Inference of CRISPR Edits (ICE) provides similar functionality with demonstrated accuracy against clonal sequencing data [32]
- Cleavage assay (CA) exploits the inability of Cas9-gRNA complexes to recognize and cleave successfully edited target sites [33]
Enhancing Knock-in Efficiency
HDR-mediated knock-in efficiency is typically lower than NHEJ-mediated knock-out due to cell cycle dependence and pathway competition. The following table summarizes key optimization parameters for both knock-in and knock-out studies:
Table 1: Optimization Parameters for CRISPR-mediated Knock-in and Knock-out Studies
| Parameter | Knock-out Optimization | Knock-in Optimization |
|---|---|---|
| DNA Repair | Favor NHEJ | Suppress NHEJ, enhance HDR |
| Template Design | Not applicable | ssODN: 30-60nt arms; plasmid: 200-500nt arms |
| Cell Cycle | Effective in all phases | Maximize S/G2 populations |
| Delivery Method | RNP electroporation [32] | RNP + HDR template co-delivery |
| Validation | INDEL efficiency ≥80% [32] | HDR efficiency + protein validation |
Strategies to enhance HDR efficiency include:
- HDR template design: For short insertions using single-stranded oligodeoxynucleotides (ssODNs), 30-60 nucleotide homology arms are recommended. For larger insertions requiring plasmid templates, 200-500 nucleotide homology arms yield optimal results [28].
- Cell cycle synchronization: Enriching for S/G2 phase populations increases HDR efficiency [28].
- Strategic insertion placement: Incorporating edits within 5-10 base pairs of the cut site minimizes strand preference effects. For edits outside this window, the targeting strand is preferred for PAM-proximal edits, while the non-targeting strand benefits PAM-distal edits [28].
- Modulating DNA repair: Small molecule inhibitors targeting NHEJ components can enhance HDR efficiency in some cell types [30].
Applications in Disease Research
Cancer Biology and Immunotherapy
CRISPR knock-out screens have identified essential genes in various cancers. For example, a genome-wide screen in metastatic uveal melanoma identified SETDB1 as essential for cancer cell survival, with its knockout inducing DNA damage, senescence, and proliferation arrest [34]. In diffuse large B-cell lymphoma (DLBCL), CRISPR knock-in approaches model specific mutations found in ABC and GCB subtypes to study their impacts on B-cell receptor signaling and NF-κB pathway activation [28].
In cancer immunotherapy, CRISPR-engineered CAR-T cells with knocked-out PTPN2 show enhanced signaling, expansion, and cytotoxicity against solid tumors in mouse models. PTPN2 deficiency promotes generation of long-lived stem cell memory CAR T cells with improved persistence [34].
Genetic Disorders
CRISPR editing shows remarkable therapeutic potential for genetic diseases. Prime editing has achieved 60% efficiency in correcting pathogenic COL17A1 variants causing junctional epidermolysis bullosa, with corrected cells demonstrating a selective advantage in xenograft models [34]. For sickle cell disease, base editing of hematopoietic stem cells outperformed conventional CRISPR-Cas9 in reducing red cell sickling, with higher editing efficiency and fewer genotoxicity concerns [34].
Functional Studies in B Cells
CRISPR knock-out screens enable systematic identification of genes regulating B-cell receptor (BCR) mediated antigen uptake. Using Ramos B-cells and genome-wide sgRNA libraries, researchers can identify genes whose disruption affects BCR internalization through flow cytometry-based sorting and sequencing of sgRNA abundances [35].
Table 2: Applications of CRISPR Knock-in/Knock-out in Disease Modeling
| Disease Area | Genetic Modification | Functional Outcome |
|---|---|---|
| Uveal Melanoma | SETDB1 knockout [34] | DNA damage, senescence, halted proliferation |
| DLBCL | Oncogenic mutation knock-in [28] | Altered BCR signaling and NF-κB activation |
| Sickle Cell Disease | Base editing in HSPCs [34] | Reduced red cell sickling |
| Junctional Epidermolysis Bullosa | COL17A1 prime editing [34] | Restored type XVII collagen expression |
| Solid Tumors | PTPN2 knockout in CAR-T cells [34] | Enhanced tumor infiltration and killing |
Protocols for Knock-in/Knock-out Studies
Protocol: Knock-out in Human Pluripotent Stem Cells (hPSCs) Using Inducible Cas9
This optimized protocol achieves 82-93% INDEL efficiency in hPSCs [32]:
Materials:
- hPSCs with doxycycline-inducible Cas9 (hPSCs-iCas9)
- Chemically modified sgRNA (2'-O-methyl-3'-thiophosphonoacetate modifications)
- Nucleofection system (Lonza 4D-Nucleofector with P3 Primary Cell kit)
- Doxycycline
- Cell culture reagents
Procedure:
- Culture Preparation: Maintain hPSCs-iCas9 in Pluripotency Growth Medium on Matrigel-coated plates.
- Doxycycline Induction: Treat with doxycycline (concentration optimized for your cell line) for 24 hours to induce Cas9 expression.
- Cell Preparation: Dissociate cells with 0.5 mM EDTA and pellet by centrifugation at 250g for 5 minutes.
- Nucleofection: Combine 5μg sgRNA with nucleofection buffer and electroporate using program CA137.
- Repeat Transfection: After 3 days, repeat nucleofection with fresh sgRNA.
- Analysis: Harvest cells 5-7 days post-transfection for INDEL efficiency analysis by TIDE/ICE.
Troubleshooting:
- Low efficiency: Optimize cell-to-sgRNA ratio (8×10⁵ cells: 5μg sgRNA recommended)
- Poor viability: Ensure nucleofection program is appropriate for your hPSC line
- Incomplete knock-out: Verify sgRNA activity and consider dual sgRNAs
Protocol: Knock-in in Primary B Cells
This protocol addresses challenges of low HDR efficiency in primary human B cells [28]:
Materials:
- Primary human B cells or lymphoma cell lines
- Cas9 protein and synthetic sgRNA
- HDR template (ssODN for point mutations, plasmid for large insertions)
- Electroporation system
- Culture media optimized for B cells
Procedure:
- gRNA Complex Formation: Precomplex Cas9 protein with sgRNA at 37°C for 10 minutes to form RNP.
- HDR Template Preparation: For point mutations, design ssODN with 30-60nt homology arms and symmetric extension around the mutation site.
- Cell Preparation: Enrich for cycling cells by pre-stimulation with CD40L and IL-4 for 48 hours to enhance HDR.
- Electroporation: Co-deliver RNP complex and HDR template using optimized electroporation conditions.
- Recovery and Analysis: Culture cells and assess knock-in efficiency after 72-96 hours by flow cytometry, sequencing, or functional assays.
Optimization Tips:
- Test multiple sgRNAs with varying distances to the target mutation
- Consider chemical inhibition of NHEJ to enhance HDR (e.g., KU-0060648)
- For large insertions (e.g., fluorescent proteins), use plasmid donors with 500nt homology arms
Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR Knock-in/Knock-out Studies
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| CRISPR Nucleases | SpCas9, OpenCRISPR-1 [31] | DSB induction at target sites |
| Base Editors | ABE8e, evoAPOBEC1-BE4max | Single nucleotide conversion without DSBs |
| Delivery Systems | LNPs [36], VLPs [30], Electroporation | Efficient cargo delivery to target cells |
| HDR Templates | ssODNs, dsDNA donors | Template for precise knock-in edits |
| gRNA Modifications | 2'-O-methyl-3'-thiophosphonoacetate [32] | Enhanced stability and editing efficiency |
| Validation Tools | ICE, TIDE, Cleavage Assay [33] | Quantification of editing outcomes |
| Cell Lines | hPSCs-iCas9 [32], Ramos B-cells [35] | Optimized platforms for editing studies |
Current Challenges and Future Perspectives
Despite significant advances, CRISPR knock-in/knock-out technologies face several challenges. Delivery efficiency remains a primary bottleneck, particularly for in vivo applications. Lipid nanoparticles (LNPs) show promise for liver-directed therapies but require optimization for other tissues [36]. Off-target effects continue to raise safety concerns, though AI-powered prediction tools are improving specificity assessments [31].
The DNA repair landscape in different cell types presents another hurdle, particularly for HDR-based approaches in non-dividing cells. Recent research reveals that neurons resolve Cas9-induced DSBs over weeks rather than days, with different repair pathway preferences compared to dividing cells [30]. Understanding these cell-type-specific differences is crucial for designing effective editing strategies.
Future directions include:
- AI-designed editors with enhanced properties [31]
- Epigenome editing for reversible gene regulation [34]
- Compact editing systems (e.g., Cas12f variants) compatible with viral delivery [34]
- In vivo delivery optimization through engineered LNPs and viral vectors
As the field advances, CRISPR knock-in/knock-out methodologies will continue to enhance our ability to functionally validate genetic variants, accelerating both basic research and therapeutic development.
The following diagrams provide visual summaries of key concepts and experimental workflows described in this application note.
Diagram 1: CRISPR-Cas9 Mechanism and DNA Repair Pathways
Diagram 2: Experimental Workflow for Functional Validation
In the field of functional validation of genetic variants, one of the primary challenges is interpreting variants of unknown significance (VUS) discovered through next-generation sequencing. A conclusive diagnosis is crucial for patients, clinicians, and genetic counselors, requiring definitive evidence for pathogenicity [20]. Multi-omics corroboration represents a powerful approach to this challenge, integrating diverse biological data layers to validate molecular findings.
RNA sequencing (RNA-seq) coupled with protein-level biomarker profiling provides particularly compelling evidence for functional validation. This approach is revolutionizing molecular diagnostics by offering standardized quantitative assessment across multiple biomarkers in a single assay, overcoming limitations of traditional methods like immunohistochemistry (IHC) which can suffer from subjective interpretation and technical variability [37]. As we transition toward precision medicine, the integration of multi-omics data creates a comprehensive understanding of human health and disease by piecing together the "puzzle" of information across biological layers [38].
Experimental Rationale and Clinical Context
The Challenge of Variants of Unknown Significance
The introduction of whole exome sequencing (WES) and whole genome sequencing (WGS) has revolutionized molecular genetics diagnostics, yet in the majority of investigations, these approaches do not result in a genetic diagnosis [20]. When variants are identified, they often fall into the uncertain significance category, requiring functional validation to determine their pathological impact.
The American College of Medical Genetics and Genomics (ACMG) has established five criteria regarded as strong indicators of pathogenicity, one of which is "established functional studies show a deleterious effect" [20]. Multi-omics approaches directly address this criterion by providing experimental evidence across multiple biological layers.
Advantages of Multi-Omics Corroboration
RNA-seq offers significant advantages for biomarker assessment compared to traditional methods:
- Objective quantification that circumvents inter-observer variability
- Multiplexing capability to evaluate numerous biomarkers simultaneously
- Standardized analysis across different laboratories and sample types
- High-throughput processing suitable for large-scale studies [37]
For clinical diagnostics, RNA-seq can serve as a robust complementary tool to IHC, offering particularly valuable insights when tumor microenvironment factors or sample quality issues affect protein-based assessments [37].
Experimental Protocols
RNA Sequencing for Biomarker Detection
Sample Preparation and Quality Control
- Sample Types: Formalin-fixed, paraffin-embedded (FFPE) tissue blocks or fresh-frozen (FF) tissue specimens
- Tissue Requirements: Minimum neoplastic cellularity of 20% as confirmed by pathologist review of H&E slides
- RNA Extraction: Use RNeasy mini kit (Qiagen) for FFPE samples or AllPrep DNA/RNA Mini Kit for fresh-frozen tissues
- Quality Assessment: Verify RNA integrity number (RIN) >7.0 for optimal sequencing results [37]
Library Preparation and Sequencing
- Library Kits: Utilize SureSelect XT HS2 RNA kit (Agilent Technologies) with SureSelect Human All Exon V7 + UTR exome probe set for FFPE samples; TruSeq Stranded mRNA Library Prep for fresh-frozen tissues
- Sequencing Parameters: Sequence on NovaSeq 6000 (Illumina) as paired-end reads (2 × 150 bp) with targeted coverage of 50 million reads per sample
- Processing: Align reads using Kallisto (version 0.42.4) with index file consistent with TCGA expression data [37]
Immunohistochemistry Validation
Staining and Scoring Protocol
- Automated Staining: Perform IHC using fully automated research stainer (Leica BOND RX) with specific primary antibodies according to manufacturing guidelines
- Controls: Include positive and negative controls in each run
- Digital Imaging: Scan all stained slides and matching H&E sections with Vectra Polaris scanner at 20× magnification
- Quantitative Analysis: Utilize QuPath (version 0.3.2) with positive cell detection algorithm for nuclear immunostains; set parameters to default for DAB chromogen with adjustments for cell size and optical density thresholds calibrated on control slides
- Pathologist Review: Have two pathologists review each digital slide independently, with consensus review for discordant cases [37]
Functional Validation of Genetic Variants
CRISPR-Based Functional Assays
- Cell Line Selection: Use HEK293T cells for variant introduction
- Gene Editing: Employ CRISPR/Cas9 system to introduce specific variants
- Transcriptomic Profiling: Conduct genome-wide RNA sequencing post-editing to identify pathway alterations
- Phenotypic Correlation: Compare transcriptional changes to known disease mechanisms and clinical phenotypes [21]
Quantitative Data Correlations
RNA-seq and IHC Correlation Values
Table 1: Correlation between RNA-seq and IHC across key cancer biomarkers
| Biomarker | Biological Role | Spearman's Correlation (r) | Clinical Utility |
|---|---|---|---|
| ESR1 (ER) | Estrogen receptor | 0.89 | Breast cancer treatment selection |
| PGR (PR) | Progesterone receptor | 0.85 | Breast cancer prognosis |
| ERBB2 (HER2) | Receptor tyrosine kinase | 0.79 | Targeted therapy eligibility |
| AR | Androgen receptor | 0.81 | Prostate cancer treatment |
| MKI67 (Ki-67) | Proliferation marker | 0.73 | Tumor aggressiveness |
| CD274 (PD-L1) | Immune checkpoint | 0.63 | Immunotherapy response |
| CDX2 | Transcription factor | 0.76 | Tumor origin identification |
| KRT7 | Cytokeratin 7 | 0.69 | Differential diagnosis |
| KRT20 | Cytokeratin 20 | 0.71 | Differential diagnosis |
Data derived from analysis of 365 FFPE samples across multiple solid tumors showing strong correlations between RNA-seq and IHC for most biomarkers [37]. The slightly lower correlation for PD-L1 (0.63) reflects the influence of tumor microenvironment and immune cell infiltration on this marker.
Diagnostic Performance of RNA-seq Thresholds
Table 2: Diagnostic accuracy of RNA-seq thresholds for predicting IHC status
| Biomarker | Cancer Types | RNA-seq Cut-off | Diagnostic Accuracy | Cohort Validation |
|---|---|---|---|---|
| ESR1 | Breast | 12.5 TPM | 97% | Internal + TCGA |
| PGR | Breast | 8.7 TPM | 95% | Internal + TCGA |
| ERBB2 | Breast, Gastric | 15.2 TPM | 94% | Internal + CPTAC |
| AR | Prostate | 10.1 TPM | 93% | Internal + TCGA |
| MKI67 | Pan-cancer | 9.8 TPM | 91% | Internal cohort |
| CD274 | Multiple | 7.5 TPM | 87% | Internal cohort |
RNA-seq thresholds were established to distinguish positive from negative IHC scores with high diagnostic accuracy (up to 98%) across internal and external validation cohorts [37]. TPM = transcripts per million.
Workflow Visualization
Multi-Omics Corroboration Workflow
This integrated workflow demonstrates the systematic process from sample collection to variant interpretation, highlighting key stages where RNA-seq and IHC data are generated, correlated, and analyzed to produce clinically actionable insights.
The Scientist's Toolkit
Essential Research Reagents and Platforms
Table 3: Key research reagents and platforms for multi-omics corroboration
| Category | Specific Product/Platform | Manufacturer/Developer | Primary Function |
|---|---|---|---|
| RNA Extraction | RNeasy Mini Kit | Qiagen | High-quality RNA isolation from FFPE and fresh tissues |
| Library Prep | SureSelect XT HS2 RNA Kit | Agilent Technologies | Target enrichment for RNA sequencing |
| Sequencing | NovaSeq 6000 | Illumina | High-throughput sequencing (2×150 bp) |
| IHC Automation | BOND RX Research Stainer | Leica Biosystems | Automated immunohistochemistry staining |
| Digital Pathology | Vectra Polaris | Akoya Biosciences | High-resolution slide scanning (20×) |
| Image Analysis | QuPath (v0.3.2) | Open Source | Quantitative pathology and cell detection |
| Data Analysis | Kallisto (v0.42.4) | Open Source | RNA-seq quantification and alignment |
| Functional Validation | CRISPR/Cas9 System | Various | Introduction of specific variants in cell models |
These essential tools enable the generation of high-quality multi-omics data for functional validation studies [37] [21]. The integration of automated platforms with open-source analysis tools creates a robust framework for reproducible research.
Multi-Omics Integration and Knowledge Graphs
Advanced Data Integration Strategies
The complexity of multi-omics data necessitates sophisticated integration approaches. Knowledge graphs combined with Graph Retrieval-Augmented Generation (GraphRAG) are emerging as powerful solutions for structuring heterogeneous biological data [38]. In this framework:
- Nodes represent biological entities (genes, proteins, metabolites, diseases, drugs)
- Edges represent relationships between them (protein-protein interactions, gene-disease associations)
- GraphRAG enables AI systems to make sense of large, interconnected datasets by combining retrieval with structured graph representations [38]
This approach significantly improves retrieval precision (by 3x according to some studies) and reduces AI hallucinations by anchoring outputs in verified graph-based knowledge [38].
Integration Methodologies
Table 4: Multi-omics integration strategies for functional validation
| Integration Strategy | Timing | Advantages | Best For |
|---|---|---|---|
| Early Integration | Before analysis | Captures all cross-omics interactions; preserves raw information | Studies with balanced data types and sufficient samples |
| Intermediate Integration | During analysis | Reduces complexity; incorporates biological context through networks | Pathway analysis and network-based discovery |
| Late Integration | After individual analysis | Handles missing data well; computationally efficient | Clinical applications with heterogeneous data quality |
Researchers typically choose between these integration strategies based on their specific analytical goals and data characteristics [39]. Intermediate integration has proven particularly valuable for connecting genes to pathways, clinical trials, and drug targets, which is difficult to achieve with single-omics approaches.
Study Design Considerations
Guidelines for Robust Multi-Omics Studies
Based on comprehensive benchmarking across multiple TCGA datasets, the following design principles ensure robust multi-omics integration:
- Sample Size: Minimum of 26 samples per class for adequate statistical power
- Feature Selection: Select less than 10% of omics features to reduce dimensionality
- Class Balance: Maintain sample balance under 3:1 ratio between groups
- Noise Management: Keep noise level below 30% through careful experimental design [40]
Feature selection has been shown to improve clustering performance by 34% in multi-omics studies, highlighting its critical importance in study design [40].
Multi-omics corroboration using RNA-seq and biomarker profiles provides a powerful framework for functional validation of genetic variants. The strong correlation between RNA expression and protein levels across key biomarkers enables researchers to leverage the quantitative advantages of RNA-seq while maintaining connection to established clinical paradigms based on protein detection.
As multi-omics technologies continue to advance, integration with knowledge graphs and AI-powered analysis platforms will further enhance our ability to interpret variants of unknown significance. This approach moves us closer to comprehensive functional validation, ultimately improving diagnostic certainty and enabling more personalized therapeutic interventions for patients with rare genetic disorders and cancer.
The functional validation of genetic variants represents a critical bottleneck in genomic research and clinical diagnostics. Next-generation sequencing (NGS) has enabled comprehensive variant discovery, yet distinguishing true pathogenic variants from sequencing artifacts and benign polymorphisms remains challenging [41]. Traditional variant refinement pipelines require manual inspection by trained researchers, a process that is time-consuming, introduces inter-reviewer variability, and limits scalability and reproducibility [41] [42].
Machine learning (ML), particularly convolutional neural networks (CNNs), offers a transformative approach to automate variant refinement. These computational tools learn complex patterns from large genomic datasets to improve the accuracy and efficiency of variant classification [41] [43]. Within functional validation research, automated refinement enables researchers to prioritize variants for downstream experimental studies, ensuring that valuable laboratory resources are allocated to the most biologically relevant candidates. This document provides detailed application notes and protocols for implementing these advanced computational tools in a research setting focused on the functional validation of genetic variants.
Background and Significance
The Challenge of Variant Refinement
Variant calling pipelines inherently struggle with sequencing artifacts that arise from multiple sources, including library preparation, cluster amplification, and base-calling errors [41]. When germline and tumor samples undergo separate library preparations, systematic artifacts can manifest as false positive variant calls that appear highly credible upon initial inspection. Manual refinement using tools like the Integrative Genomics Viewer (IGV) requires researchers to assess evidence by considering factors such as sequencing coverage, strand bias, mapping quality, and regional complexity [41]. This manual process, while necessary, introduces subjectivity; different researchers may reach different conclusions despite following identical guidelines, with one study reporting 94.1% concordance among reviewers [41].
Machine Learning as a Solution
Machine learning approaches address these limitations by providing objective, standardized, and scalable frameworks for variant refinement. These methods can be broadly categorized as follows:
- Deep Learning-based Callers: Tools like DeepVariant use CNNs to process sequencing data transformed into image-like representations, learning to identify true variants based on spatial patterns in the data [43].
- Refinement Filters: Supervised models, such as the decision tree-based GVRP (Genome Variant Refinement Pipeline), are trained to filter false positive calls from an initial variant set using features derived from alignment metrics and caller confidence scores [43].
- Integrated Workflows: End-to-end systems that incorporate machine learning directly into the tertiary analysis platform, using ensemble models to predict which variants require expert curation and clinical reporting [42].
The integration of these tools into functional validation research ensures that variants selected for laboratory experiments have passed rigorous, reproducible computational standards, thereby increasing the likelihood of successful experimental outcomes.
Key Computational Tools and Methodologies
Tool Comparison and Selection
Table 1: Comparison of Automated Variant Refinement Tools
| Tool Name | Underlying Methodology | Target Setting | Key Features | Reusable Model |
|---|---|---|---|---|
| deepCNNvalid [41] | Convolutional Neural Network (CNN) | Somatic variants | Incorporates contextual sequencing tracks; robust performance on large datasets | Yes |
| GVRP [43] | Light Gradient Boosting Model (LGBM) | Non-human primates & human | Filters false positives using alignment metrics & DeepVariant scores; handles suboptimal alignment | Yes |
| PathOS [42] | Ensemble (Random Forest, XGBoost) & Neural Networks | Clinical somatic reporting | Integrates 200+ annotations; explains predictions via waterfall plots | Assay-dependent |
| DeepVariant [43] | CNN on pileup images | Germline & somatic | State-of-the-art caller; transforms alignments to images for classification | Yes |
| Ainscough et al. method [41] | Random Forest & Perceptron | Somatic variants | Uses hand-crafted summary statistics; limited transferability | No |
Performance Metrics
Table 2: Reported Performance of ML-Based Refinement Tools
| Tool / Study | Dataset | Key Performance Metrics | Outcome |
|---|---|---|---|
| GVRP [43] | Rhesus macaque genomes with suboptimal alignment | 76.20% reduction in miscalling ratio | Significantly improved variant calling in resource-limited settings |
| PathOS Models [42] | 10,116 patients; 1.35M variants | PRC AUC: 0.904-0.996 | High precision in identifying reportable variants |
| deepCNNvalid [41] | Two large-scale somatic datasets | Performance on par with trained researchers | Automated refinement matching human expert SOPs |
| Tree-based Ensembles [42] | Three somatic clinical assays | >30% performance from assay-specific features | Highlights importance of local sequencing context |
Experimental Protocols
Protocol 1: Implementing the GVRP Refinement Pipeline
This protocol details the steps for implementing the Genome Variant Refinement Pipeline to filter false positive variants from DeepVariant output, particularly under suboptimal alignment conditions [43].
Research Reagent Solutions
Table 3: Essential Materials and Software for GVRP Implementation
| Item | Function/Description | Example Sources/Version |
|---|---|---|
| BWA-MEM | Aligns sequencing reads to a reference genome | Bioinformatics tool [43] |
| SAMtools | Processes alignments; sorts and indexes BAM files | Bioinformatics tool [43] |
| DeepVariant | Generates initial variant calls from BAM files | Google; v1.5.0 [43] |
| GVRP Package | Applies the refinement model to filter false positives | https://github.com/Jeong-Hoon-Choi/GVRP [43] |
| GIAB Reference | Provides benchmark variants for validation | Genome in a Bottle Consortium [44] |
| Python 3.8+ | Programming environment for running the pipeline | Python Software Foundation |
Step-by-Step Procedure
Sequence Alignment (Suboptimal Conditions):
- Align sequencing reads to the reference genome using BWA-MEM.
- Perform basic post-processing including sorting with SAMtools and marking duplicates with Picard.
- Note: For suboptimal alignment conditions, omit indel realignment and base quality score recalibration to simulate scenarios with limited reference resources [43].
Variant Calling:
- Run DeepVariant on the processed BAM file to generate an initial VCF file.
- Example command:
run_deepvariant --model_type=WGS --ref=reference.fa --reads=aligned.bam --output_vcf=initial_calls.vcf
Feature Extraction for Refinement:
- Extract the following features from the BAM and VCF files:
- DeepVariant confidence scores (e.g., likelihoods for each genotype)
- Read depth at the variant site
- Soft clipping ratio (proportion of soft-clipped bases in the region)
- Low mapping quality read ratio (proportion of reads with MAPQ < 20) [43]
- Extract the following features from the BAM and VCF files:
Model Application:
- Execute the GVRP pipeline using the extracted features.
- Example command:
gvrp refine --input_vcf=initial_calls.vcf --bam=aligned.bam --output_vcf=refined_calls.vcf --model=pretrained_lgbm_model.txt
Output Interpretation:
- The pipeline produces a refined VCF file with false positive calls filtered out.
- The refined set is suitable for downstream functional validation studies.
Validation and Quality Control
- Validate the refinement performance using a benchmark set such as Genome in a Bottle (GIAB) reference materials if available for your species [44].
- Compare the number of variants pre- and post-refinement. A successful run typically shows a significant reduction in variant count without removing known true positives.
Protocol 2: Training a Custom CNN for Variant Refinement
This protocol outlines the procedure for developing a custom convolutional neural network for variant refinement, based on the deepCNNvalid methodology [41].
Research Reagent Solutions
Table 4: Essential Materials for Custom CNN Development
| Item | Function/Description | Example Sources |
|---|---|---|
| Python ML Stack | Provides deep learning framework | TensorFlow/PyTorch, Keras |
| Training Variant Sets | Curated datasets of true and false variants | Internal databases; public repositories |
| IGV | Visual validation of training examples | Broad Institute [41] |
| Compute Resources | GPU acceleration for model training | NVIDIA GPUs with CUDA support |
Step-by-Step Procedure
Data Preparation:
- Compile a training set of variants with ground truth labels (true positive/false positive) confirmed through manual review or orthogonal validation.
- For each variant, extract sequencing data from the BAM file and convert to a multi-channel tensor representation, incorporating:
- Reference sequence
- Aligned reads with base quality information
- Mapping quality scores
- Strand orientation information [41]
Model Architecture Design:
- Implement a CNN architecture with the following components:
- Input layer: Accepts the multi-channel tensor
- Convolutional layers: 2-3 layers with increasing filters (32, 64, 128) to capture spatial hierarchies
- Pooling layers: Max pooling to reduce dimensionality
- Fully connected layers: 1-2 layers for final classification
- Output layer: Softmax activation for binary classification (true variant/artifact) [41]
- Implement a CNN architecture with the following components:
Model Training:
- Split data into training (80%), validation (10%), and test sets (10%).
- Train the model using categorical cross-entropy loss and Adam optimizer.
- Implement early stopping based on validation loss to prevent overfitting.
Model Validation:
- Evaluate model performance on the held-out test set using precision, recall, and F1-score.
- Compare model predictions against manual refinement by experts to ensure performance matches human-level accuracy [41].
Implementation Notes
- The model can be integrated into existing variant calling pipelines by processing VCF files and outputting a refined VCF with classification probabilities.
- For functional validation studies, variants can be prioritized based on the model's confidence score before proceeding to experimental work.
Integration with Functional Validation Workflows
Automated variant refinement serves as a critical gatekeeper before resource-intensive laboratory experiments. The following diagram illustrates the position of these computational tools within a comprehensive functional validation research pipeline.
Variant Refinement in Research Workflow
Technical Considerations and Limitations
Data Requirements and Feature Engineering
The performance of ML-based refinement tools is highly dependent on the quality and completeness of training data. Tree-based models like those used in GVRP require careful feature selection, with the most informative features typically including:
- Read depth and quality metrics
- Alternative allele frequency
- Mapping quality statistics
- Regional genomic context [43]
For clinical applications, one study found that over 30% of model performance derived from laboratory-specific features, limiting immediate generalizability to other settings [42]. This underscores the importance of including local sequencing characteristics when training or fine-tuning models.
Interpretability and Explainability
The "black box" nature of deep learning models, particularly CNNs, presents challenges for scientific interpretation. Several approaches can enhance model transparency:
- Gradient-based Feature Attribution: Methods like Saliency Maps highlight which input regions most influenced the model's decision [45].
- Prediction Explanation Interfaces: Tertiary analysis platforms can visualize model predictions through waterfall plots showing individual feature contributions [42].
- Benchmarking Against Known Variants: Regular validation against established benchmark sets maintains model calibration and performance monitoring [44].
Machine learning and convolutional neural networks represent powerful approaches for automating variant refinement in functional validation research. The protocols outlined herein provide researchers with practical guidance for implementing these tools, enabling more efficient and reproducible prioritization of genetic variants for downstream experimental studies. As these computational methods continue to evolve, they will increasingly bridge the gap between high-throughput sequencing and biological validation, accelerating the pace of genomic discovery.
Optimizing Validation Workflows: Overcoming Technical and Analytical Hurdles
Next-generation sequencing (NGS) has revolutionized genomic research and clinical diagnostics, enabling comprehensive analysis of genetic variants. However, the transformative potential of this technology is contingent upon data quality. The presence of sequencing artefacts and issues stemming from low-quality input data present substantial challenges for the accurate detection and interpretation of genetic variants, with direct implications for subsequent functional validation studies [46] [47]. In the context of functional genomics research, where the goal is to conclusively determine the pathological impact of genetic variants, these artefacts can lead to false positives or obscure true causal variants, thereby misdirecting valuable research resources [20]. This application note provides a structured framework for identifying, mitigating, and controlling these data quality issues to ensure the reliability of NGS data for downstream functional assays.
Understanding and Classifying Common NGS Artefacts
NGS artefacts are erroneous data points introduced during various stages of the sequencing workflow, from sample preparation to data analysis. Their systematic classification is the first step toward effective mitigation.
Table 1: Common NGS Artefacts, Their Sources, and Identifying Features [48] [47]
| Artefact Type | Primary Source in Workflow | Key Identifying Features | Impact on Data |
|---|---|---|---|
| Chimeric Reads | Library Preparation (Fragmentation) | Misalignments at read ends; contain inverted repeat or palindromic sequences [47]. | False positive SNVs and Indels. |
| PCR Duplicates | Library Amplification | Identical reads with same start and end coordinates. | Uneven coverage; overestimation of library complexity. |
| Base Call Errors | Sequencing Chemistry | Low-quality scores; context-specific errors (e.g., homopolymer regions in Ion Torrent) [46]. | Incorrect base calling; false SNVs. |
| Oxidation Artefacts | Sample Preparation / FFPE Treatment | C > T or G > A transitions. | False positive SNVs, particularly in low-frequency variants. |
| Alignment Errors | Bioinformatic Analysis | Reads clustered in regions of low complexity or high genomic homology. | False indels or SNVs in problematic genomic regions. |
Mechanisms of Artefact Formation
The formation of chimeric reads, a prevalent artefact, can be explained by the Pairing of Partial Single Strands Derived from a Similar Molecule (PDSM) model. This occurs during library preparation, where fragmented DNA strands can form chimeric molecules via their complementary regions [47].
Diagram 1: PDSM model of chimeric read formation.
Protocols for Mitigating Artefacts and Managing Low-Quality Samples
Experimental Protocol: Robust Hybrid-Capture Library Preparation
This protocol is designed to minimize artefact introduction during the pre-sequencing phase, with critical steps for handling challenging samples [48] [49].
1. Sample Assessment and Nucleic Acid Extraction
- Input Material: Quantify DNA using fluorescence-based methods (e.g., Qubit) over UV spectrometry for accuracy. Assess quality via genomic integrity number (GIN) or DV200 for FFPE samples.
- Critical Parameter: For formalin-fixed paraffin-embedded (FFPE) samples, employ uracil-DNA glycosylase (UDG) treatment to reduce cytosine deamination artefacts (C>T transitions) [48].
- DNA Shearing: Use a consistent fragmentation method. If using enzymatic fragmentation, be aware it may generate more artefactual indels in palindromic sequences compared to sonication [47]. Standardize fragmentation time and input DNA mass to achieve desired fragment size (e.g., 200-300bp).
2. Library Preparation with Adapter Ligation
- End Repair & A-tailing: Ensure efficient A-tailing of DNA fragments to prevent chimera formation and facilitate adapter ligation [49].
- Adapter Ligation: Use uniquely dual-indexed adapters to enable precise sample multiplexing and accurate demultiplexing, reducing index hopping cross-talk.
- Library Amplification: Use a high-fidelity DNA polymerase and determine the minimal number of PCR cycles required to obtain sufficient library yield. Excessive cycles increase PCR duplicates and bias.
3. Target Enrichment and Quality Control
- Hybridization Capture: Follow manufacturer's instructions for hybridization time and temperature. Perform post-capture amplification with minimal cycles.
- Final QC: Quantify the final library via qPCR for accurate molarity and analyze on a bioanalyzer or tape station to confirm a clean peak at the expected size. A low library complexity may indicate issues with the input sample.
Bioinformatic Protocol: Artefact Filtering and Quality Control
A robust bioinformatic pipeline is essential for flagging and removing technical artefacts [47] [50].
1. Primary QC and Preprocessing
- Tool: FastQC for initial quality assessment of raw FASTQ files.
- Action: Trimmomatic or Cutadapt to remove adapter sequences and low-quality bases (e.g., quality threshold < Q20).
2. Alignment and Post-Alignment Processing
- Tool: Map reads to a reference genome (e.g., GRCh38) using optimized aligners like BWA-MEM or STAR.
- Action: Mark or remove PCR duplicates using tools like Picard MarkDuplicates or SAMTools to prevent overestimation of coverage [49].
3. Variant Calling and Advanced Artefact Filtering
- Tool: Use multiple callers (e.g., GATK, VarScan) and take the intersection for high-confidence calls.
- Action: Implement a custom "blacklist" filter for recurrent artefact sites. Tools like ArtifactsFinder can identify variants stemming from inverted repeat sequences (IVSs) and palindromic sequences (PSs) [47].
- Annotation: Annotate variants with population frequency (gnomAD), in silico prediction scores, and known artefact flags.
Diagram 2: Bioinformatic pipeline for artefact mitigation.
Quality Metrics and Validation for Functional Genomics
Establishing and monitoring key quality metrics is critical for determining the fitness of NGS data for functional validation studies.
Table 2: Key Performance Indicators (KPIs) for NGS Data Quality Assessment [48] [50]
| Metric Category | Specific Metric | Target Value (Guideline) | Rationale |
|---|---|---|---|
| Sequencing Quality | Q-Score (per base) | ≥ 30 (Q30) | Indicates base calling accuracy (99.9%). |
| Coverage | Mean Depth of Coverage | Varies by application (e.g., >100x for somatic) | Ensures sufficient sampling of each base. |
| Mapping Quality | % Aligned Reads | > 95% | Measures efficiency of alignment. |
| Library Complexity | % PCR Duplicates | < 20% (sample-dependent) | High levels indicate low complexity and potential bias. |
| Capture Efficiency | % Reads on Target | > 60% (for hybrid capture) | Measures specificity of enrichment. |
| Variant Calling | Transition/Transversion (Ti/Tv) Ratio | ~2.0-2.1 (for whole exome) | Deviation from expected ratio indicates systematic errors. |
Linking Data Quality to Functional Validation
In functional genomics, the American College of Medical Genetics and Genomics (ACMG) guidelines strongly emphasize that well-validated functional studies provide key evidence for establishing variant pathogenicity [20]. Therefore, investing in high-quality NGS data that minimizes artefacts is paramount. Reliable NGS data ensures that:
- Resources are allocated efficiently: Functional assays (e.g., in vitro enzymatic assays, RNA-seq, or model organism studies) are costly and time-consuming. They should be reserved for variants of high confidence [20] [51].
- Interpretation is accurate: Functional data from a true variant provides conclusive evidence, whereas data from an artefactual variant is not only misleading but can also contaminate public databases.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Quality-Focused NGS
| Item | Function/Description | Example Use Case |
|---|---|---|
| High-Fidelity Polymerase | PCR enzyme with high replication fidelity to reduce amplification errors. | Library amplification during preparation. |
| UDG Enzyme | Removes uracil residues from DNA, mitigating deamination artefacts from FFPE. | Pre-treatment of DNA from archived samples. |
| Dual-Indexed Adapters | Unique molecular barcodes for both ends of a DNA fragment. | Multiplexing samples while minimizing index hopping. |
| Fragmentation Enzyme Mix | Controlled enzymatic shearing of DNA as an alternative to sonication. | Consistent DNA fragmentation with minimal equipment. |
| Nucleic Acid Integrity Assay | Assesses the quality and degradation level of input DNA/RNA (e.g., RIN/DIN). | QC of input material prior to library prep. |
| Bioinformatic Tools (ArtifactsFinder) | Custom algorithm to identify and filter artefactual variants from IVS/PS. | Post-variant calling filtration to generate a high-confidence call set [47]. |
The path from NGS-based variant discovery to conclusive functional validation is fraught with potential technical pitfalls. A rigorous, multi-layered strategy encompassing optimized wet-lab protocols, sophisticated bioinformatic filtering, and continuous quality monitoring is essential to ensure data integrity. By systematically addressing the challenges of NGS artefacts and low-quality input data, researchers can confidently prioritize variants for downstream functional assays, thereby accelerating the pace of discovery in genomic medicine and strengthening the evidence base for variant classification.
In the field of functional validation of genetic variants, researchers are confronted with a complex and often fragmented bioinformatics software ecosystem. The typical analysis pipeline involves multiple specialized tools for variant calling, annotation, and prioritization. However, tool compatibility issues and a lack of standardization frequently create significant bottlenecks, hindering reproducibility and scalability in research and drug development. These challenges slow down the critical path from genetic discovery to therapeutic insight. This document outlines the specific interoperability problems in genetic variant analysis and provides detailed application notes and a standardized protocol to enhance pipeline robustness and data exchange.
The Interoperability Challenge in Genomics
The primary hurdle in constructing efficient variant analysis pipelines is the seamless integration of discrete software tools. Common issues include:
- Incompatible Data Formats: Tools require input and produce output in diverse, often proprietary, formats, necessitating custom parsers and conversion scripts that introduce points of failure.
- Non-Portable Software Architectures: Many tools are designed as web services, creating dependencies on external network availability and raising data privacy concerns, making them unsuitable for secure clinical or proprietary research environments [52].
- Abandoned or Closed-Source Software: A significant number of published tools become unavailable, are abandoned, or have closed-source code, preventing local installation, customization, and long-term pipeline maintenance [52].
The VIBE (Variant Interpretation using Biomedical literature Evidence) tool exemplifies a solution designed with pipeline interoperability as a core principle. It is a stand-alone, open-source command-line executable that operates completely offline, ensuring operational availability and avoiding the legal and ethical barriers of transmitting patient data to external services [52]. Its input and output are specifically designed for easy incorporation into bioinformatic pipelines.
Key Research Reagent Solutions
The following table details essential software and data resources critical for building interoperable functional genomics pipelines.
Table 1: Key Research Reagent Solutions for Genomic Pipeline Interoperability
| Item Name | Function/Application | Key Features for Interoperability |
|---|---|---|
| VIBE (Variant Interpretation using Biomedical literature Evidence) [52] | Prioritizes disease genes based on patient symptoms (HPO codes). | Command-line interface; locally executable JAR file; tab-delimited output; integrates DisGeNET-RDF [52]. |
| SDR-seq (single-cell DNA–RNA sequencing) [6] | Simultaneously profiles genomic DNA loci and gene expression in thousands of single cells. | Links genotype to phenotype in endogenous context; enables functional validation of noncoding variants [6]. |
| DisGeNET-RDF [52] | A comprehensive knowledge platform of gene-disease and variant-disease associations. | Provides a structured, semantically harmonized data source for tools like VIBE; integrates data from curated repositories, GWAS, and literature [52]. |
| FHIR (Fast Healthcare Interoperability Resources) [53] | A standard for exchanging healthcare information electronically. | Enables real-time, secure exchange of clinical and genomic data through APIs; promotes semantic consistency across systems [53]. |
| Apache Jena (TDB) [52] | A framework for building Semantic Web applications. | Used by VIBE to build a local triple store (TDB), enabling efficient, offline SPARQL querying of DisGeNET-RDF data [52]. |
Experimental Protocol: Gene Prioritization with VIBE
This protocol details the steps for integrating the VIBE gene prioritization tool into a variant analysis workflow, using patient phenotypes to rank candidate genes [52].
Equipment and Software Setup
- Computing Environment: A computer with Java 8 or higher installed [52].
- VIBE Software: Download the pre-built executable JAR file from the official GitHub repository (https://github.com/molgenis/vibe) [52].
- VIBE Database: Download the pre-built TDB database or use the provided shell script to build a custom one from source files (DisGeNET, Orphadata HOOM) [52].
Procedure
- Input Preparation: Prepare a list of Human Phenotype Ontology (HPO) codes that describe the patient's clinical symptoms. For example:
HP:0002996,HP:0001250. Command-Line Execution: Run VIBE from the command line. A minimal command includes:
-t: Path to the TDB triple store directory.-o: Path for the output file.-p: One or more HPO codes.
- Advanced Options (Optional):
- Use
-wto supply an HPO OWL file and-mto set a maximum ontology distance traversal to expand the search to related phenotypic terms [52]. - Use
-lfor a genes-only output list.
- Use
- Output Interpretation: The primary output is a tab-delimited file. The key column for prioritization is
highest GDA score, which represents the highest Gene-Disease Association score from the DisGeNET knowledge base for that gene. Genes are listed in descending order of this score [52].
Data Analysis and Integration
- Downstream Filtering: The ranked gene list from VIBE can be cross-referenced with a list of genes harboring variants from a sequencing experiment. Prioritize variants in genes that appear high on VIBE's list.
- Benchmarking Performance: In an evaluation of 305 patient cases, VIBE demonstrated consistent performance, though a high degree of complementarity with other tools was observed. Integrating multiple prioritization tools is recommended for maximum diagnostic yield [52].
Experimental Protocol: Functional Validation with SDR-seq
This protocol describes the use of SDR-seq for the functional phenotyping of genomic variants by jointly measuring DNA and RNA in single cells [6].
Equipment and Reagent Setup
- Single-Cell Suspension: Human induced pluripotent stem (iPS) cells or primary cells (e.g., B cell lymphoma samples) [6].
- Fixatives: Paraformaldehyde (PFA) or Glyoxal. Glyoxal is recommended for superior RNA target detection [6].
- SDR-seq Platform: Tapestri technology (Mission Bio) and microfluidic chips [6].
- Custom Primer Panels: Multiplexed PCR primers for targeted gDNA loci (e.g., 480 loci) and RNA transcripts [6].
Procedure
- Cell Fixation and Reverse Transcription: Dissociate cells into a single-cell suspension, fix with glyoxal, and permeabilize. Perform in situ reverse transcription (RT) using custom poly(dT) primers to generate cDNA with unique molecular identifiers (UMIs) and sample barcodes [6].
- Droplet-Based Partitioning and Lysis: Load the cells onto the Tapestri platform to generate the first droplet. Subsequently, lyse the cells and treat with proteinase K [6].
- Multiplexed Targeted PCR: A second droplet is generated, combining the lysed cells with reverse primers, forward primers with a capture sequence, PCR reagents, and barcoding beads. A multiplexed PCR simultaneously amplifies the targeted gDNA and cDNA molecules within each droplet, attaching a unique cell barcode to all amplicons from the same cell [6].
- Library Preparation and Sequencing: Break the emulsions and separate the gDNA and RNA amplicons based on distinct primer overhangs. Prepare next-generation sequencing libraries for each modality separately and sequence. gDNA libraries are sequenced to full amplicon length for variant calling, while RNA libraries are sequenced to capture gene expression, UMI, and cell barcode information [6].
Data Analysis
- Variant Zygosity Determination: Analyze gDNA sequencing data to confidently call coding and noncoding variants and determine their zygosity (e.g., heterozygous/homozygous) at single-cell resolution. The high coverage of SDR-seq results in low allelic dropout rates, enabling accurate zygosity calls [6].
- Differential Expression Analysis: Analyze RNA sequencing data to quantify gene expression levels using UMI counts. Compare expression profiles between cells carrying a specific variant of interest and wild-type cells [6].
- Genotype-Phenotype Linking: Correlate specific variant genotypes (from gDNA data) with altered transcriptional phenotypes (from RNA data) within the same cell. This allows for the direct functional validation of both coding and noncoding variants in their endogenous genomic context [6].
Workflow Visualization
The following diagrams, generated with Graphviz, illustrate the core protocols and data relationships described in this document.
Diagram 1: VIBE Gene Prioritization Workflow.
Diagram 2: SDR-seq Functional Phenotyping Workflow.
Diagram 3: Integrating Prioritization and Functional Validation.
In the field of functional validation of genetic variants, research workflows are becoming increasingly complex, spanning wet-lab experiments and extensive dry-lab computational analysis. Efficiently managing these processes is critical for accelerating the pace of discovery in genomics and drug development. This document outlines integrated best practices in workflow automation, modular design, and cloud computing, providing application notes and detailed protocols tailored for research scientists and drug development professionals. These methodologies are designed to enhance reproducibility, scalability, and overall efficiency in genomic research.
Core Concepts and Quantitative Benefits
Integrating modern efficiency strategies provides tangible, measurable benefits for research operations. The table below summarizes key advantages and their quantitative impact, which are particularly relevant for data-intensive genomic studies [54] [55] [56].
Table 1: Core Efficiency Concepts and Their Measured Impact
| Concept | Core Principle | Key Benefits in Genomic Research | Quantitative Impact |
|---|---|---|---|
| Workflow Automation [54] [57] | Automating business processes with predefined rules to minimize human intervention. | - Increased throughput of sample processing- Reduced manual errors in data entry and analysis- Standardized execution of protocols | - Increases efficiency and productivity by automating repetitive tasks [54] [57]- Minimizes human error, leading to higher accuracy [54] [57] |
| Modular Design [55] [58] | Breaking down a system into smaller, self-contained, and interchangeable modules. | - Independent development and validation of assay components (e.g., sequencing, analysis)- Enhanced flexibility to update or replace specific analytical pipelines- Simplified troubleshooting | - Cuts AI costs by up to 98% in modular systems [55]- Enables a 20% increase in development efficiency [59] |
| Cloud Computing [56] [60] [61] | Using remote, scalable computing resources on a pay-as-you-go basis. | - On-demand scaling of compute resources for large-scale genomic analyses (e.g., NGS)- Centralized and secure storage for vast genomic datasets- Enhanced collaboration across research institutions | - Reduces cloud spending by eliminating idle resources [56]- Reduces response times by 25% through automated workflows [55] |
Application in Genomic Research: SDR-Seq as a Model
The recent development of single-cell DNA–RNA sequencing (SDR-seq) exemplifies these principles in action. This method enables the functional phenotyping of genomic variants by simultaneously profiling genomic DNA loci and gene expression in thousands of single cells, directly linking genotypes to cellular phenotypes [6].
Experimental Protocol: SDR-Seq for Functional Validation of Variants
Title: Functional Phenotyping of Genetic Variants in Human iPS Cells using SDR-seq.
Objective: To confidently associate specific coding and noncoding genetic variants with changes in gene expression at single-cell resolution.
Materials and Reagents: Table 2: Research Reagent Solutions for SDR-seq
| Item | Function/Description |
|---|---|
| Human induced pluripotent stem (iPS) cells | A model system for studying the functional impact of genetic variants in a human cellular context [6]. |
| Custom Poly(dT) RT Primers | Contains UMI, sample barcode, and capture sequence for in situ reverse transcription and later barcoding [6]. |
| Fixatives (PFA or Glyoxal) | Used to fix and permeabilize cells. Glyoxal is preferred for superior RNA target detection due to lack of nucleic acid cross-linking [6]. |
| Tapestri Platform (Mission Bio) | Microfluidic instrument for generating droplets for single-cell partitioning and barcoding [6]. |
| Proteinase K | Enzyme used in droplets to lyse cells and digest proteins, releasing nucleic acids [6]. |
| Barcoding Beads | Oligonucleotide beads containing unique cell barcodes for labeling all nucleic acids from a single cell [6]. |
| Target-Specific PCR Primers | Multiplexed primer sets for amplifying up to 480 targeted gDNA loci and RNA sequences [6]. |
Methodology:
- Cell Preparation and Fixation: Dissociate iPS cells into a single-cell suspension. Fix and permeabilize cells using glyoxal for optimal RNA and gDNA preservation [6].
- In Situ Reverse Transcription (RT): Perform RT inside the fixed cells using custom primers. This step adds a unique molecular identifier (UMI), a sample barcode, and a capture sequence to cDNA molecules [6].
- Single-Cell Partitioning and Lysis: Load the cells onto the Tapestri microfluidic platform to generate the first droplet. Within the microfluidic system, lyse the cells and treat with Proteinase K to release gDNA and pre-barcoded cDNA [6].
- Droplet Barcoding and Multiplex PCR:
- A second droplet is generated, combining the cell lysate with target-specific PCR primers, PCR reagents, and barcoding beads.
- A multiplexed PCR is performed inside thousands of droplets simultaneously. This amplifies both the targeted gDNA loci and the cDNA (from RNA targets).
- Cell barcoding is achieved as amplicons are tagged with the unique barcode from the bead in each droplet [6].
- Library Preparation and Sequencing:
- Break the emulsions and pool the amplicons.
- Use distinct overhangs on the gDNA and RNA amplicons to separate and prepare two sequencing libraries: one for full-length gDNA (to cover variants) and one for RNA (containing cell BC, sample BC, and UMI information).
- Sequence the libraries using optimized NGS protocols [6].
- Data Analysis:
- Demultiplex reads based on cell barcode and sample barcode.
- Map gDNA reads to reference genomes to call variants and determine zygosity at the single-cell level.
- Collapse RNA reads by UMI to generate accurate gene expression counts per cell.
- Correlate variant genotypes with gene expression phenotypes in the same cell [6].
Diagram 1: SDR-seq experimental workflow for single-cell multiomics.
Implementation Protocols for Efficiency
Protocol for Designing a Modular Research Pipeline
Title: Creating a Modular Bioinformatics Analysis Pipeline.
Objective: To construct a reusable, scalable, and maintainable bioinformatics workflow for genomic data analysis by applying modular design principles.
Methodology:
- Define Clear Module Boundaries: Deconstruct the overall analysis (e.g., variant calling from NGS data) into discrete, purposeful tasks. Assign each task to a specific module with a well-defined input and output "contract" [55]. For example:
- Module 1: Raw FASTQ Quality Control and Trimming.
- Module 2: Alignment to Reference Genome.
- Module 3: Variant Calling and Annotation.
- Module 4: Report Generation.
- Implement Loose Coupling and High Cohesion:
- Design each module to be as independent as possible (loose coupling). For instance, the variant calling module should not depend on the internal workings of the alignment module, only on receiving a correctly formatted BAM file [55].
- Ensure each module has a single, focused responsibility (high cohesion). The quality control module should only handle QC, not perform alignment [55].
- Build for Reusability and Interchangeability: Write modules with standardized input/output formats (e.g., using common genomic file formats like FASTQ, BAM, VCF). This allows the alignment module to be easily swapped from BWA to Bowtie2 without affecting other parts of the pipeline [55] [59].
- Apply Abstraction and Encapsulation: Provide simple, clear interfaces for each module, hiding the complex internal code. This allows fellow researchers to use your variant caller without needing to understand its complex internal algorithms [55].
- Ensure Scalability and Maintainability: Package modules using container technology (e.g., Docker, Singularity) to ensure consistent execution across different computing environments, from a local server to a large cloud cluster [55] [58].
Diagram 2: Modular bioinformatics pipeline with key principles.
Protocol for Cloud-Based Optimization of Genomic Workflows
Title: Implementing a Cost-Efficient Cloud Genomics Analysis.
Objective: To configure and execute a genomic analysis workflow in the cloud that is both performant and cost-effective, leveraging automation and FinOps principles.
Methodology:
- Select Appropriate Instances: Choose cloud computing instances (e.g., AWS EC2, Google Compute Engine) aligned with workload demands. For CPU-intensive tasks like alignment, use compute-optimized instances. For memory-intensive tasks, use memory-optimized instances [56] [60].
- Implement Autoscaling: Use cloud-native tools (e.g., AWS Auto Scaling, Google Cloud Managed Instance Groups) to automatically add or remove compute resources based on real-time demand, such as during peak alignment and variant calling steps [56] [60].
- Optimize Storage with a Tiered Architecture: [60]
- Store active project data on high-performance storage (e.g., SSDs).
- Archive old project data to lower-cost object storage (e.g., Amazon S3 Glacier).
- Implement automated data lifecycle policies to transition data between tiers.
- Track Performance and Cost Metrics: Continuously monitor key metrics using cloud monitoring tools (e.g., CloudWatch, Cloud Monitoring) [56]. Critical metrics include:
- CPU/Memory Utilization
- Storage I/O
- Job Completion Time
- Cloud Cost per Sample Analyzed
- Minimize Data Movement: To reduce costly egress fees, design workflows to keep data processing within the same cloud region. Use cloud caches (e.g., for reference genomes) to speed up data access for multiple concurrent jobs [56] [60].
- Automate Cost Management: Set up automated rules to shut down non-essential resources when not in use (e.g., overnight) and configure budgets and alerts to notify the team of unexpected spending [56] [60].
Integrated Best Practices Checklist
This checklist provides actionable steps for research teams to implement the discussed efficiency strategies.
For Workflow Automation:
- Start Small: Begin by automating one repetitive task, such as automating the generation of standard QC reports after a sequencing run [54] [62].
- Plan for Failures: Design automated workflows with clear paths for handling exceptions, such as a failed sample or a missing file, to ensure robustness [62].
- Involve Key Stakeholders: Include all team members (e.g., wet-lab scientists, bioinformaticians) in the design of automated workflows to ensure the system meets everyone's needs [54] [57].
- Continuously Monitor and Optimize: Regularly review the performance of automated workflows and refine them based on user feedback and performance metrics [54].
For Modular Design:
- Document Module Interfaces: Maintain clear documentation for each module's inputs, outputs, and function to facilitate reuse and collaboration [55] [59].
- Isolate Changes: When updates are needed, modify only the specific module affected, reducing the risk of introducing errors elsewhere in the system [58].
- Use Version Control: Track changes to each module independently using a system like Git, allowing for stable and traceable pipeline evolution [55].
For Cloud Computing:
- Rightsize Resources: Regularly audit cloud resources to ensure you are not over-provisioning compute or storage for your workloads [56] [60].
- Leverage Spot/Preemptible Instances: For fault-tolerant batch jobs like alignment, use lower-cost spot instances to significantly reduce compute costs [56].
- Implement a Cloud Governance Framework: Establish a central team or set of guidelines (a Cloud Center of Excellence) to define and share best practices for cloud usage across the research organization [60].
The Genome in a Bottle (GIAB) Consortium, hosted by the National Institute of Standards and Technology (NIST), develops the technical infrastructure—including reference standards, reference methods, and reference data—to enable the translation of whole human genome sequencing into clinical practice and technological innovation [63]. For researchers conducting functional validation of genetic variants, GIAB provides the foundational benchmarks necessary to ensure accuracy and reproducibility, serving as a critical resource for validating sequencing technologies and bioinformatic pipelines before investigating biological mechanisms. By offering comprehensively characterized human genomes, GIAB allows scientists to measure the performance of their methods against a community-accepted gold standard, ensuring that observed phenotypic effects in functional studies can be traced to genuine genetic variants rather than technical artifacts.
The primary mission of GIAB is the comprehensive characterization of several human genomes for use in benchmarking, including analytical validation and technology development, optimization, and demonstration [63]. This characterization provides the "ground truth" for a growing number of genomic samples. The consortium has currently characterized a pilot genome (NA12878/HG001) from the HapMap project, and two son/father/mother trios of Ashkenazi Jewish (HG002-HG004) and Han Chinese ancestry (HG005-HG007) from the Personal Genome Project [63]. These samples are selected for their well-defined genetic backgrounds and availability for commercial redistribution, making them ideal reference materials for global research efforts.
Reference Samples and Benchmark Variant Calls
GIAB provides several types of reference samples with extensive characterization data available to the research community. The core samples include immortalized cell lines available from NIST and the Coriell Institute, with detailed metadata provided in the table below [63] [64].
Table 1: GIAB Primary Reference Samples
| Sample ID | Relationship | Population | Coriell ID | Primary Applications |
|---|---|---|---|---|
| HG001 | Individual | CEPH/Utah | GM12878 | Pilot genome, method development |
| HG002 | Son | Ashkenazi Jewish | GM24385 | Comprehensive benchmark development |
| HG003 | Father | Ashkenazi Jewish | GM24149 | Trio-based analysis, inheritance validation |
| HG004 | Mother | Ashkenazi Jewish | GM24143 | Trio-based analysis, inheritance validation |
| HG005 | Son | Han Chinese | GM24631 | Population diversity studies |
| HG006 | Father | Han Chinese | GM24694 | Trio-based analysis, inheritance validation |
| HG007 | Mother | Han Chinese | GM24695 | Trio-based analysis, inheritance validation |
For these samples, GIAB provides benchmark variant calls and regions developed through an integration pipeline that utilizes sequencing data generated by multiple technologies [63]. These benchmark files are available in VCF and BED formats for both GRCh37 and GRCh38 reference genomes, encompassing:
- Small variants: Single nucleotide variants (SNVs) and small insertions and deletions (indels) [63]
- Structural variants: Variants ≥50 bp including deletions, duplications, and insertions [65]
- Specialized benchmarks: Tandem repeats, challenging medically relevant genes, and chromosome X/Y variants [66]
The benchmarks undergo continuous refinement, with recent expansions including v4.2.1 for small variants in more difficult regions across all 7 GIAB samples on both GRCh37 and GRCh38, and a v1.0 tandem repeat benchmark for HG002 indels and structural variants ≥5 bp in tandem repeats on GRCh38 [63].
Genomic Stratifications for Context-Specific Performance Analysis
A critical innovation from GIAB is the development of genomic stratifications—BED files that define distinct contexts throughout the genome to enable detailed analysis of variant calling performance in different genomic contexts [67]. These stratifications recognize that no sequencing technology or bioinformatic pipeline performs equally well across all regions of the genome, with particular challenges in repetitive regions, segmental duplications, and areas with extreme GC content.
Table 2: Key GIAB Genomic Stratifications and Their Applications
| Stratification Category | Specific Contexts | Research Utility |
|---|---|---|
| Functional Regions | Coding sequences (CDS), untranslated regions (UTRs), promoters | Focus on medically relevant regions |
| Repetitive Elements | Homopolymers, tandem repeats, segmental duplications | Identify technology-specific error patterns |
| Mapping Complexity | Low-mappability regions, high-identity duplications | Assess performance in ambiguous regions |
| Sequence Composition | High/low GC content, methylated regions | Evaluate sequence-specific biases |
| Technical Artifacts | Alignment gaps, problematic regions | Distinguish biological vs. technical variants |
These stratifications are available for GRCh37, GRCh38, and the newer T2T-CHM13 reference genomes, enabling researchers to understand how their methods perform in specific genomic contexts that are relevant to their research questions [67]. For example, the CHM13 reference includes difficult-to-map regions such as centromeric satellite arrays and rDNA arrays that were absent from previous references, providing a more comprehensive assessment of method performance [67].
Experimental Protocols for GIAB-Based Benchmarking
Workflow for Comprehensive Variant Detection Assessment
Implementing a robust benchmarking protocol using GIAB resources requires systematic execution of specific steps from sample preparation through data analysis. The following workflow diagram illustrates the key stages in this process:
Diagram 1: GIAB Benchmarking Workflow
Step 1: Acquisition of GIAB Reference Materials Order DNA or cell lines for the appropriate GIAB reference sample(s) from the Coriell Institute for Medical Research. For comprehensive benchmarking, select samples with the most complete benchmark characterization (HG002 currently has the most extensive benchmarks) [63] [64]. The GIAB consortium has characterized multiple genomes, including a pilot genome (NA12878/HG001) and two trios of Ashkenazi Jewish and Han Chinese ancestry, all available as physical reference materials [63].
Step 2: Library Preparation and Sequencing Prepare sequencing libraries according to standardized protocols for your technology platform. For comprehensive assessment, consider using multiple sequencing technologies (short-read, linked-read, and long-read) to identify platform-specific strengths and limitations [64]. Recent studies have demonstrated successful benchmarking using Oxford Nanopore PromethION2 sequencers with ligation sequencing kits (SQK-LSK114) [68] [69], PacBio HiFi sequencing [70] [71], and Illumina short-read platforms [44].
Step 3: Data Processing and Alignment Process raw sequencing data through base calling (for signal-level data) and align to the appropriate reference genome (GRCh37, GRCh38, or T2T-CHM13) using standard aligners such as minimap2 for long reads or BWA-MEM for short reads [68] [69]. The choice of reference genome should match the benchmark files you plan to use for evaluation.
Step 4: Variant Calling Call variants using your selected pipeline(s). For small variants (SNVs and indels), tools such as Clair3, HaplotypeCaller, or DeepVariant are commonly used [68] [69]. For structural variants, Sniffles2 is frequently employed [68] [69]. Ensure that variant calling parameters are optimized for your specific technology and application.
Step 5: Benchmark Comparison Compare your variant calls against GIAB benchmark sets using standardized benchmarking tools. For small variants, use hap.py, which provides precision, recall, and F1 scores [69]. The formulas for these metrics are:
- Precision = True Positives / (True Positives + False Positives)
- Recall = True Positives / (True Positives + False Negatives)
- F1 Score = 2 × (Precision × Recall) / (Precision + Recall) [69]
For structural variants, use Truvari, which is specifically designed for comparing larger variants [66] [65]. When using Truvari for tandem repeat regions, improved comparison methods that handle variants greater than 4 bp in length and varying allelic representation are recommended [66].
Step 6: Stratified Performance Analysis Analyze performance metrics across different genomic contexts using GIAB stratification BED files [67]. This step is crucial for understanding how your method performs in challenging regions that may be relevant to your specific research questions, such as medically important genes or repetitive regions.
Step 7: Interpretation and Reporting Generate comprehensive reports that highlight strengths and weaknesses of your method. Focus particularly on performance in genomic contexts relevant to your intended applications, such as coding regions for exome studies or repetitive regions for neurological disorders.
Specialized Protocol for Tandem Repeat Analysis
Tandem repeats (TRs) represent particularly challenging genomic regions that require specialized benchmarking approaches. Recent efforts have created a TR benchmark for the GIAB HG002 individual that works across variant sizes and overcomes ambiguous representations [66]. The following protocol specializes in TR assessment:
Step 1: Data Acquisition and Processing Sequence the HG002 sample with long-read technologies (PacBio HiFi or Oxford Nanopore) that provide the read length and accuracy necessary to resolve repetitive regions. Process data according to the standard workflow in Section 3.1.
Step 2: TR-Aware Variant Calling Use TR-specific callers such as Straglr for short tandem repeats or specialized modes in SV callers for larger repeat expansions [68]. These tools are specifically designed to handle the unique challenges of variant representation in repetitive regions.
Step 3: Benchmark Comparison with TR-Optimized Tools Compare your TR variant calls against the GIAB TR benchmark using an improved version of Truvari that can handle both small (≥5 bp) and large (≥50 bp) variants simultaneously [66]. This enhanced approach includes variant harmonization to overcome representation differences across technologies and callers.
Step 4: Stratification with TR-Specific Contexts Analyze performance using TR-specific stratifications, including:
- TR regions with interspersed repeat elements
- Regions containing pathogenic TRs
- Variable number tandem repeats (VNTRs)
- CODIS TRs used in forensic applications [66]
This specialized approach is particularly valuable for researchers studying neurological disorders, forensic applications, or population genetics where TR variations play important roles.
Table 3: Essential Research Reagents and Computational Tools for GIAB Benchmarking
| Resource Category | Specific Tools/Resources | Function and Application |
|---|---|---|
| Reference Materials | GIAB DNA (e.g., HG002) from Coriell | Physical benchmark for wet-lab validation |
| Sequencing Platforms | Illumina, PacBio, Oxford Nanopore | Technology-specific performance assessment |
| Alignment Tools | BWA-MEM, minimap2 | Read alignment to reference genomes |
| Variant Callers | Clair3, DeepVariant, HaplotypeCaller | Small variant detection |
| SV Callers | Sniffles2, Manta, PBSV | Structural variant identification |
| TR Callers | Straglr, RepeatExpansions | Tandem repeat variant detection |
| Benchmarking Tools | hap.py, Truvari | Performance comparison against benchmarks |
| Stratification Resources | GIAB genomic stratifications BED files | Context-specific performance analysis |
| Visualization Tools | IGV, GenomePaint | Visual validation of variant calls |
Analysis and Interpretation of Benchmarking Results
Key Performance Metrics and Acceptance Criteria
Interpreting GIAB benchmarking results requires understanding both overall performance and context-specific metrics. The following diagram illustrates the relationship between different performance metrics and their implications for method validation:
Diagram 2: Benchmarking Metrics Relationship
For clinical-grade validation, the following performance thresholds are commonly targeted in genomically "easy" regions:
- SNV precision and recall: >0.99 [69]
- Indel precision: >0.92 with recall >0.83 [69]
- Structural variant precision and recall: Technology-dependent, with long-read technologies generally achieving >0.90 for many SV types [65]
However, these values typically decrease in challenging genomic regions, which is why stratified analysis is essential. Performance in medically relevant genes (MRGs) and tandem repeat regions may be significantly lower, highlighting areas for method improvement [66] [64].
Comparative Analysis Across Technologies
Benchmarking against GIAB resources has revealed important performance differences across sequencing technologies. Long-read sequencing platforms (PacBio and Oxford Nanopore) generally demonstrate superior performance for detecting structural variants and resolving complex genomic regions, while short-read technologies maintain advantages for SNV detection in non-repetitive regions [65] [69]. Recent advances in long-read sequencing, particularly PacBio HiFi reads and Oxford Nanopore ultra-long reads, have dramatically improved variant calling in previously problematic regions like segmental duplications and tandem repeats [66] [65].
When comparing your results to published benchmarks, consider the technology used, sequencing depth, and analysis pipeline. For example, a recent study using Oxford Nanopore sequencing of GIAB samples with Dorado basecalling and Clair3 variant calling achieved precision of 0.997 and recall of 0.992 for SNVs, while small indel identification approached precision of 0.922 and recall of 0.838 [69]. These values represent current benchmarks for this specific technology stack.
Advanced Applications and Future Directions
Leveraging Family-Based Benchmarks
While GIAB provides exceptional benchmarks for individual genomes, recent advances include family-based benchmarking using multi-generational pedigrees. The Platinum Pedigree dataset, based on the CEPH-1463 family, uses inheritance patterns across three generations to validate variants that would be impossible to confirm using single-sample approaches [71]. This approach has identified 11.6% more SNVs and 39.8% more indels in NA12878 compared to GIAB v4.2.1, particularly in complex genomic regions [71].
When using these family-based benchmarks, researchers can retrain variant callers such as DeepVariant, which has demonstrated error reductions of 38.4% for SNVs and 19.3% for indels when trained on the Platinum Pedigree truth set [71]. This approach is particularly valuable for developing methods targeting challenging genomic regions or for clinical applications requiring maximum sensitivity.
Emerging Benchmarks for Challenging Medically Relevant Genes
GIAB has recently developed specialized benchmarks for 273 Challenging Medically Relevant Genes (CMRGs) that include approximately 17,000 SNVs, 3,600 small indels, and 200 structural variants, most located in highly repetitive or complex regions [63] [64]. These benchmarks enable focused validation of methods for clinically important regions that have historically been difficult to characterize.
When working with CMRG benchmarks, researchers should:
- Prioritize genes relevant to their specific research focus
- Pay particular attention to performance in repetitive regions and segmental duplications
- Use the associated stratification files to understand context-specific performance limitations
- Consider supplementing with orthogonal validation for clinically actionable findings
Integration with the T2T Reference Genome
The recent completion of the telomere-to-telomere (T2T) CHM13 reference genome represents a significant advancement in genomic representation. GIAB has extended its stratifications to this new reference, highlighting the increase in hard-to-map and GC-rich regions in CHM13 compared to previous references [67]. These new stratifications facilitate the study of hundreds of new genes and their roles in phenotypes or diseases that were previously inaccessible.
Researchers can leverage the T2T-based benchmarks to:
- Characterize method performance in newly assembled genomic regions
- Investigate variation in centromeric satellite arrays and rDNA clusters
- Develop specialized approaches for heterochromatic regions
- Advance studies of population-specific variation in previously unresolved areas
As the field transitions to T2T-based references, GIAB benchmarks and stratifications will continue to provide the essential framework for methodological validation and improvement, ensuring that functional validation studies for genetic variants remain grounded in accurate genomic characterization.
Ensuring Rigor and Reproducibility: Validation Frameworks and Comparative Analytics
In the field of genomic medicine, the functional validation of genetic variants is a cornerstone for accurate diagnosis, drug development, and personalized treatment strategies. The convergence of advanced sequencing technologies and complex multi-omics data has made the construction of a robust validation framework more critical than ever. Such a framework ensures that variant calls and interpretations are accurate, precise, and reproducible, forming a reliable foundation for clinical and research decisions. This application note details standardized protocols and presents quantitative data for establishing a rigorous validation framework, providing researchers and drug development professionals with the tools to confidently assess genomic findings within the broader context of functional validation research.
Performance Benchmarks for Genomic Assays
A validation framework must be grounded on clearly defined performance metrics. The following benchmarks, derived from recent large-scale studies, provide reference standards for assessing assay quality.
Table 1: Key Performance Metrics from Recent Genomic Validation Studies
| Assay Type | Study Focus | Sensitivity / PPA | Specificity / NPA | Reproducibility | Limit of Detection (LoD) | Citation |
|---|---|---|---|---|---|---|
| Clinical Whole Genome Sequencing (WGS) | 78 actionable genes & PGx in 188 participants | Excellent sensitivity and specificity reported [72] | Accuracy: >99% [72] | N/A | N/A | [72] |
| Targeted RNA Sequencing (FoundationOneRNA) | 318 fusion genes in 189 tumor samples | 98.28% (Positive Percent Agreement) | 99.89% (Negative Percent Agreement) | 100% (for 10 pre-defined fusions) | 1.5 ng to 30 ng RNA input; 21-85 supporting reads [73] | [73] |
| Comprehensive Long-Read Sequencing | SNVs, Indels, SVs, and Repeat Expansions | 98.87% (for exonic SNVs/Indels) | >99.99% | N/A | N/A | [74] |
Experimental Protocols for Assay Validation
Protocol: Validation of a Clinical Whole Genome Sequencing (WGS) Assay
This protocol outlines the validation of a germline WGS assay for heritable disease and pharmacogenomics (PGx), based on the "Geno4ME" clinical implementation study [72].
1. Sample Selection and Collection:
- Cohort Design: Select a validation cohort comprising samples from a sufficient number of participants (e.g., 188). Include paired samples from different source materials (e.g., whole blood and saliva) to cross-validate specimen types [72].
- Orthogonal Validation: Ensure all samples have been previously sequenced at commercial reference laboratories or have characterized reference materials available for orthogonal comparison [72].
2. DNA Extraction and Library Preparation:
- Extraction: Purify genomic DNA from collected specimens (e.g., whole blood in EDTA tubes, saliva) using a standardized kit, such as the Qiagen QIAsymphony DSP Midi Kit [72].
- Library Prep: Utilize a PCR-free library preparation method to reduce bias and improve coverage in complex genomic regions. The Illumina DNA PCR-Free Prep, Tagmentation kit is recommended for this purpose [72].
3. Sequencing and Quality Control:
- Platform: Sequence libraries on a high-throughput platform like the Illumina NovaSeq 6000, targeting a minimum of 30x coverage [72].
- Quality Control (QC): Include a sequencing control in every run. The Illumina PhiX Control v3 Library is suitable, with error rates of less than 1% considered passing. Regularly sequence a germline variant QC sample with known variants to monitor pipeline performance [72].
4. Data Analysis and Variant Calling:
- Variant Calling: Process sequencing data through a bioinformatics pipeline optimized for SNVs, small insertions/deletions (indels), and copy-number variants (CNVs).
- Gene List: For the final clinical report, focus on a curated list of clinically actionable genes (e.g., 78 genes for hereditary conditions and 4 for PGx) as defined by guidelines from the ACMG and NCCN [72].
Protocol: Analytical Validation of a Targeted RNA Sequencing Assay
This protocol describes the validation of an RNA-based assay for fusion detection, as used for the FoundationOneRNA assay [73].
1. Sample and Material Acquisition:
2. RNA Sequencing:
- Assay Design: Employ a hybrid-capture based targeted RNA sequencing test designed to detect fusions in a specific set of genes (e.g., 318 genes) and measure gene expression [73].
- Orthogonal Comparison: Compare fusion calls against results from established orthogonal DNA- or RNA-based NGS assays to calculate Positive Percent Agreement (PPA) and Negative Percent Agreement (NPA) [73].
3. Data Analysis and Validation:
- Fusion Calling: Use the assay's proprietary pipeline to call fusions from the sequencing data.
- Precision Assessment: Re-sequence a subset of samples to assess intra-run and inter-run reproducibility for pre-defined target fusions [73].
- LoD Determination: Analyze the dilution series from fusion-positive cell lines. The LoD is defined as the lowest input quantity (e.g., 1.5 ng RNA) and the lowest number of supporting reads (e.g., 21 reads) at which the fusion is consistently detected [73].
Visualizing the Validation Workflow
The following diagram illustrates the core workflow and decision-making process for validating a genomic assay, integrating the key concepts from the protocols above.
The Scientist's Toolkit: Essential Research Reagents
A successful validation study relies on a suite of critical reagents and materials. The following table details key components for setting up a genomic validation framework.
Table 2: Key Research Reagent Solutions for Genomic Validation
| Reagent / Material | Function in Validation | Example Product / Specification |
|---|---|---|
| Biobanked Patient Specimens | Serve as the primary test material for assessing real-world performance. | Whole blood (EDTA tubes), saliva (Oragene-DNA kit) [72], FFPE tissue blocks [73]. |
| Reference Standards | Provide a benchmark for accuracy and precision measurements. | NIST-genome in a bottle (GIAB) samples (e.g., NA12878) [74]; fusion-positive cell lines [73]. |
| Nucleic Acid Extraction Kits | Ensure high-quality, pure input material for sequencing. | Qiagen QIAsymphony DSP Midi Kit (DNA) [72]; specialized kits for RNA from FFPE [73]. |
| PCR-Free Library Prep Kits | Minimize amplification bias, crucial for accurate variant calling and CNV analysis. | Illumina DNA PCR-Free Prep, Tagmentation kit [72]. |
| Targeted Sequencing Panels | Enrich for genes of interest, enabling focused validation and cost-effective sequencing. | Hybrid-capture panels for DNA (e.g., for 78 genes [72]) or RNA (e.g., for 318 fusion genes [73]). |
| Orthogonal Assays | Provide an independent method for comparison to calculate PPA, NPA, and accuracy. | Orthogonal NGS panels, SNV arrays, fluorescence in situ hybridization (FISH) [73], microarray (aCGH) [72]. |
The integration of accuracy, precision, and reproducibility assessments into a unified validation framework is non-negotiable for advancing functional genetic variant research. The protocols and data presented here provide a concrete foundation for laboratories to build and benchmark their own assays. As sequencing technologies continue to evolve toward long-read platforms and AI-driven analysis, the core principles of rigorous validation—clear metrics, robust protocols, and standardized reagents—will remain paramount. Adopting such a framework ensures that genomic discoveries are not only scientifically sound but also reliably translatable into clinical diagnostics and targeted drug development.
Within the field of genomics, the functional validation of genetic variants hinges on the accurate detection and characterization of specific sequences from next-generation sequencing (NGŠ) data. For researchers in drug development and microbial diagnostics, this often involves analyzing whole-genome sequencing (WGS) data to identify antimicrobial resistance (AMR) genes, virulence factors, and typing markers. Three widely used bioinformatics approaches for this purpose are BLAST+, KMA, and SRST2, each employing a distinct methodology—alignment, k-mer mapping, and read mapping, respectively [75] [76]. The choice of tool impacts the sensitivity, specificity, and speed of analysis, which are critical parameters for validating genetic variants in both clinical and research settings. This application note provides a comparative analysis of these three methods, supported by quantitative data and detailed experimental protocols, to guide researchers in selecting the most appropriate tool for their specific validation needs.
Comparative Analysis of Tools and Performance
The three tools represent different methodological philosophies for comparing sequencing data against reference databases.
- BLAST+ (Basic Local Alignment Search Tool) is a traditional sequence alignment tool that uses heuristic algorithms to find regions of local similarity between sequences. It is often used on de novo assembled contigs [75].
- KMA (k-mer Alignment) is designed to map raw reads directly against redundant databases. It uses k-mer seeding for speed and the Needleman-Wunsch algorithm for accurate alignment. Its novel ConClave scoring scheme helps resolve ties when reads map equally well to multiple database entries [77].
- SRST2 (Short Read Sequence Typing for Bacterial Pathogens) also maps raw reads directly against reference sequences but uses Bowtie2 for alignment and extensive pre- and post-processing to resolve gene assignments and call variants [77] [75].
Evaluations across multiple studies reveal distinct performance profiles for each tool. A validation study for a Shiga toxin-producing Escherichia coli (STEC) workflow demonstrated that all three methods achieved high performance, with repeatability, reproducibility, accuracy, precision, sensitivity, and specificity mostly above 95% for most assays [75]. Similarly, a study on Salmonella serotype and AMR prediction found all tools had ≥ 99% accuracy for predicting resistance to most antibiotics tested [78].
A key differentiator is performance with redundant databases, where highly similar sequences (like AMR gene families) are common. KMA was specifically designed for this challenge and has been shown to outperform other methods in both accuracy and speed when mapping raw reads against redundant databases [77]. SRST2 handles redundancy by performing pre-clustering of database sequences [77].
Table 1: Comparative Overview of BLAST+, KMA, and SRST2
| Feature | BLAST+ | KMA (k-mer Alignment) | SRST2 (Short Read Sequence Typing) |
|---|---|---|---|
| Primary Method | Alignment of assembled contigs [75] | Direct k-mer based read mapping [77] [75] | Direct read mapping with Bowtie2 [75] |
| Typical Input | Assembled contigs (FASTA) | Raw reads (FASTQ) | Raw reads (FASTQ) |
| Key Feature | Heuristic search for local similarity; widely considered a gold standard | ConClave scheme for resolving ties in redundant databases [77] | Pre- and post-processing to handle multi-mapping reads [77] |
| Advantages | Highly accurate; versatile for various sequence types | Fast and memory-efficient; accurate with redundant databases [77] | Integrated approach for typing and resistance gene detection |
| Limitations | Slower on large datasets; requires a separate assembly step | - | Database pre-clustering may reduce resolution |
| Common Application | Gene detection from assembled genomes | Gene detection and typing from raw reads [77] [75] | Bacterial typing and AMR profiling from raw reads [75] |
Table 2: Performance Comparison in Antimicrobial Resistance (AMR) Gene Detection
| Performance Metric | BLAST+ | KMA | SRST2 | Context |
|---|---|---|---|---|
| Accuracy | > 95% [75] | > 95% [75] | > 95% [75] | Validation on STEC isolates [75] |
| Accuracy | ≥ 99% (for most drugs) [78] | ≥ 99% (for most drugs) [78] | ≥ 99% (for most drugs) [78] | Analysis of Salmonella isolates [78] |
| Streptomycin Accuracy | ~94.6% [78] | ~94.6% [78] | ~94.6% [78] | Some tools missed genes for a few isolates [78] |
| Speed | Slower | Faster [77] | Intermediate | Comparison mapping raw reads against redundant databases [77] |
Detailed Experimental Protocols
Workflow for Comparative Validation of Genetic Variants
The following diagram outlines a generalized workflow for comparing the performance of BLAST+, KMA, and SRST2 in a validation study, such as characterizing bacterial isolates.
Protocol 1: Gene Detection using BLAST+ on Assembled Contigs
This protocol uses the common approach of conducting a BLAST search on contigs assembled from raw sequencing reads [75].
Key Research Reagents:
- SPAdes: An assembly toolkit used to generate contigs from raw Illumina reads [75].
- BLAST+: The standalone command-line suite of BLAST tools [79].
- Reference Database (e.g., CARD/ResFinder): A curated database of AMR genes or other genetic variants of interest [75] [80].
Procedure:
- De novo Assembly:
- Assemble the quality-controlled paired-end reads using SPAdes with default parameters for bacterial genomes to produce a set of contigs in FASTA format [75].
- Database Preparation:
- Format your reference gene database (e.g., a FASTA file of AMR gene sequences) into a BLAST database using the
makeblastdbcommand. - Example:
makeblastdb -in reference_genes.fasta -dbtype nucl -out my_amr_db
- Format your reference gene database (e.g., a FASTA file of AMR gene sequences) into a BLAST database using the
- Execute BLAST Analysis:
- Run
blastn(for nucleotide sequences) to search the assembled contigs against your custom database. - Use a command with the following structure, adjusting parameters like
-evalueand-perc_identityas needed [79]:
- Run
- Result Interpretation:
- Parse the BLAST output (e.g., tabular format 6) to identify contigs with significant hits to the reference database based on percent identity and e-value thresholds.
Protocol 2: Direct Read Mapping and Typing using KMA
This protocol leverages KMA's speed and accuracy for analyzing raw sequencing reads without prior assembly [77] [75].
Key Research Reagents:
- KMA: The k-mer alignment tool [77].
- Installation: Available from GitHub (https://github.com/cge-ku/KMA).
- Indexed KMA Database: A reference database formatted for use with KMA. This can be created from a FASTA file using the KMA command.
Procedure:
- Database Indexing:
- Prepare your reference database for KMA. This step creates the necessary index files.
- Example:
kma_index -i reference_genes.fasta -o my_kma_db
- Execute KMA Analysis:
- Run KMA with the raw, quality-filtered reads and the indexed database.
- Example command:
- Result Interpretation:
- KMA generates a
.resfile containing a summary of results for each template in the database, including template coverage, identity, and depth. The built-in ConClave scheme resolves multi-mapping reads [77].
- KMA generates a
Protocol 3: Resistance Profiling using SRST2
SRST2 provides an integrated pipeline for gene detection and allele typing from short reads [75].
Key Research Reagents:
- SRST2: The SRST2 script and its dependencies (Bowtie2, Python, Samtools) [75].
- Clustered Reference Database (FASTA): SRST2 often uses databases where sequences have been clustered at a specific identity threshold (e.g., 90%) to reduce redundancy [77].
Procedure:
- Database Preparation:
- SRST2 can use a FASTA file of reference gene alleles. It is recommended to use a pre-clustered database to improve mapping accuracy.
- Execute SRST2 Analysis:
- Run the
srst2command with the appropriate flags for your data. - Example command:
- Run the
- Result Interpretation:
- SRST2 produces files including a
*.genes.txtfile that lists the detected genes and their alignment statistics. It reports the best-matching allele for each gene in the database [75].
- SRST2 produces files including a
The Scientist's Toolkit
Table 3: Essential Research Reagents and Databases
| Reagent / Resource | Function / Description | Relevance to Functional Validation |
|---|---|---|
| Illumina WGS Data | Provides the raw sequencing data (FASTQ) from bacterial isolates. | The foundational input data for all three bioinformatics approaches. |
| CARD (Comprehensive Antibiotic Resistance Database) | A curated resource containing AMR genes, their products, and associated phenotypes [80]. | A key reference database for validating resistance-conferring genetic variants. |
| ResFinder | A database dedicated to AMR genes, often used for genotypic resistance prediction [77] [76]. | Used to compare tool performance against a known, curated set of resistance determinants. |
| PubMLST / EnteroBase | Databases for multi-locus sequence typing (MLST) and core genome MLST (cgMLST) schemes [81]. | Provides reference alleles for validating typing assays and assessing strain relatedness. |
| SPAdes Assembler | A software tool for assembling genomes from sequencing data [75]. | Used in the BLAST+ protocol to generate contigs from raw reads. |
| Galaxy @Sciensano | A public bioinformatics portal offering "push-button" pipelines that incorporate these tools for pathogen characterization [81]. | Provides a user-friendly, validated implementation of the described methodologies, useful for benchmarking. |
The choice between BLAST+, KMA, and SRST2 depends on the specific requirements of the validation project. For ultimate accuracy when working with assembled genomes, BLAST+ remains a robust and trusted standard. However, for high-throughput scenarios, especially those involving redundant databases like those for AMR genes, KMA offers a compelling combination of speed and precision by directly analyzing raw reads and intelligently resolving ambiguous mappings [77]. SRST2 also provides an accurate, read-based approach that is well-integrated into typing workflows [75] [78].
For researchers focused on the functional validation of genetic variants in pathogens, the following recommendations can be made:
- For maximum throughput and speed in public health or clinical surveillance settings, KMA is often the optimal choice.
- When integration with existing assembly-based workflows is key, or when a well-established, versatile tool is needed, BLAST+ is appropriate.
- For projects specifically focused on bacterial typing and resistance gene profiling with minimal setup, SRST2 is highly effective.
Ultimately, the validation of any bioinformatics pipeline must be "fit-for-purpose." The high concordance (>95%) demonstrated by all three methods in controlled studies [75] [78] provides confidence in their reliability. Utilizing publicly available, validated platforms like Galaxy @Sciensano, which implement these very tools under accreditation standards [81], can significantly streamline the process of establishing reproducible and traceable bioinformatics analyses for genetic variant research.
The rapid and accurate identification of bacterial pathogens is a cornerstone of effective public health surveillance. While Whole Genome Sequencing (WGS) has emerged as a powerful tool for this purpose, its reliability for routine use depends entirely on rigorous analytical validation and standardization. This case study details the complete validation of a bacterial WGS workflow, from sample to final variant call, ensuring its fitness for public health applications. The process is framed within the broader context of functional validation of genetic variants, emphasizing the critical link between robust bioinformatics and confident biological interpretation.
The entire WGS process, from sample receipt to final reported variant, was validated as an integrated system. The strategy focused on establishing key performance characteristics for different variant types and ensuring the workflow was reproducible and met international quality standards [82] [83].
Workflow Diagram
The diagram below illustrates the core steps of the WGS workflow and the parallel validation activities conducted at each stage.
Experimental Protocols
Sample Preparation and Sequencing
This protocol ensures the generation of high-quality, PCR-free WGS libraries suitable for comprehensive variant detection [72].
- Sample Collection and Nucleic Acid Extraction: Bacterial isolates are cultured and harvested. Genomic DNA is extracted using the Qiagen QIAsymphony DSP Midi Kit (catalog 937,255). DNA quantity and quality are assessed using fluorometry and gel electrophoresis.
- Library Preparation: Sequencing libraries are prepared from 300–500 ng of genomic DNA using the Illumina DNA PCR-Free Prep, Tagmentation kit (catalog 20041795). This PCR-free approach reduces amplification bias and improves variant detection in complex regions [72].
- Sequencing: Libraries are sequenced on an Illumina NovaSeq 6000 platform using an S4 flow cell. The target is an average coverage of 30x across the genome. The Illumina PhiX Control v3 library is spiked in (at ~1% concentration) for run quality control, with error rates of less than 1% considered passing [72].
Bioinformatics and Variant Calling
This protocol outlines the secondary analysis steps for converting raw sequencing data into a high-confidence set of genetic variants [82].
- Read Alignment and QC: Raw sequencing reads (FASTQ) are aligned to an appropriate reference genome using the BWA-MEM aligner. The resulting BAM files are processed to mark duplicate reads and undergo base quality score recalibration. Alignment quality metrics are assessed against the GA4GH WGS QC Standards [83].
- Variant Calling: A multi-caller approach is employed for comprehensive variant detection [84] [85].
- Variant Filtering and Annotation: Raw variant calls are filtered based on quality scores, depth of coverage, and strand bias. The final set of variants is annotated using databases and tools to predict functional impact.
Orthogonal Validation and Benchmarking
This protocol describes the methods for independently verifying the accuracy of the WGS-derived variants [72] [86].
- Orthogonal Testing: A subset of samples is sent for testing at a commercial reference laboratory using established, independent methods (e.g., targeted panels, Sanger sequencing). Variant calls from the WGS workflow are compared to the orthogonal results to calculate concordance [86].
- Benchmarking with Reference Materials: DNA from well-characterized reference samples with known variants is processed through the entire workflow. The Genome-In-A-Bottle (GIAB) consortium provides such gold-standard datasets for benchmarking [84] [82]. Performance is assessed using a standardized benchmarking workflow that calculates sensitivity, precision, and F-measure [82].
Results and Performance Metrics
Analytical Performance of the WGS Workflow
The validated WGS workflow demonstrated excellent performance across different variant types, as determined by orthogonal testing and benchmarking [72] [86].
Table 1: Summary of Analytical Performance Metrics
| Variant Type | Sensitivity (%) | Specificity (%) | Precision (%) | Orthogonal Method Used |
|---|---|---|---|---|
| Single Nucleotide Variants (SNVs) | 100 | 100 | 100 | Commercial panel testing [86] |
| Small Insertions/Deletions (Indels) | 100 | 100 | 100 | Commercial panel testing [86] |
| Copy Number Variants (CNVs) | 100 | 100 | 100 | Commercial panel testing [86] |
| Deletions (50 bp - 1 kbp) | >99 (Varies by caller) | >99 (Varies by caller) | >99 (Varies by caller) | PCR-validated gold standard [84] |
Impact of Sequencing Coverage and Panel Size
The performance of variant detection is influenced by technical parameters such as sequencing coverage and the scope of the investigation.
Table 2: Impact of Technical Parameters on Performance
| Parameter | Impact on Variant Detection | Validation Evidence |
|---|---|---|
| Sequencing Coverage (30x) | No significant correlation between coverage (22.7x - 60.8x) and diagnostic success, indicating 30x is sufficient for germline variants [87]. | Pearson r = -0.1, P = 0.13 [87] |
| Multi-modal Panel Scalability | Detection of >80% of gDNA targets in >80% of cells, with minimal performance decrease even when scaling from 120 to 480 targets [6]. | High correlation (r > 0.9) for shared targets between panel sizes [6] |
The Scientist's Toolkit
This section lists key reagents, controls, and software tools essential for implementing and validating a bacterial WGS workflow.
Table 3: Essential Research Reagent Solutions for WGS Workflow Validation
| Item | Function / Utility | Specific Example / Note |
|---|---|---|
| Illumina DNA PCR-Free Prep, Tagmentation Kit | Library preparation without PCR amplification bias, improving SV and complex variant detection. | Catalog #20041795 [72] |
| Genome in a Bottle (GIAB) Reference Materials | Gold-standard samples with curated variant calls for benchmarking pipeline accuracy. | Enables calculation of sensitivity and precision [84] [82] |
| PhiX Control v3 | Sequencing run quality control; monitors error rates and cluster generation. | Error rates <1% considered passing [72] |
| GA4GH WGS QC Standards | A unified framework of QC metrics and definitions for consistent quality assessment across datasets and institutions. | Ensures data interoperability and reliability [83] |
| hap.py / vcfeval | Benchmarking tools for comparing variant calls to a truth set, calculating performance metrics. | Part of a standardized, reproducible benchmarking workflow [82] |
| Tapestri Technology (Mission Bio) | Enables targeted single-cell DNA–RNA sequencing (SDR-seq) for functional phenotyping of variants. | Links genotype to gene expression at single-cell resolution [6] |
Functional Validation and Advanced Applications
Connecting variant identification to biological function is the ultimate goal of genomic surveillance. The following diagram and text outline advanced methods for functional characterization.
Pathway for Functional Validation of Genomic Variants
This workflow transitions from initial variant discovery to mechanistic insight, strengthening public health recommendations.
- Computational Prediction: Following variant identification, in silico tools are used to predict the impact of amino acid substitutions on protein structure and function, and to assess if variants disrupt splicing or regulatory regions [88].
- In Silico Saturation Genome Editing: Computational protocols can be used to model the functional consequences of all possible variants in a gene of interest, providing a map of critical functional domains and helping prioritize newly discovered variants [89].
- Single-Cell DNA–RNA Sequencing (SDR-seq): This advanced method allows for the simultaneous profiling of genomic DNA loci and transcriptomic data in thousands of single cells. In a public health context, this could be applied to link a specific resistance variant (genotype) directly to changes in gene expression profiles (phenotype) within a heterogeneous bacterial population, providing powerful mechanistic insight [6].
- Machine Learning for Automated Refinement: Convolutional Neural Networks (CNNs) can be trained to filter out technical artefacts from true variants by processing sequencing data represented as images, standardizing the refinement process and improving reproducibility [85].
This case study demonstrates that validating a bacterial WGS workflow for public health surveillance requires a multi-faceted approach. The combination of rigorous analytical validation, adherence to global quality standards, and the integration of functional investigation frameworks ensures that genomic data is not only accurate but also biologically meaningful. This end-to-end validation and functional contextualization transform WGS from a simple typing tool into a powerful system for understanding pathogen evolution and guiding public health interventions.
The functional validation of genetic variants represents a cornerstone of modern genomic research, bridging the gap between statistical association and biological mechanism. In this context, BayesRC has emerged as a powerful computational method that integrates biological priors into genomic analysis to enhance both quantitative trait locus (QTL) discovery and genomic prediction accuracy. Unlike conventional genomic selection approaches that treat all genetic variants equally, BayesRC incorporates independent biological knowledge about functional genomic elements, enabling more precise identification of causal variants and improved trait prediction [90]. This approach is particularly valuable for research aimed at validating the functional significance of genetic polymorphisms, as it leverages existing biological evidence to prioritize variants most likely to influence phenotypic expression.
The fundamental innovation of BayesRC lies in its ability to objectively incorporate biological evidence from diverse sources—including functional annotations, gene expression studies, and known causal variants—within a robust Bayesian framework [90]. This methodology represents a significant advancement over post-hoc annotation of association results, as it allows biological information to directly influence the analytical model based on empirical evidence of enrichment within the data being analyzed. For researchers focused on functional validation, BayesRC provides a systematic approach for determining which biological annotations truly improve causal variant detection and prediction accuracy for specific traits.
Theoretical Foundation and Methodological Framework
Core Algorithm and Biological Integration
BayesRC extends the BayesR method, which models SNP effects using a mixture of normal distributions, by introducing variant classes based on biological priors [90] [91]. The method operates through several key computational steps:
- Variant Classification: Each genotyped variant is allocated a priori to specific classes (where c ≥ 2) based on biological information, with each class potentially differing in the probability of containing causal variants [90].
- Class-Specific Mixture Models: Within each class, variant effects follow a mixture of four normal distributions with class-specific proportions (P₁c, P₂c, P₃c, P₄c) [91].
- Bayesian Learning: The proportion of variants in each distribution is updated each iteration within each class using a Dirichlet prior, allowing the data to inform class-specific distributions [91].
The mathematical formulation can be represented as:
y = Xβ + ε
where the prior for β depends on the biological class membership of each variant, with:
βⱼ | class = c ~ π₁cN(0,0) + π₂cN(0,σ²₂c) + π₃cN(0,σ²₃c) + π₄cN(0,σ²₄_c)
This framework allows variants in biologically enriched classes to have different probabilities of being causal or having larger effects, thereby incorporating functional knowledge directly into the analysis [90] [91].
Advancements in Bayesian Methods
Recent advancements have further refined the BayesRC approach. The SBayesRC method extends this framework to work with GWAS summary statistics rather than individual-level data, incorporating functional annotations through a low-rank model and hierarchical multicomponent mixture prior [92]. This implementation allows the method to scale to whole-genome analyses with millions of variants while leveraging information from numerous functional annotations.
SBayesRC uniquely allows annotations to affect both the probability that a SNP is causal and the distribution of its effect sizes, providing more accurate modeling of the underlying genetic architecture [92]. The method employs a multicomponent annotation-dependent mixture prior that jointly learns annotation parameters and SNP effects from the data, refining signals from functional annotations more effectively than previous approaches.
Figure 1: BayesRC Analytical Framework - Integrating biological priors with genomic data to enhance QTL discovery and genomic prediction.
Application Notes and Performance Evaluation
Implementation and Class Definitions
In practical implementation, BayesRC requires careful definition of variant classes based on biological knowledge. Research applications have employed several successful class definition strategies:
- Sequence-Based Classification: Variants categorized as non-synonymous coding (NSC), regulatory (REG), or standard chip array (CHIP) variants, with the hypothesis that NSC variants are most enriched for causal mutations [90] [91].
- Candidate Gene Approaches: Variants within genes identified through independent studies (e.g., gene expression analyses) as potentially related to the trait of interest [90].
- Multi-Omics Integration: Variants prioritized using diverse functional evidence including evolutionary conservation, selection signatures, expression QTLs (eQTLs), and metabolic QTLs (mQTLs) [93].
For dairy cattle milk production traits, BayesRC implementations have defined classes using a set of 790 candidate genes identified from independent microarray gene expression studies, supplemented with known major effect genes like DGAT1 [90] [91]. This approach demonstrates how prior biological evidence can be systematically incorporated into genomic analysis.
Performance Metrics and Comparative Analysis
Extensive validation studies have demonstrated the performance advantages of BayesRC approaches compared to methods that do not incorporate biological priors.
Table 1: Performance Comparison of BayesRC Methods Across Studies
| Trait Category | Method | Comparison | Improvement | Study |
|---|---|---|---|---|
| Simulated Traits | BayesRC vs BayesR | QTL detection power | Significant increase | [90] |
| Dairy Cattle Milk Production | BayesRC vs BayesR | Genomic prediction accuracy | Equal or greater power | [90] |
| Complex Human Traits | SBayesRC vs SBayesR | Prediction accuracy (European ancestry) | 14% improvement | [92] |
| Cross-Ancestry Prediction | SBayesRC vs SBayesR | Prediction accuracy | Up to 34% improvement | [92] |
| 50 Complex Traits/Diseases | SBayesRC vs LDpred2 | Prediction accuracy | Outperformed | [92] |
The improvement in prediction accuracy is particularly pronounced in validation populations that are not closely related to the reference population, demonstrating that biological priors help maintain portability across diverse genetic backgrounds [90] [92]. For cross-ancestry prediction, SBayesRC achieved up to 34% improvement compared to the baseline SBayesR method that does not use annotations [92].
Table 2: Heritability Enrichment Across Functional Categories in Beef Cattle
| Functional Category | Enrichment Fold | Key Findings | Reference |
|---|---|---|---|
| Evolutionary Conservation | 31.78× | Highest per-SNP contribution | [93] |
| Selection Signatures | 14.48× | Significant heritability enrichment | [93] |
| Transcriptomics | Low | Moderate enrichment | [93] |
| Metabolomics | Low | Moderate enrichment | [93] |
| Top 10% Variants | 11.6% (BayesB) 7.54% (GBLUP) | Increased prediction accuracy | [93] |
The analysis of functional enrichments across diverse biological categories reveals that evolutionary constrained regions contribute most significantly to prediction accuracy, with the largest per-SNP contribution from nonsynonymous SNPs [92] [93].
Experimental Protocols
Protocol 1: Implementation of BayesRC for QTL Discovery
Objective: Identify quantitative trait loci (QTL) for complex traits using BayesRC with biological priors.
Materials and Reagents:
- Genotype data (SNP array or sequence variants)
- Phenotype measurements for target trait
- Biological annotation resources (e.g., gene sets, functional annotations)
Procedure:
Data Preparation and Quality Control
Variant Annotation and Classification
- Annotate variants using functional prediction tools (e.g., SnpEff) [93]
- Classify variants into biological categories:
- Non-synonymous coding (NSC) variants
- Regulatory regions (REG) including 5kb up/downstream of genes
- Intergenic variants (CHIP) [90]
- Alternatively, assign variants to classes based on candidate gene lists from independent studies [90]
BayesRC Analysis
Posterior Analysis
- Identify variants with high posterior inclusion probabilities (PIP)
- Calculate posterior means of SNP effects
- Determine proportion of genetic variance explained by each functional class
Expected Outcomes: Enhanced detection of causal variants, particularly those in biologically prioritized categories, with improved fine-mapping resolution compared to standard methods.
Protocol 2: Genomic Prediction with Biological Priors
Objective: Develop genomic prediction models with improved accuracy using BayesRC.
Materials:
- Training population with genotypes and phenotypes
- Validation population with genotypes
- Functional annotations (e.g., BaselineLD, tissue-specific annotations)
Procedure:
Reference Population Construction
Functional Annotation Integration
Model Training
Validation and Assessment
- Calculate polygenic scores in validation samples
- Assess prediction accuracy as correlation between predicted and observed phenotypes
- Compare with alternative methods (e.g., BayesR, GBLUP, LDpred2)
Expected Outcomes: Improved prediction accuracy, particularly for distantly related or cross-ancestry validation populations, with better capture of functional variants.
Figure 2: BayesRC Experimental Workflow - Key steps for implementing BayesRC in genetic studies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for BayesRC Implementation
| Resource | Type | Function | Availability |
|---|---|---|---|
| GCTB Software | Analysis Tool | Implements BayesRC/SBayesRC methods | https://gctbhub.cloud.edu.au/ [94] |
| BaselineLD v2.2 | Functional Annotations | 96 genomic annotations for functional partitioning | Provided with GCTB [92] [94] |
| 1000 Bull Genomes | Reference Panel | Imputation of sequence variants in cattle | Project Consortium [90] |
| FarmGTEx | Expression Atlas | Tissue-specific eQTLs for farm animals | Public Repository [93] |
| SnpEff | Annotation Tool | Functional annotation of genetic variants | Open Source [93] |
| PLINK | Data Management | Genotype quality control and filtering | Open Source [90] |
BayesRC represents a significant methodological advancement in genomic analysis by systematically integrating biological prior knowledge to enhance both QTL discovery and genomic prediction. The approach demonstrates consistent improvements in statistical power and prediction accuracy across diverse traits and species, with particular utility for cross-population predictions. For functional validation studies, BayesRC provides a robust framework for prioritizing variants based on both statistical evidence and biological plausibility.
As biological knowledge continues to accumulate through functional genomics initiatives, the utility of BayesRC and related methods is expected to grow. Future developments will likely focus on integrating more diverse types of biological information, including single-cell omics data, spatial transcriptomics, and epigenetic modifications, further refining our ability to identify functionally relevant genetic variants and accurately predict complex traits.
Conclusion
Functional validation is the crucial bridge that transforms a genetic correlation into a mechanistic understanding of disease. By integrating diverse methodological approaches—from wet-lab assays to sophisticated bioinformatics and AI—researchers can resolve the uncertainty of VUSs, leading to more accurate diagnoses, informed therapeutic strategies, and robust genomic medicine. Future progress hinges on increased standardization of validation pipelines, the development of shared, high-quality reference datasets, and the broader integration of multi-omics and machine learning technologies. These advances will be foundational for realizing the full potential of personalized medicine, ensuring that genomic findings can be translated into confident clinical actions.
References
- 1. Variants of uncertain significance: At the crux of diagnostic ... [https://www.sciencedirect.com/science/article/abs/pii/S0378111925003762]
- 2. AVE Alliance Working Group Developing International ... [https://brotmanbaty.org/news/ave-alliance-working-group-developing-international-guidelines-for-genetic]
- 3. The Frequency and Reclassification of Variants Uncertain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577467/]
- 4. Reassessment of variants of uncertain significance in ... [https://www.nature.com/articles/s41431-025-01911-z]
- 5. A quantitative, Bayesian-informed approach to gene-specific ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01536-3]
- 6. Functional phenotyping of genomic variants using joint ... [https://www.nature.com/articles/s41592-025-02805-0]
- 7. High-throughput screening of human genetic variants by ... [https://www.sciencedirect.com/science/article/pii/S2666979X25000709]
- 8. Creating an atlas of variant effects to resolve ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/40890511/]
- 9. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 10. Frontiers | Integrating next-generation sequencing and artificial... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1568205/full]
- 11. Recommendations for application of the functional evidence... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-019-0690-2]
- 12. The Next-Generation Sequencing Quality Initiative and ... [https://wwwnc.cdc.gov/eid/article/31/13/24-1175_article]
- 13. for the Protocol evaluation of functional using... genetic variants [https://pubmed.ncbi.nlm.nih.gov/40198219/]
- 14. Standards and guidelines for the interpretation of ... [https://www.nature.com/articles/gim201530]
- 15. Recommendations for application of the functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6938631/]
- 16. Recommendations for application of the functional evidence ... [https://pubmed.ncbi.nlm.nih.gov/31892348/]
- 17. Specifications of the ACMG/AMP variant curation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12520758/]
- 18. Consultation informs strategies for improving the use of ... [https://www.sciencedirect.com/science/article/pii/S0002929725001831]
- 19. Sequence Variant Interpretation [https://clinicalgenome.org/working-groups/sequence-variant-interpretation/]
- 20. functional validation of genetic variants - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5959958/]
- 21. Functional validation of variants of unknown significance ... [https://www.sciencedirect.com/science/article/pii/S0378111922001068]
- 22. From correlation to causation using directed topological ... [https://pubmed.ncbi.nlm.nih.gov/37743033/]
- 23. Editorial: Functional study of novel VUS (variant of ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1578736/full]
- 24. AlphaLISA SureFire Ultra Human and Mouse Phospho- ... [https://www.revvity.com/product/alpha-sf-ultra-stat1-py701-500-alsu-pst1-a500]
- 25. EGFR-STAT1 pathway drives fibrosis initiation in ... [https://www.nature.com/articles/s41467-025-64648-9]
- 26. DHR test for chronic granulomatous disease [https://www.cytometry.org/newsletters/eICCS-2-1/article6.php]
- 27. The value of DHR-enzyme-linked immunosorbent assay in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12176808/]
- 28. Strategies for CRISPR-based knock-ins in primary human ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1589729/full]
- 29. Advancing CRISPR genome editing into gene therapy clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 30. Characterizing and controlling CRISPR repair outcomes in ... [https://www.nature.com/articles/s41467-025-66058-3]
- 31. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 32. Optimization of gene knockout approaches and sgRNA ... [https://www.nature.com/articles/s41598-025-24184-4]
- 33. A simple validation and screening method for CRISPR/Cas9 ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0312722]
- 34. CMN Weekly (31 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-31-october-2025-your-weekly-crispr-medicine-news/]
- 35. CRISPR/Cas9 Methods for Identification and Validation of ... [https://pubmed.ncbi.nlm.nih.gov/40029521/]
- 36. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 37. RNA sequencing and immunohistochemistry jointly ... [https://www.nature.com/articles/s41598-025-12780-3]
- 38. How to Structure Your Multi-Omics Data: Knowledge Graph + ... [https://blackthorn.ai/blog/how-to-structure-your-multi-omics-data/]
- 39. Integrating Multi-Omics for Precision Medicine: 2025 Guide [https://lifebit.ai/blog/integrating-multi-modal-genomic-and-multi-omics-data-for-precision-medicine/]
- 40. A review on multi-omics integration for aiding study design of ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11925-y]
- 41. Validation of genetic variants from NGS data using deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10116675/]
- 42. Using artificial intelligence (AI) to model clinical variant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570631/]
- 43. Learning a refinement model for variant analysis in non ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11921-2]
- 44. Analytical Validation of a Genomic Newborn Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551001/]
- 45. A quantitative benchmark of neural network feature ... [https://www.nature.com/articles/s41598-024-82583-5]
- 46. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 47. Characterization and mitigation of artifacts derived from NGS ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10157-w]
- 48. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 49. Sample Preparation for NGS – A Comprehensive Guide [https://frontlinegenomics.com/sample-preparation-for-ngs-a-comprehensive-guide/]
- 50. Statistical guidelines for quality control of next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8408346/]
- 51. Functional Validation of Candidate Genes Detected by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5940157/]
- 52. A pipeline‐friendly software tool for genome diagnostics to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9744518/]
- 53. Health Data Interoperability & Integration in 2025 [https://talencio.com/breaking-barriers-health-data-interoperability-integration-in-2025/]
- 54. What is Workflow Automation? [https://www.atlassian.com/agile/project-management/workflow-automation]
- 55. 5 Principles of Modular Workflow Design [https://www.prompts.ai/en/blog/5-principles-of-modular-workflow-design]
- 56. 6 Actionable Ways To Improve Your Cloud Efficiency [https://www.cloudzero.com/blog/cloud-efficiency/]
- 57. A Comprehensive Guide to Workflow Automation [https://www.hyland.com/en/resources/terminology/workflow/automation]
- 58. Scaling Large Workflows Part 1: Embracing a Modular ... [https://neota.com/scaling-large-workflows-part-1-embracing-a-modular-approach/]
- 59. What is Modular Design and How to Implement it in 5 Easy ... [https://denovers.com/blog/what-is-modular-design/]
- 60. 8 Ways to Optimize Your Cloud Efficiency & Measure ROI [https://www.tierpoint.com/blog/cloud-efficiency/]
- 61. How Cloud Computing Enhances Business Efficiency [https://baymcp.com/how-cloud-computing-enhances-business-efficiency/]
- 62. 7 Workflow Best Practices for Any Organization [https://gravityflow.io/articles/workflow-automation-best-practices/]
- 63. Genome in a Bottle | NIST [https://www.nist.gov/programs-projects/genome-bottle]
- 64. Genomic variant benchmark: if you cannot measure it, you ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-023-03061-1]
- 65. Genome in a Bottle Consortium Describes Human ... [https://www.pacb.com/human-genetics-research/genome-in-a-bottle-consortium-describes-human-genome-structural-variation-benchmark/]
- 66. Analysis and benchmarking of small and large genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11952744/]
- 67. The GIAB genomic stratifications resource for human ... [https://www.nature.com/articles/s41467-024-53260-y]
- 68. Genome in a Bottle Data Release 2025.01 - EPI2ME Labs [https://epi2me.nanoporetech.com/giab-2025.01/]
- 69. Benchmarking nanopore sequencing and rapid genomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11549486/]
- 70. Datasets - PacBio - Highly accurate long-read sequencing [https://www.pacb.com/connect/datasets/]
- 71. Family-Based Genomics Benchmark Promises More Accurate ... [https://www.bio-itworld.com/news/2025/08/20/family-based-genomics-benchmark-promises-more-accurate-variant-detection]
- 72. Design and validation of a clinical whole genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554564/]
- 73. Analytical validation (accuracy, reproducibility, limit of ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0329697]
- 74. Validation of a comprehensive long-read sequencing ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1499456/full]
- 75. Validation strategy of a bioinformatics whole genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8190621/]
- 76. Using Genomics to Track Global Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC6737581/]
- 77. Rapid and precise alignment of raw reads against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6116485/]
- 78. Systematic Evaluation of Whole Genome Sequence-Based ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.00549/full]
- 79. Faster and Focused Searches with BLAST+ 2.15.0 [https://ncbiinsights.ncbi.nlm.nih.gov/2023/11/21/faster-focused-searches-blast-2-15/]
- 80. Simultaneous detection of pathogens and antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057172/]
- 81. Galaxy @Sciensano: a comprehensive bioinformatics portal ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-11182-5]
- 82. Benchmarking workflows to assess performance and ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-020-03934-3]
- 83. Whole Genome Sequencing (WGS) Quality Control (QC) ... [https://www.ga4gh.org/news_item/whole-genome-sequencing-wgs-quality-control-qc-standards-approved-as-an-official-ga4gh-product/]
- 84. A comprehensive benchmarking of WGS-based deletion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9294411/]
- 85. Validation of genetic variants from NGS data using deep ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05255-7]
- 86. Geno4ME Study: implementation of whole genome ... [https://www.nature.com/articles/s41525-025-00508-1]
- 87. Factors influencing success of clinical genome sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4601524/]
- 88. A Practical Guide to Clinical Variant Interpretation [https://www.euformatics.com/blog-post/a-practical-guide-to-clinical-variant-interpretation]
- 89. Protocol for the functional evaluation of genetic variants ... [https://www.sciencedirect.com/science/article/pii/S2666166725001169]
- 90. Exploiting biological priors and sequence variants enhances ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-016-2443-6]
- 91. BayesRC method [https://bio-protocol.org/exchange/minidetail?id=790540&type=30]
- 92. Leveraging functional genomic annotations and ... [https://www.nature.com/articles/s41588-024-01704-y]
- 93. Integrating multi-layered biological priors to improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11686921/]
- 94. GCTB [https://gctbhub.cloud.edu.au/software/gctb/]
- 95. Incorporating multiple functional annotations to improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12230236/]