Strategies for Managing False Positives in Screening Data: From Drug Discovery to Clinical Trials
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on addressing the pervasive challenge of false positives in scientific screening.
Strategies for Managing False Positives in Screening Data: From Drug Discovery to Clinical Trials
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on addressing the pervasive challenge of false positives in scientific screening. It explores the foundational impact of false positives from high-throughput drug screening (HTS) to clinical trial data analysis, outlines advanced methodological approaches for mitigation, offers practical troubleshooting and optimization strategies, and presents a framework for the validation and comparative analysis of screening methods. By synthesizing insights across the research pipeline, this resource aims to enhance data integrity, improve research efficiency, and accelerate the development of reliable therapeutic agents.
Understanding the Foundational Impact and Causes of False Positives in Research
A Researcher's Guide to Definitions and Impact
In screening data research, a false positive occurs when a test incorrectly indicates the presence of a specific condition or effect—such as a hit in a high-throughput screen—when it is not actually present. This is a Type I error, or a "false alarm" [1] [2]. Its counterpart, the false negative, occurs when a test fails to detect a condition that is truly present, incorrectly indicating its absence. This is a Type II error, meaning a real effect or "hit" was missed [1] [2].
The consequences of these errors are context-dependent and can significantly impact research validity and resource allocation. The table below summarizes these outcomes across different fields.
Table 1: Consequences of False Positives and False Negatives in Different Research Contexts
| Field/Context | Consequence of a False Positive | Consequence of a False Negative |
|---|---|---|
| Medical Diagnosis [2] [3] | Unnecessary treatment, patient anxiety, and wasted resources. | Failure to treat a real disease, leading to worsened patient health. |
| Drug Development [4] | Pursuit of an ineffective treatment, wasting significant R&D budget and time. | Elimination of a potentially effective treatment, missing a healthcare and economic opportunity. |
| Spam Detection [3] [5] | A legitimate email is sent to the spam folder, potentially causing important information to be missed. | A spam email appears in the inbox, causing minor inconvenience. |
| Fraud Detection [3] | A legitimate transaction is blocked, causing customer inconvenience. | A fraudulent transaction is approved, leading to direct financial loss. |
| Scientific Discovery [6] [7] | Literature is polluted with false findings, inspiring fruitless research programs and ineffective policies. A field can lose its credibility [7]. | A true discovery is missed, delaying scientific progress and understanding. |
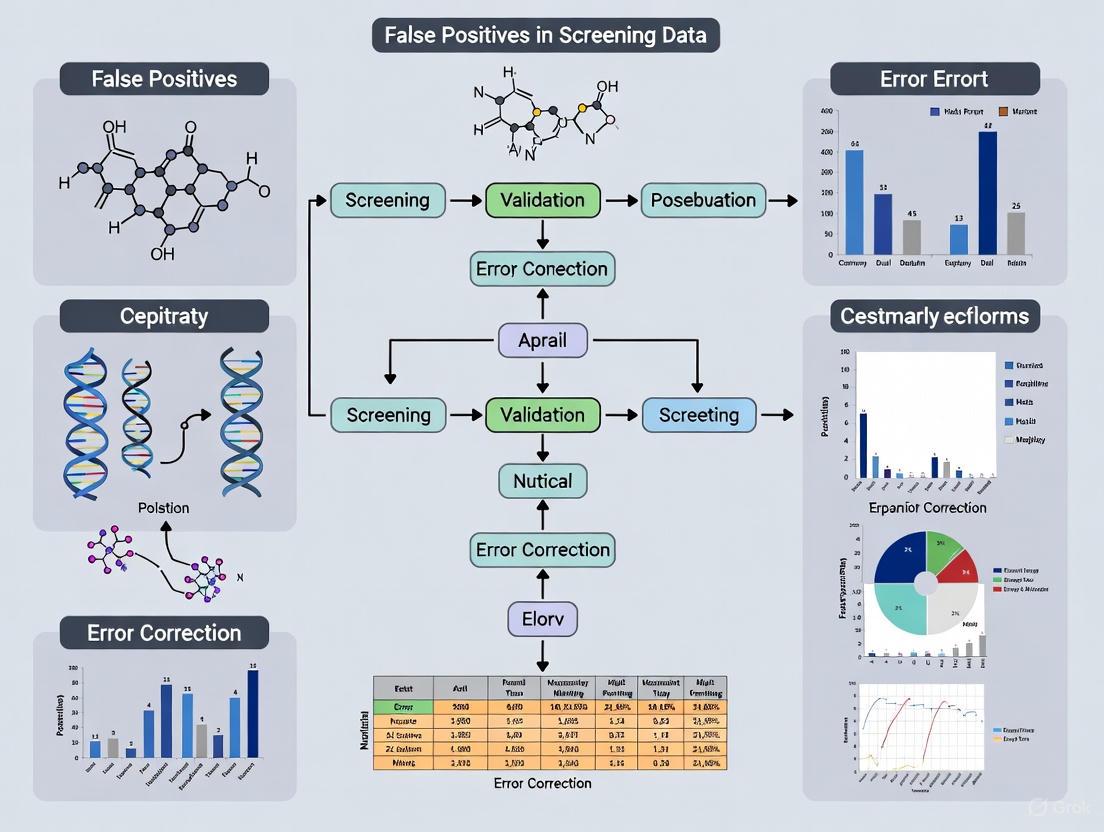
The following workflow illustrates the decision path in a binary test and where these errors occur.
Troubleshooting FAQs: Addressing False Positives and Negatives in the Lab
This section addresses common experimental challenges related to false positives and false negatives, offering practical solutions for researchers.
FAQ 1: My assay has no window at all. What should I check first? A complete lack of an assay window, where you cannot distinguish between positive and negative controls, often points to a fundamental setup issue [8].
- Primary Checks:
- Instrument Configuration: Verify that your microplate reader or other instrument is set up correctly. The most common reason for a TR-FRET assay to fail, for instance, is the use of incorrect emission filters. Always use the manufacturer-recommended filters for your specific instrument [8].
- Reagent Integrity: Check the expiration dates and storage conditions of all reagents. Improperly stored or old reagents may have degraded.
- Control Functionality: Ensure your positive and negative controls are working as expected. If controls are not behaving predictively, the problem may lie with the control preparations rather than the experimental samples.
FAQ 2: My assay window is small and noisy. How can I improve its robustness? A small or variable assay window increases the risk of both false positives and false negatives by making it difficult to reliably distinguish a true signal.
- Solution: Evaluate your assay using the Z'-factor, a statistical metric that assesses the quality and robustness of a high-throughput screen by considering both the dynamic range (the assay window) and the data variation [8].
- The formula is: Z' = 1 - [ (3σpositive + 3σnegative) / |μpositive - μnegative| ]
- Here, σ is the standard deviation and μ is the mean of the positive and negative controls.
- A Z'-factor > 0.5 is considered an excellent assay suitable for screening. A small window with high noise (large standard deviation) will yield a low Z'-factor, indicating the assay needs optimization before proceeding [8].
FAQ 3: Why are my IC₅₀/EC₅₀ values inconsistent between labs or experiments? Differences in calculated potency values like IC₅₀ often stem from variations in sample preparation rather than the assay itself [8].
- Troubleshooting Steps:
- Stock Solution Integrity: This is the primary reason for differences. Ensure the concentration, purity, and solvent composition of your compound stock solutions are accurate and consistent. Use freshly prepared stocks where possible [8].
- Protocol Adherence: Strictly standardize all procedural steps, including incubation times, temperatures, and reagent addition order.
- Data Normalization: Use ratiometric data analysis for assays like TR-FRET. Dividing the acceptor signal by the donor signal (e.g., 665 nm/615 nm for Europium) accounts for pipetting variances and minor lot-to-lot reagent variability, leading to more reproducible results [8].
FAQ 4: How can I reduce false positives in my statistical analysis? False positives in data analysis can arise from "researcher degrees of freedom"—undisclosed flexibility in how data is collected and analyzed [7].
- Corrective Measures:
- Pre-register Analysis Plans: Decide your data collection termination rule and primary analysis method before you begin collecting data [7].
- Report All Measures and Conditions: List all variables collected and all experimental conditions run, including any failed manipulations [7].
- Use Appropriate Power: Underpowered studies are a major source of unreliable results. Conduct power analysis to ensure your sample size is large enough to detect a true effect. One simulation in drug development showed that increasing Phase II trial power from 50% to 80% could increase productivity by over 60% by reducing false negatives [4].
Experimental Protocols for Error Mitigation
Protocol 1: Validating Assay Performance with Z'-Factor Calculation
This protocol provides a step-by-step method to quantitatively assess the robustness of a screening assay, helping to prevent both false positives and negatives caused by a poor assay system [8].
- Plate Setup: On a microplate, designate a minimum of 16 wells for the positive control and 16 wells for the negative control.
- Assay Execution: Run the assay according to your standard procedure on the entire plate.
- Data Collection: Measure the raw signal (e.g., RFU) for all control wells.
- Calculation:
- Calculate the mean (μ) and standard deviation (σ) for the positive control and the negative control.
- Apply the values to the Z'-factor formula: Z' = 1 - [ (3σpositive + 3σnegative) / |μpositive - μnegative| ]
- Interpretation:
- Z' ≥ 0.5: The assay is robust and suitable for screening.
- 0 < Z' < 0.5: The assay is marginal and may require optimization.
- Z' ≤ 0: The assay is not viable and cannot distinguish between controls.
Protocol 2: A Bayesian Framework for Interpreting "Significant" p-values
This methodological approach helps contextualize a statistically significant result to estimate the risk that it is a false positive, which is particularly high for novel or surprising findings [6].
- Define Prior Odds: Before the experiment, estimate the prior probability that your hypothesis is true, based on existing literature and scientific plausibility. For novel, paradigm-shifting hypotheses, this probability may be low [6].
- Conduct the Experiment: Perform your study and note the resulting p-value.
- Calculate the False Positive Risk (FPR): Use statistical methods (e.g., as proposed by Colquhoun, 2017) to calculate the probability that a significant finding is actually a false positive [1]. This FPR is always higher than the observed p-value.
- Interpretation: A p-value of 0.05 does not mean a 5% chance of a false positive. The actual risk could be much higher (e.g., 20-50%) depending on the prior odds. This framework emphasizes the need for replication and cautious interpretation of single studies, especially for novel findings published in high-impact journals [1] [6].
The Scientist's Toolkit: Key Reagent Solutions
The following table details essential materials and their functions in managing assay quality.
Table 2: Key Research Reagents and Materials for Quality Control
| Item/Reagent | Function in Managing False Positives/Negatives |
|---|---|
| TR-FRET Donor & Acceptor (e.g., Tb or Eu cryptate) | Forms the basis of a homogeneous, ratiometric assay. Using the recommended donor/acceptor pair with correct filters minimizes background noise and improves signal specificity, reducing error-prone signals [8]. |
| Validated Positive & Negative Controls | Critical for calculating the Z'-factor and validating every assay run. A well-characterized control set ensures the assay is functioning properly and can detect true effects. |
| Standardized Compound Libraries | Using compounds with verified purity and concentration in screening reduces false positives stemming from compound toxicity, aggregation, or degradation. |
| High-Quality Assay Plates | Optically clear, non-binding plates ensure consistent signal detection and prevent compound absorption, which can lead to inaccurate concentration-response data and both false positives and negatives. |
Visualization: The Precision-Recall Trade-Off
In machine learning and statistical classification, a key challenge is the inherent trade-off between false positives and false negatives, which is managed by adjusting the classification threshold. This relationship is captured by the metrics of precision and recall. The following diagram illustrates how changing the threshold to reduce one type of error inevitably increases the other.
In the high-stakes world of drug development, false positives represent a critical and costly challenge. A false positive occurs when an assay or screening method incorrectly identifies an inactive compound as a potential hit [9]. These misleading signals can derail research trajectories, consume invaluable resources, and ultimately skew the entire development pipeline. The impact cascades from early discovery through clinical trials, with studies indicating that a significant majority of phase III oncology clinical trials in the past decade have been negative for overall survival benefit, in part due to ineffective therapies advancing from earlier stages [10]. Understanding, quantifying, and mitigating false positives is therefore not merely a technical exercise but a fundamental requirement for research integrity and efficiency.
Quantifying the Impact: The Multifaceted Cost of False Positives
The cost of false positives extends far beyond simple reagent waste. It encompasses direct financial losses, massive time delays, and the opportunity cost of pursuing dead-end leads.
Financial and Resource Drain
False positives impose a significant financial burden on the drug development process, which already costs an estimated $1-2.5 billion and takes 10-15 years to bring a new drug to market [9]. The table below summarizes the key areas of impact.
Table 1: Quantitative Impact of False Positives in Drug Development
| Area of Impact | Quantitative / Qualitative Effect | Context / Source |
|---|---|---|
| High-Throughput Screening (HTS) | Can derail entire HTS campaigns [11]. | A single HTS campaign can screen 250,000+ compounds. |
| Hit Rate Inflation | Artificially inflates hit rates, forcing re-screening and validation [11]. | Increases follow-up workload and costs. |
| Phase III Trial Failure | 87% of phase III oncology trials negative for OS benefit [10]. | Suggests many ineffective therapies advance to late-stage testing. |
| Clinical Trial False Positives | 58.4% false-positive OS rate when P=.05 is used [10]. | Based on analysis of 362 phase III superiority trials. |
The Ripple Effect on Workflow and Efficiency
The consequences of false positives create a ripple effect that impedes operational efficiency:
- Resource Misallocation: Teams spend weeks on secondary screening and validation of false leads, which can mean "hundreds of wasted follow-ups and delayed projects" [11].
- Distorted Structure-Activity Relationships (SAR): False positives can obscure genuine SAR, complicating the critical lead optimization process [11].
- Increased Attrition: The high failure rate of phase III trials, fueled in part by false advances from earlier stages, represents the ultimate resource drain, exposing patients to therapies with insufficient efficacy and consuming development costs that could have been allocated to more promising candidates [10].
Guide: Minimizing False Positives in ADP-Detection Assays
Problem: High false positive rates in assays measuring kinase, ATPase, or other ATP-dependent enzyme activity are skewing screening results and wasting resources.
Background: These assays are a universal readout for enzymes that consume ATP. Many traditional formats, particularly coupled enzyme assays, use secondary enzymes (like luciferase) to generate a signal. Test compounds can inhibit or interfere with these coupling enzymes rather than the target enzyme, producing a false-positive signal [11].
Solution: Implement a direct detection method.
- Step 1: Evaluate Your Current Assay Format. Compare your method against the following table to identify potential vulnerability to false positives.
Table 2: Comparison of ADP Detection Assay Formats and False Positive Sources
| Assay Type | Detection Mechanism | Typical Sources of False Positives |
|---|---|---|
| Coupled Enzyme Assays | Uses enzymes to convert ADP to ATP, driving a luminescent reaction. | Compounds that inhibit coupling enzymes, generate ATP-like signals, or quench luminescence. |
| Colorimetric (e.g., Malachite Green) | Detects inorganic phosphate released from ATP. | Compounds absorbing at the detection wavelength; interference from phosphate buffers. |
| Direct Fluorescent Immunoassays | Directly detects ADP via antibody-based tracer displacement. | Very low – direct detection of the product itself minimizes interference points. |
- Step 2: Transition to a Direct Detection Platform. Replace indirect, coupled assays with a direct method like the Transcreener ADP² Assay, which uses competitive immunodetection to measure ADP production without secondary enzymes [11].
- Step 3: Optimize Assay Parameters. Ensure the assay supports a wide ATP concentration range (e.g., 0.1 µM to 1 mM) to maintain physiological relevance and broad enzyme compatibility [11].
- Step 4: Validate with Controls. Use robust controls to confirm the assay's specificity, accuracy, precision, and limits of detection as part of a rigorous validation protocol [9].
The following workflow contrasts the problematic indirect method with the recommended direct detection approach:
Guide: Addressing False Positives in Mass Spectrometry-Based Screening
Problem: Even advanced, direct detection methods like mass spectrometry (MS) can be plagued by novel false-positive mechanisms that consume time and resources to resolve [12].
Background: MS is valued for its direct nature, which avoids common artifacts like fluorescence interference and eliminates the need for coupling enzymes. However, unexplained false positives still occur.
Solution: Develop a dedicated pipeline to identify and filter these specific false positives.
- Step 1: Acknowledge the Possibility. Recognize that no HTS method is completely immune to false positives, and investigate hits from MS screens with a critical eye.
- Step 2: Develop a Counter-Screen. Create a secondary assay designed specifically to test for the newly identified mechanism of interference. The nature of this counter-screen will depend on the specific false-positive mechanism discovered in your system [12].
- Step 3: Implement a Triaging Pipeline. Integrate this counter-screen into your primary screening workflow to automatically flag and eliminate these classes of false hits before they advance to more resource-intensive validation stages [12].
Key Reagents and Technologies for False Positive Mitigation
The following toolkit details essential solutions that can enhance the accuracy of your screening campaigns.
Table 3: Research Reagent Solutions for Minimizing False Positives
| Solution / Technology | Function | Key Benefit for False Positive Reduction |
|---|---|---|
| Transcreener ADP² Assay | Direct, antibody-based immunodetection of ADP. | Eliminates coupling enzymes, a major source of compound interference [11]. |
| Microfluidic Devices & Biosensors | Creates controlled environments for cell-based assays and monitors analytes with high sensitivity. | Mimics physiological conditions for more relevant data; reduces assay variability [9]. |
| Automated Liquid Handlers (e.g., I.DOT) | Provides precise, non-contact liquid dispensing for assay miniaturization and setup. | Enhances assay precision and consistency, minimizing human error and technical variability [9]. |
| AI & Machine Learning Platforms | Predictive modeling for hit identification and experimental design. | Accelerates hit ID and helps design assays that are less prone to interference [9]. |
| Design of Experiments (DoE) | A systematic approach to optimizing assay parameters and conditions. | Reduces experimental variation and identifies robust assay conditions that improve signal-to-noise [9]. |
Frequently Asked Questions (FAQs)
Q1: What are the most common causes of false positives in high-throughput drug screening? False positives typically arise from compound interference with the detection system. In coupled assays, this means inhibiting secondary enzymes like luciferase. Other common causes include optical interference (e.g., compound fluorescence or quenching), non-specific compound interactions with assay components, and aggregation-based artifacts [11] [9].
Q2: How can I convince my lab to invest in a new, more specific assay platform given budget constraints? Frame the decision in terms of total cost of ownership. While a direct detection assay might have a higher per-well reagent cost, it drastically reduces the false positive rate. This translates to significant savings by avoiding weeks of wasted labor on validating false leads, reducing reagent consumption for follow-up assays, and accelerating project timelines. One analysis showed that switching to a direct detection method could reduce false leads in a 250,000-compound screen from 3,750 to roughly 250—a 15x improvement [11].
Q3: Are there statistical approaches to reduce false positives in later-stage clinical trials? Yes. Research into phase III oncology trials has explored using more stringent statistical thresholds, such as lowering the P value from .05 to .005, which was shown to reduce the false-positive rate from 58.4% to 34.7%. However, this also increases the false-negative rate. A flexible, risk-based model is often recommended, where stringency is higher in crowded therapeutic areas and more relaxed in areas of high unmet need, like some orphan diseases [10].
Q4: We use mass spectrometry, which is a direct method. Why are we still seeing false positives? Mass spectrometry, while direct and less prone to common artifacts, is not infallible. Novel mechanisms for false positives that are unique to MS-based screening can and do occur. The solution is to develop a specific pipeline for detecting these unusual false positives, which may involve creating a custom counter-screen to identify and filter them out from your true hits [12].
Q5: How does assay validation help prevent false positives? A robust assay validation process is your first line of defense. By thoroughly testing and documenting an assay's specificity, accuracy, precision, and robustness before it's used for screening, you can identify and correct vulnerabilities that lead to false positives. This includes testing for susceptibility to interference from common compound library artifacts [9].
Frequently Asked Questions (FAQs)
1. What is root cause analysis (RCA) in the context of screening data research? Root cause analysis is a systematic methodology used to identify the underlying, fundamental reason for a problem, rather than just addressing its symptoms. In screening data research, this is crucial for distinguishing true positive results from false positives, which can be caused by technical artifacts, data quality issues, or methodological errors. The goal is to implement corrective actions that prevent recurrence and improve data reliability [13].
2. Our team is new to RCA. What is a simple method we can use to start an investigation? The Five Whys technique is an excellent starting point. It involves repeatedly asking "why" (typically five times) to peel back layers of symptoms and reach a root cause. For example:
- Why was the assay result a potential false positive? Because the signal was anomalously high.
- Why was the signal anomalously high? Because the positive control was contaminated.
- Why was the positive control contaminated? Because the vial was used without proper aspiration technique.
- Why was the improper technique used? Because the training on the new liquid handler was incomplete.
- Why was the training incomplete? Because the training protocol was not updated to include the new equipment. The root cause is an outdated training protocol, not the individual user's mistake [13].
3. We are seeing a high rate of inconclusive results. How can we prioritize which potential cause to investigate first? A Pareto Chart is a powerful tool for prioritization. It visually represents the 80/20 rule, suggesting that 80% of problems often stem from 20% of the causes. By categorizing your inconclusive results (e.g., "low signal-to-noise," "precipitate formation," "edge effect," "pipetting error") and plotting their frequency, you can immediately identify the most significant category. Your team should then focus its RCA efforts on that top contributor first [13].
4. Our media fill simulations for an aseptic process are failing, but our investigation found no issues with our equipment or technique. What could be the source of contamination? As a documented case from the FDA highlights, the source may not be your process but your materials. In one instance, multiple media fill failures were traced to the culture media itself, which was contaminated with Acholeplasma laidlawii. This organism is small enough (0.2-0.3 microns) to pass through a standard 0.2-micron sterilizing filter. The resolution was to filter the media through a 0.1-micron filter or to use pre-sterilized, irradiated media [14].
5. How can we proactively identify potential failure points in a new screening assay before we run it? Failure Mode and Effects Analysis (FMEA) is a proactive RCA tool. Your team brainstorms all potential things that could go wrong (failure modes) in the assay workflow. For each, you assess the Severity (S), Probability of Occurrence (O), and Probability of Detection (D) on a scale (e.g., 1-10). Multiplying S x O x D gives a Risk Priority Number (RPN). This quantitative data allows you to prioritize and address the highest-risk failure modes before they cause false positives or other data integrity issues [13].
Troubleshooting Guides
Problem: Inconsistent Replicates and High Well-to-Well Variability
| Step | Action | Rationale & Details |
|---|---|---|
| 1 | Verify Liquid Handler Performance | Check calibration of pipettes, especially for small volumes. Ensure tips are seated properly and are compatible with the plates being used. Look for drips or splashes. |
| 2 | Inspect Reagent Homogeneity | Ensure all reagents, buffers, and cell suspensions are thoroughly mixed before dispensing. Vortex or pipette-mix as required. |
| 3 | Check for Edge Effects | Review plate maps for patterns related to plate location. Evaporation in edge wells can cause artifacts. Use a lid or a plate sealer, and consider using a humidified incubator. |
| 4 | Confirm Cell Health & Seeding Density | Use a viability stain to confirm cell health. Use a microscope to check for consistent monolayer or clumping. Re-count cells to ensure accurate seeding density across wells. |
| 5 | Analyze with a Fishbone Diagram | If the cause remains elusive, conduct a team brainstorming session using a Fishbone Diagram. Use the 6M categories (Methods, Machine, Manpower, Material, Measurement, Mother Nature) to identify all potential sources of variation [13]. |
Problem: Systematic False Positive Signals in a High-Throughput Screen
| Step | Action | Rationale & Details |
|---|---|---|
| 1 | Interrogate Compound/Reagent Integrity | Check for compound precipitation, which can cause light scattering or non-specific binding. Review chemical structures for known promiscuous motifs (e.g., pan-assay interference compounds, or PAINS). Confirm reagent stability and storage conditions. |
| 2 | Analyze Plate & Signal Patterns | Create a scatter plot of all well signals against their plate location. Look for systematic trends (e.g., gradients) indicating a temperature, dispense, or reader issue. Perform a Z'-factor analysis to reassay the robustness of the screen itself [13]. |
| 3 | Investigate Instrumentation | Check the spectrophotometer, fluorometer, or luminometer for calibration errors, dirty optics, or lamp degradation. Run system suitability tests with standard curves. |
| 4 | Employ Orthogonal Assays | Confirm any "hit" from a primary screen using a different, non-correlated assay technology (e.g., confirm a fluorescence readout with a luminescence or SPR-based assay). This helps rule out technology-specific artifacts. |
| 5 | Apply Fault Tree Analysis | For complex failures, use Fault Tree Analysis. This Boolean logic-based method helps model specific combinations of events (e.g., "Compound is fluorescent" AND "assay uses fluorescence polarization") that lead to the false positive outcome, helping to pinpoint the precise failure pathway [13]. |
Methodology and Data Visualization
Root Cause Analysis Methodologies for Research
The table below summarizes key RCA tools, their primary application, and a quantitative assessment of their ease of use and data requirements to help you select the right tool.
| Methodology | Primary Use Case | Ease of Use (1-5) | Data Requirement |
|---|---|---|---|
| Five Whys | Simple, linear problems with human factors [13]. | 5 (Very Easy) | Low (Expert Knowledge) |
| Pareto Chart | Prioritizing multiple competing problems based on frequency [13]. | 4 (Easy) | High (Quantitative Data) |
| Fishbone Diagram | Brainstorming all potential causes in a structured way during a team session [13]. | 4 (Easy) | Medium (Team Input) |
| Fault Tree Analysis | Complex failures with multiple, simultaneous contributing factors; uses Boolean logic [13]. | 2 (Complex) | High (Quantitative & Logic) |
| Failure Mode & Effects Analysis (FMEA) | Proactively identifying and mitigating risks in a new process or assay [13]. | 3 (Moderate) | High (Structured Analysis) |
| Scatter Plot | Visually investigating a hypothesized cause-and-effect relationship between two variables [13]. | 3 (Moderate) | High (Paired Numerical Data) |
Experimental Protocol: Conducting a Five Whys Analysis
- Assemble a Team: Gather individuals with direct knowledge of the process and problem.
- Define the Problem: Write a clear, specific problem statement.
- Ask "Why?" Starting with the problem statement, ask why it happened.
- Record the Answer: Document the answer from the team's consensus.
- Iterate: Use the answer as the basis for the next "why?" Repeat this process until the team agrees the root cause is identified (this may be at the fifth why or a different number).
- Identify and Implement Countermeasures: Develop actions to address the root cause.
Logical Workflow for Root Cause Analysis
The following diagram illustrates the logical decision process for selecting and applying RCA methodologies to a data quality issue.
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function in Screening & RCA |
|---|---|
| 0.1-micron Sterilizing Filter | Used to prepare media or solutions when contamination by small organisms like Acholeplasma laidlawii is suspected, as it can penetrate standard 0.2-micron filters [14]. |
| Z'-Factor Assay Controls | A statistical measure used to assess the robustness and quality of a high-throughput screen. It uses positive and negative controls to quantify the assay window and signal dynamic range, helping to identify assays prone to variability and false results. |
| Orthogonal Assay Reagents | A different assay technology (e.g., luminescence vs. fluorescence) used to confirm hits from a primary screen. This is critical for ruling out technology-specific artifacts that cause false positives. |
| Pan-Assay Interference Compound (PAINS) Filters | Computational or library filters used to identify compounds with chemical structures known to cause false positives through non-specific mechanisms in many assay types. |
| Stable Cell Lines with Reporter Genes | Engineered cells that provide a consistent and specific readout (e.g., luciferase, GFP) for a biological pathway, reducing variability and artifact noise compared to transiently transfected systems. |
Technical Support Center
Troubleshooting Guides & FAQs
This technical support center addresses common challenges researchers face when handling missing data in clinical trials, with a focus on mitigating false-positive findings.
FAQ 1: Why can common methods like LOCF increase the risk of false-positive results? Answer: Simple single imputation methods, such as Last Observation Carried Forward (LOCF), assume that a participant's outcome remains unchanged after dropping out (data are Missing Completely at Random). However, this assumption is often false. When data are actually Missing at Random (MAR) or Missing Not at Random (MNAR), these methods can create an artificial treatment effect, thereby inflating the false-positive rate (Type I error) [15] [16] [17]. Simulation studies have shown that LOCF and Baseline Observation Carried Forward (BOCF) can lead to an inflated rate of false-positive results (Regulatory Risk Error) compared to more advanced methods [15] [17].
FAQ 2: What are the most reliable primary analysis methods for controlling false positives? Answer: For the primary analysis, Mixed Models for Repeated Measures (MMRM) and Multiple Imputation (MI) are generally recommended over simpler methods [15] [16] [18]. These methods assume data are Missing at Random (MAR), which is a more plausible assumption than MCAR in many trial settings. They use all available data from participants and provide more robust control of false-positive rates [15] [17]. The table below summarizes the performance of different methods based on simulation studies.
Table 1: Comparison of Statistical Methods for Handling Missing Data
| Method | Key Assumption | Impact on False-Positive Rate | Key Simulation Findings |
|---|---|---|---|
| Last Observation Carried Forward (LOCF) | Missing Completely at Random (MCAR) | Can inflate false-positive rates [15] | Inflated Regulatory Risk Error in 8 of 32 simulated MNAR scenarios [15] |
| Baseline Observation Carried Forward (BOCF) | Missing Completely at Random (MCAR) | Can inflate false-positive rates [15] | Inflated Regulatory Risk Error in 12 of 32 simulated MNAR scenarios [15] |
| Multiple Imputation (MI) | Missing at Random (MAR) | Better controls false-positive rates [15] [18] | Inflated rate in 3 of 32 MNAR scenarios [15]; Low bias & high power for MAR [18] |
| Mixed Model for Repeated Measures (MMRM) | Missing at Random (MAR) | Better controls false-positive rates [15] [18] | Inflated rate in 4 of 32 MNAR scenarios [15]; Least biased method in PRO simulation [18] |
| Pattern Mixture Models (PPM) | Missing Not at Random (MNAR) | Conservative for sensitivity analysis [18] | Superior for MNAR data; provides conservative estimate of treatment effect [18] |
FAQ 3: How should we handle missing data that is "Missing Not at Random" (MNAR)? Answer: For data suspected to be MNAR, where the reason for missingness is related to the unobserved outcome itself, sensitivity analyses are crucial. Control-based Pattern Mixture Models (PMMs), such as Jump-to-Reference (J2R) and Copy Reference (CR), are recommended [16] [18]. These methods provide a conservative estimate by assuming that participants who dropped out from the treatment group will have a similar response to those in the control group after dropout. This helps assess the robustness of the primary trial results under a "worst-case" MNAR scenario [18].
FAQ 4: What is the single most important step to reduce the impact of missing data? Answer: The most effective strategy is prevention during the trial design and conduct phase [19]. Proactive measures significantly reduce the amount and potential bias of missing data. Key tactics include:
- Implementing robust patient retention strategies [19] [16].
- Applying Quality-by-Design (QbD) principles to identify and mitigate risks to data quality early in the planning process [20].
- Using effective centralized monitoring tools, like well-designed Key Risk Indicators (KRIs), to detect site-level issues (e.g., rising dropout rates) early [20].
Experimental Protocols
Protocol: Implementing a Multiple Imputation (MI) Analysis with Predictive Mean Matching
This protocol outlines the steps for using MI, a robust method for handling missing data under the MAR assumption, to reduce bias and control false-positive rates.
1. Imputation Phase:
- Objective: Create multiple complete datasets by replacing missing values with plausible estimates.
- Procedure:
a. Use a statistical procedure (e.g.,
PROC MIin SAS) to generatemcomplete datasets. Rubin's framework suggests 3-5 imputations, but more (e.g., 20-100) are common for better stability [16]. b. Specify an imputation model that includes the outcome variable, treatment group, time, baseline covariates, and any variables predictive of missingness. c. For continuous outcomes, use the Predictive Mean Matching (PMM) method. PMM imputes a missing value by sampling fromkobserved data points with the closest predicted values, preserving the original data distribution and reducing bias [16].
2. Analysis Phase:
- Objective: Analyze each of the
mimputed datasets separately. - Procedure:
a. Perform the planned primary analysis (e.g., ANCOVA model for the primary endpoint) on each of the
mcompleted datasets. b. From each analysis, save the parameter estimates (e.g., treatment effect) and their standard errors.
3. Pooling Phase:
- Objective: Combine the results from the
manalyses into a single set of estimates. - Procedure:
a. Calculate the final point estimate by averaging the
mtreatment effect estimates. b. Calculate the combined standard error using Rubin's Rules, which incorporates the average within-imputation variance (W) and the between-imputation variance (B) to account for the uncertainty of the imputations [16]. c. Use the combined estimates to calculate confidence intervals and p-values.
The following workflow diagram illustrates the entire MI process.
The Scientist's Toolkit: Research Reagent Solutions
This table details key methodological "reagents" essential for designing and analyzing clinical trials with a low risk of false positives due to missing data.
Table 2: Essential Materials for Handling Missing Data
| Tool / Solution | Function & Purpose |
|---|---|
| Mixed Models for Repeated Measures (MMRM) | A model-based analysis method that uses all available longitudinal data points under the MAR assumption without requiring imputation. It is often the preferred primary analysis for continuous endpoints [15] [18]. |
| Multiple Imputation (MI) Software (e.g., PROC MI) | A statistical procedure used to generate multiple plausible versions of a dataset with missing values imputed. It accounts for the uncertainty of the imputation process, leading to more valid statistical inferences [16]. |
| Pattern Mixture Models (PMMs) | A class of models used for sensitivity analysis to test the robustness of results under MNAR assumptions. Variants like "Jump-to-Reference" (J2R) are considered conservative and are valued by regulators [16] [18]. |
| Key Risk Indicators (KRIs) | Proactive monitoring tools (e.g., site-level dropout rates, data entry lag times) used during trial conduct to identify operational issues that could lead to problematic missing data, allowing for timely intervention [20]. |
| Statistical Analysis Plan (SAP) | A pre-specified document that definitively states the primary method for handling missing data and the plan for sensitivity analyses. This prevents data-driven selection of methods and protects trial integrity [16] [21]. |
Advanced Methodologies to Minimize False Positives in Data Screening
Understanding LOCF, BOCF, and False Positives
In drug development, the primary analysis often relies on specific methods to handle missing data. Two traditional approaches are Last Observation Carried Forward (LOCF) and Baseline Observation Carried Forward (BOCF). These methods work by substituting missing values; LOCF replaces missing data with a subject's last available measurement, while BOCF uses the baseline value.
A false positive in this context occurs when a study incorrectly concludes that a drug is more effective than the control, when in reality it is not. This is also known as a Regulatory Risk Error (RRE). The core of the problem is that LOCF and BOCF are based on a restrictive assumption that data are Missing Completely at Random (MCAR) [15].
Modern methods like Multiple Imputation (MI) and Likelihood-based Repeated Measures (MMRM) are less restrictive, as they assume data are Missing at Random (MAR). When data are actually Missing Not at Random (MNAR), the use of LOCF and BOCF can inflate the rate of false positives, increasing regulatory risks compared to MI and MMRM [15].
The table below summarizes a simulation study comparing the false-positive rates of these methods [15].
| Method | Underlying Assumption | Scenarios with Inflated False-Positive Rates (out of 32) | Key Finding |
|---|---|---|---|
| BOCF | Missing Completely at Random (MCAR) | 12 | Inflates regulatory risk; no scenario provided adequate control where modern methods failed. |
| LOCF | Missing Completely at Random (MCAR) | 8 | Inflates regulatory risk; no scenario provided adequate control where modern methods failed. |
| Multiple Imputation (MI) | Missing at Random (MAR) | 3 | Better choice for primary analysis; superior control of false positives. |
| MMRM | Missing at Random (MAR) | 4 | Better choice for primary analysis; superior control of false positives. |
A Practical Experimental Protocol for Method Comparison
To empirically validate the performance of different methods for handling missing data, you can implement the following experimental workflow. This protocol is based on simulation studies that have identified the shortcomings of legacy methods [15].
Objective: To compare the rate of false-positive results (Regulatory Risk Error) generated by BOCF, LOCF, MI, and MMRM under a controlled Missing Not at Random (MNAR) condition.
Materials & Software: Statistical software (e.g., R, SAS, Python), predefined clinical trial simulation model.
Procedure:
- Dataset Generation: Simulate a complete, primary clinical trial dataset for a drug versus control study. The true treatment effect should be defined as zero to allow for false-positive detection [15].
- Induce Missing Data: Systematically remove a portion of the post-baseline data from the simulated dataset using an MNAR mechanism. This means the probability of data being missing is related to the unobserved outcome itself [15].
- Apply Methods: Analyze the resulting incomplete dataset using four different methods:
- Baseline Observation Carried Forward (BOCF)
- Last Observation Carried Forward (LOCF)
- Multiple Imputation (MI)
- Mixed-Model Repeated Measures (MMRM)
- Record Outcome: For each method, record the statistical conclusion regarding the drug's efficacy. A false positive is recorded if the method incorrectly indicates a statistically significant benefit for the drug (p < 0.05).
- Replicate and Calculate: Repeat steps 1-4 a large number of times (e.g., 10,000 iterations) for the same MNAR scenario. The false-positive rate (RRE) for each method is calculated as the percentage of iterations that yielded a false positive.
- Compare: Compare the calculated RRE of BOCF and LOCF against the RRE of MI and MMRM. An inflated RRE indicates a higher risk of false positives.
Expected Outcome: This experiment will typically show that BOCF and LOCF produce a higher false-positive rate (RRE) compared to MI and MMRM when data are missing not at random [15].
The Scientist's Toolkit: Essential Research Reagent Solutions
When designing experiments and analyzing data to mitigate false positives, having the right "reagents" — whether computational or statistical — is crucial. The following table details key solutions for your research.
| Tool / Method | Type | Primary Function | Role in Addressing False Positives |
|---|---|---|---|
| Multiple Imputation (MI) | Statistical Method | Handles missing data by creating several complete datasets and pooling results. | Reduces bias from missing data; less likely than LOCF/BOCF to inflate false positives under MAR/MNAR [15]. |
| Mixed-Model Repeated Measures (MMRM) | Statistical Model | Analyzes longitudinal data with correlated measurements without imputing missing values. | Provides a robust, likelihood-based approach that better controls false-positive rates [15]. |
| Risk-Based Quality Management (RBQM) | Framework | Shifts focus from 100% data verification to centralized monitoring of critical data points. | Improves overall data quality and enables proactive issue detection, indirectly reducing factors that contribute to spurious findings [22]. |
| Homogenous Time Resolved Fluorescence (HTRF) | Assay Technology | A biochemical assay used to study molecular interactions. | Includes built-in counter-screens (e.g., time-zero addition, dual-wavelength assessment) to identify compound interference, a common source of false hits in screening [23]. |
Frequently Asked Questions (FAQs)
1. Why do LOCF and BOCF remain popular if they inflate false-positive rates? There is a persistent perception that the inherent bias in LOCF and BOCF is conservative and protects against falsely claiming a drug is effective. However, simulation studies have proven this false. These methods can create an illusion of stability and inflate the apparent effect size, leading to a higher chance of a false positive claim of efficacy [15].
2. What is the key difference between the MCAR and MAR assumptions? MCAR (Missing Completely at Random): The probability that data is missing is unrelated to both the observed and unobserved data. It is a completely random event. This is the unrealistic assumption underlying LOCF and BOCF. MAR (Missing at Random): The probability that data is missing may depend on observed data (e.g., a subject with worse baseline symptoms may be more likely to drop out), but not on the unobserved data. This is the more plausible assumption for MI and MMRM [15].
3. My clinical trial has a low rate of missing data. Is it safe to use LOCF? No. Even with a low amount of missing data, using an inappropriate method can bias the results. The risk is not solely about the quantity of missing data, but about the nature of the missingness mechanism. Modern methods like MMRM are superior even with small amounts of missing data and should be considered the primary analysis for regulatory submission [15].
4. Beyond false positives, what other risks do legacy methods pose? Using legacy methods can lead to inefficient use of resources. Furthermore, as the industry moves towards risk-based approaches and clinical data science, reliance on outdated methods like LOCF and BOCF can hinder innovation, slow down database locks, and ultimately delay a drug's time to market [22].
5. Our team is familiar with LOCF. How can we transition to modern methods? Transitioning requires both a shift in mindset and skill development. Start by:
- Education: Discuss published comparative studies (like the one cited here) with your team.
- Upskilling: Invest in training for statisticians and data scientists on MI and MMRM implementation.
- Pilot Testing: Apply modern methods in parallel with legacy methods on completed studies to build internal comfort and demonstrate their impact.
- Consultation: Engage with regulatory statisticians early to gain alignment on using MI or MMRM as the pre-specified primary analysis [22].
Troubleshooting Guides
MMRM Convergence Issues
Problem: My Mixed Model for Repeated Measures (MMRM) fails to converge or produces unreliable estimates.
Solution:
- Check Covariance Structure: Ensure you've selected an appropriate covariance structure (unstructured, compound symmetry, autoregressive). Unstructured covariance is most flexible but requires more parameters. Start with simpler structures if you have convergence issues. [24]
- Verify Time-by-Covariate Interactions: Always include time-by-covariate interactions in your MMRM specification. Omitting these interactions can reduce power and robustness against dropout bias. [25]
- Inspect Starting Values: Poor starting values can prevent convergence. Use method of moments estimates or simplified model results as starting values.
- Increase Iterations: For complex models with many parameters, increase the maximum number of iterations in your estimation algorithm.
Multiple Imputation Compatibility Problems
Problem: After using multiple imputation, my analysis results seem inconsistent or implausible.
Solution:
- Check Imputation Level Strategy: For multi-item instruments, decide whether to impute at the item-level or score-level. Empirical evidence shows item-level imputation may yield different results than score-level imputation. [26]
- Verify Included Variables: Include all analysis variables in the imputation model, including outcome and auxiliary variables that may predict missingness. Omission can introduce bias. [27]
- Assess Imputation Number: Use sufficient number of imputations. While 3-5 was historically common, modern recommendations suggest 20-100 imputations depending on the percentage of missing data. [28]
- Examine Pooling Results: Ensure proper pooling of estimates using Rubin's rules. Software should automatically combine parameter estimates and standard errors across imputed datasets. [16]
False Positive Control in Screening Data
Problem: My screening data analysis produces unexpectedly high false positive rates.
Solution:
- Adjust for Multiple Comparisons: When running multiple statistical tests, implement correction methods like Bonferroni or Benjamini-Hochberg False Discovery Rate control. Uncorrected testing dramatically increases false positives. [29]
- Validate Missing Data Mechanisms: Conduct sensitivity analyses to test whether missingness mechanisms (MCAR, MAR, MNAR) affect your conclusions. [26]
- Power Analysis: Conduct power analysis before data collection to ensure adequate sample size. Underpowered studies increase both false positive and false negative rates. [30]
Table 1: Comparison of Missing Data Handling Methods in Clinical Trials
| Method | Bias Risk | Handling of Uncertainty | Regulatory Acceptance | Best Use Case |
|---|---|---|---|---|
| Complete Case Analysis | High | Poor | Low | Minimal missingness (<5%) MCAR only |
| Last Observation Carried Forward (LOCF) | High | Poor | Decreasing | Historical comparisons only |
| Single Imputation | Medium | Poor | Low | Not recommended for primary analysis |
| Multiple Imputation | Low | Good | High | Primary analysis with missing data |
| MMRM | Low to Medium | Good | High | Repeated measures with monotone missingness |
Frequently Asked Questions
MMRM Implementation Questions
Q: When should I choose MMRM versus multiple imputation for handling missing data in longitudinal studies?
A: The choice depends on your data structure and research question:
- Use MMRM when you have longitudinal data with monotone missingness patterns (dropouts) and complete baseline covariates. MMRM uses all available data without explicit imputation. [26]
- Use multiple imputation when you have intermittent missingness, missing baseline covariates, or more than two timepoints. [26]
- For clinical trials with repeated measures, MMRM is often the preferred primary analysis method. [16]
Q: How do I specify time-by-covariate interactions in MMRM correctly?
A: Always include interactions between time and baseline covariates in your MMRM model. For example, in R's mmrm package: [25]
Omitting these interactions can eliminate the power advantage of MMRM over complete-case ANCOVA. [25]
Multiple Implementation Questions
Q: Should I impute at the item level or scale score level for multi-item questionnaires?
A: Impute at the item level rather than the composite score level. Empirical studies comparing EQ-5D-5L data found that mixed models after multiple imputation of items yielded different (typically lower) scores at follow-up compared to score-level imputation. [26]
Q: How many imputations are sufficient for my study?
A: While traditional rules suggested 3-5 imputations, modern recommendations are higher:
- Start with at least 20 imputations
- For higher percentages of missing data (>30%), use 40-100 imputations
- The number should be at least equal to the percentage of incomplete cases [27] [28]
False Positive Concerns
Q: How can I minimize false positives when analyzing screening data with multiple endpoints?
A: Implement a hierarchical testing strategy:
- Pre-specify primary, secondary, and exploratory endpoints
- Use gatekeeping procedures for multiple families of endpoints
- Apply False Discovery Rate (FDR) control within endpoint families
- Consider Bayesian approaches for false positive control [30] [29]
Q: Does handling missing data affect false positive rates?
A: Yes, inadequate handling of missing data can inflate false positive rates. Complete case analysis and single imputation methods can:
- Introduce selection bias
- Produce artificially narrow confidence intervals
- Increase both type I and type II error rates [16]
Table 2: Impact of Statistical Decisions on Error Rates
| Statistical Decision | Impact on False Positives | Impact on False Negatives | Recommendation |
|---|---|---|---|
| No multiple testing correction | Dramatically increases | Variable | Always correct for multiple comparisons |
| Complete case analysis with >5% missingness | Increases | Increases | Use MMRM or MI |
| Underpowered study (<80% power) | Variable | Increases | Conduct power analysis pre-study |
| Inappropriate covariance structure | Variable | Increases | Use unstructured when feasible |
Workflow Diagrams
Multiple Imputation Workflow
Multiple Imputation Process Flow
MMRM Implementation Checklist
MMRM Implementation Steps
Research Reagent Solutions
Table 3: Essential Software Tools for MMRM and Multiple Imputation
| Tool Name | Function | Implementation Notes | Reference |
|---|---|---|---|
| mmrm R Package | Fits MMRM models | Uses Template Model Builder for fast convergence; supports various covariance structures | [24] |
| mice R Package | Multiple imputation using chained equations | Flexible for different variable types; includes diagnostic tools | [31] |
| PROC MIXED (SAS) | MMRM implementation | Industry standard for clinical trials; comprehensive covariance structures | [16] |
| PROC MI (SAS) | Multiple imputation | Well-documented for clinical research; integrates with analysis procedures | [16] |
| brms.mmrm R Package | Bayesian MMRM | Uses Stan backend; good for complex random effects structures | [32] |
Advanced Technical Considerations
Bayesian MMRM Validation
When implementing Bayesian MMRM using packages like {brms}, validation is crucial:
- Use simulation-based calibration to check implementation correctness
- Be aware that complex models with treatment groups and unstructured covariance may have identification issues
- Prior specification strongly influences results, particularly for covariance parameters [32]
Multilevel Multiple Imputation
For clustered or multilevel data (patients within hospitals, students within schools):
- Use multilevel imputation models that account for the data structure
- Specify random effects appropriately in the imputation model
- For longitudinal data, restructure from wide to long format before imputation [31]
Sensitivity Analyses
Always conduct sensitivity analyses for missing data assumptions:
- Compare results under different missingness mechanisms (MAR vs MNAR)
- Use pattern-mixture models or selection models to assess robustness
- Document all assumptions about missing data in your statistical analysis plan [26] [16]
Leveraging Entity Resolution and Advanced Analytics for Improved Match Precision
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: What are the most common data quality issues that cause false positives in entity resolution for research data?
False positives often originate from data quality issues and inappropriate matching thresholds. Common causes include:
- Identifier Problems: Unique IDs that are null, missing, repeated, or not unique within or across data sources can cause erroneous matches [33].
- Inconsistent Formats: The same entity may appear with different formatting across systems (e.g., "Jane Smith" vs. "Smith, Jane"), leading matching algorithms to treat them as distinct entities [34] [35].
- Ambiguous Entity Information: Some records may look similar but refer to different entities (e.g., two people with the same name and birthdate), creating uncertainty that simple rules cannot resolve [34].
Q2: How can I reduce the manual review workload in my entity resolution process without compromising accuracy?
Implementing a dual-threshold approach with optimization can significantly reduce manual review. Research has shown that by using particle swarm optimization to tune algorithm parameters, the manual review size can be reduced from 11.6% to 2.5% for deterministic algorithms and from 10.5% to 3.5% for probabilistic algorithms, while maintaining high precision [36]. Furthermore, employing active learning strategies, where only the most informative record pairs are sampled for labeling, can achieve comparable optimization results with a training set of 3,000 records instead of 10,000 [36].
Q3: What is the difference between rule-based and ML-powered matching, and when should I use each?
- Rule-Based Matching: Uses a set of customizable, predefined rules (e.g., exact matching, fuzzy matching) to find matches. It is reliable when unique identifiers are present and offers high transparency [37] [34]. However, it can be brittle with messy or incomplete data.
- ML-Powered Matching: Uses a machine learning model that analyzes patterns holistically across all record fields. It is more powerful for accounting for errors, missing information, and subtle similarities that rule-based systems might miss. It provides a confidence score for each match, helping to rank accuracy [37]. ML-based matching is often preferable for complex, noisy data where deterministic rules are insufficient.
Q4: Our research data is fragmented across multiple siloed systems. How can we integrate it for effective entity resolution?
A robust data preparation stage is critical. This involves:
- Standardization: Converting data into consistent formats (e.g., date formats, phone numbers).
- Normalization: Text normalization to handle typos and inconsistencies [34].
- Enrichment: Augmenting records with reliable reference data to improve match quality [35]. Building or buying unified data platforms that can consolidate these fragmented sources is a key step before matching can begin [38].
Troubleshooting Guides
Issue: High Rate of False Positives in Matching Results
| Potential Cause | Diagnostic Steps | Resolution |
|---|---|---|
| Overly permissive matching rules or low confidence thresholds. | Review the rules and confidence scores of the false positive pairs. Analyze which fields contributed to the match. | Adjust matching rules to be more strict. For ML-based matching, increase the confidence score threshold required for an automatic match [37]. |
| Poor data quality in key identifier fields. | Profile data to check for nulls, inconsistencies, and formatting variations in fields used for matching (e.g., SSN, names) [35]. | Implement or enhance data cleaning and standardization pipelines before the matching process [34]. |
| Lack of a manual review process for ambiguous cases. | Check if your workflow has a "potential match" or "indeterminate" category for records that fall between match/non-match thresholds [36]. | Implement a dual-threshold system that classifies results into definite matches, definite non-matches, and a set for manual review. This prevents automatic, potentially incorrect, classifications [36]. |
Issue: Entity Resolution Job Fails or Produces Error Files
| Potential Cause | Diagnostic Steps | Resolution |
|---|---|---|
| Invalid Unique IDs in the source data. | Check the error log or file generated by the service. Look for entries related to the Unique ID [33]. | Ensure the Unique ID field is present in every row, is unique across the dataset, and does not exceed character limits (e.g., 38 characters for some systems) [33]. |
| Use of reserved field names in the schema. | Review the schema mapping for field names like MatchID, Source, or ConfidenceLevel [33]. |
Create a new schema mapping, renaming any fields that conflict with reserved names used by the entity resolution service [33]. |
| Internal server error. | Check if the error message indicates an internal service failure [39]. | If the error is due to an internal server error, you are typically not charged, and you can retry the job. For persistent issues, contact technical support [33]. |
Experimental Protocols & Methodologies
Protocol 1: Optimizing a Dual-Threshold Entity Resolution System
This methodology is based on a published study that successfully reduced manual review while maintaining zero false classifications [36].
1. Objective: To tune the parameters of entity resolution algorithms (Deterministic, Probabilistic, Fuzzy Inference Engine) to minimize the size of a manual review set, under the constraint of no false classifications (PPV=NPV=1) [36].
2. Materials & Reagents:
- Data Source: Clinical data warehouse or similar research database with known duplicate records.
- Algorithms: Simple Deterministic, Probabilistic (Expectation-Maximization), Fuzzy Inference Engine (FIE).
- Optimization Framework: Particle Swarm Optimization (PSO) or a similar computational optimization technique.
- Computing Environment: Sufficient processing power for iterative model training and evaluation.
3. Step-by-Step Procedure:
- Step 1: Data Preparation. Standardize and clean the data. Remove stop-words and punctuation. Standardize names using a lookup table and validate critical fields like Social Security Numbers [36].
- Step 2: Blocking. Apply a blocking procedure (e.g., matching on first name + last name, last name + date of birth) to limit the search space to potential duplicate record pairs [36].
- Step 3: Generate Gold Standard Data. Randomly select a large set of record-pairs (e.g., 20,000). Have these reviewed by multiple experts in a stepwise process to establish a definitive match/non-match status for each pair. Split this into a training set (e.g., 10,000 pairs) and a held-out test set (e.g., 10,000 pairs) [36].
- Step 4: Define Algorithm and Baselines. Select the algorithms to optimize. Define a baseline set of parameters for each based on literature or preliminary experimentation [36].
- Step 5: Optimize Parameters. Run the optimization process (e.g., PSO) on the training set. The objective function should seek to minimize the number of record-pairs classified into the "manual review" category, while ensuring no pairs are misclassified [36].
- Step 6: Evaluate. Apply the optimized algorithms to the held-out test set. Measure the size of the manual review set and the classification accuracy.
4. Quantitative Data Summary:
| Algorithm | Baseline Manual Review | Optimized Manual Review | Precision after Optimization |
|---|---|---|---|
| Simple Deterministic | 11.6% | 2.5% | 1.0 |
| Fuzzy Inference Engine (FIE) | 49.6% | 1.9% | 1.0 |
| Probabilistic (EM) | 10.5% | 3.5% | 1.0 |
Data derived from training on 10,000 record-pairs using particle swarm optimization [36].
Protocol 2: Active Learning for Efficient Training Set Labeling
1. Objective: To reduce the size of the required training set for entity resolution algorithm optimization by strategically sampling the most informative record pairs.
2. Procedure:
- Step 1: Start with a small, random sample of record-pairs (e.g., 2,000) from the total training pool.
- Step 2: Have an expert label these pairs with match/non-match status.
- Step 3: Run a preliminary optimization on this small set.
- Step 4: Use a marginal uncertainty sampling strategy. Apply the current model to the entire unlabeled pool and select a small batch of additional records (e.g., 25 pairs) that are closest to the match/non-match thresholds [36].
- Step 5: Get expert labels for this new, informative batch.
- Step 6: Retrain/optimize the model with the enlarged training set.
- Step 7: Repeat steps 4-6 for a set number of iterations or until performance plateaus. The cited study achieved high performance with a total of 3,000 records using this method, compared to 10,000 with random sampling [36].
Workflow Visualization
Entity Resolution Workflow
Dual-Threshold Decision Logic
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function / Purpose |
|---|---|
| Particle Swarm Optimization (PSO) | A computational method for iteratively optimizing algorithm parameters to find a minimum or maximum of a function. Used to tune matching thresholds to minimize manual review [36]. |
| Fuzzy Inference Engine (FIE) | A rule-based deterministic algorithm that uses a set of functions and rules to map similarity scores onto weights for determining matches. Highly tunable and can achieve high precision [36]. |
| Expectation-Maximization (EM) Algorithm | A probabilistic method for finding maximum-likelihood estimates of parameters in statistical models. Used in the Fellegi-Sunter probabilistic entity resolution model to estimate m and u probabilities [36]. |
| Levenshtein Edit Distance | A string metric for measuring the difference between two sequences. Calculates the minimum number of single-character edits required to change one word into the other. Used for calculating similarity between text fields [36]. |
| Active Learning Sampling | A machine learning strategy where the algorithm chooses the most informative data points to be labeled by an expert. Reduces the total amount of labeled data required for training [36]. |
| Blocking / Indexing | A method to reduce the computational cost of entity resolution by grouping records into "blocks" and only comparing records within the same block. Critical for scaling to large datasets [36] [34]. |
Integrating AI and Machine Learning for Smarter, Context-Aware Screening
This technical support center is designed for researchers and scientists integrating Artificial Intelligence (AI) and Machine Learning (ML) into data screening processes. A core challenge in this integration is managing false positives—instances where the system incorrectly flags a negative case as positive [40]. This guide provides troubleshooting and methodologies to help you diagnose, understand, and mitigate these issues, ensuring your AI tools are both smart and reliable.
Troubleshooting Guides
Guide 1: Addressing a High Rate of False Positives
A high false positive rate can overwhelm resources and obscure true results.
- Problem: Your AI screening system is generating an unexpectedly large number of false alerts.
- Symptoms: Low precision; too many non-relevant cases requiring manual review.
- Impact: Wasted computational and human resources, potential missed true positives due to alert fatigue.
Step-by-Step Resolution:
Audit Your Training Data
- Action: Check the labels in your training dataset for inaccuracies. A model trained on mislabeled data will learn incorrect patterns [41].
- How: Manually review a sample of data points that were used to train the model, especially those from the classes contributing most to the false positives.
Conduct an Error Analysis
- Action: Systematically analyze the cases your model is getting wrong [41].
- How: Create a new dataset containing both the target and model-predicted values. Group this data by feature categories and calculate the accuracy and error rate for each group. This will identify specific scenarios where your model fails (e.g., "The model has a 70% error rate for customers with a 'Month-to-month' contract") [41].
Evaluate Feature Relevance
- Action: Determine if the model is using features that are not causally linked to the outcome.
- How: Use model interpretation tools (e.g., SHAP, LIME) to see which features are driving the predictions for the false positive cases. Irrelevant features can lead the model astray.
Tune the Decision Threshold
- Action: Adjust the probability threshold used to classify a case as "positive."
- How: By default, this threshold is often 0.5. Increasing it to a higher value (e.g., 0.7 or 0.8) will make the model more conservative, only making a positive classification when it is more confident, thereby reducing false positives.
Implement a Replicate Testing Strategy
- Action: For critical screenings, don't rely on a single model decision. Use a majority rule strategy on multiple tests [42].
- How: Run multiple independent assays or model inferences on the same sample. A case is only considered a true positive if it returns a positive result in a majority of the tests (e.g., 2 out of 3). This strategy exponentially reduces the effective false-positive rate [42].
Guide 2: Dealing with a "Black Box" Model That Lacks Explainability
Regulators and stakeholders need to understand why an AI system makes a decision.
- Problem: Your model's predictions are not interpretable, making it difficult to explain alerts to colleagues or regulators [43].
- Symptoms: Inability to answer the question, "Why did the system flag this specific case?"
- Impact: Eroded trust in the system, regulatory compliance risks, and difficulty diagnosing model errors [43].
Step-by-Step Resolution:
Integrate Explainable AI (XAI) Methods
- Action: Use post-hoc explanation tools to shed light on individual predictions.
- How: Employ libraries like
SHAPorLIMEto generate "reason codes" for each prediction. These tools can highlight the top features that contributed to a specific classification, turning a black-box prediction into an interpretable report.
Ensure Comprehensive Documentation
Create an Auditable Trail
- Action: Ensure that every decision made by the AI system can be reconstructed and reviewed later [43].
- How: Log all inputs, the model's version, the resulting prediction, and the confidence score for every screening event. This creates a reliable record for internal audits and regulatory inquiries.
Validate with Domain Experts
- Action: Partner with subject-matter experts to review the model's explanations.
- How: Regularly present the model's top false positive cases and the corresponding XAI reason codes to domain experts. Their feedback will help you validate if the model's "reasoning" is sound and align the model's behavior with domain knowledge.
Frequently Asked Questions (FAQs)
Q1: Our AI model performs well on validation data but fails in production with real-world data. What could be the cause? A: This is often a sign of data drift or a training-serving skew. The data your model sees in production has likely changed from the data it was trained and validated on. To address this:
- Monitor Data Distributions: Continuously monitor the statistical properties of incoming production data and compare them to your training set.
- Establish MLOps Practices: Implement robust Machine Learning Operations (MLOps) to manage, version, and monitor models and data continuously, preventing the deployment of brittle systems [44].
- Retrain Regularly: Schedule periodic model retraining with freshly labeled production data to keep the model adapted to current conditions.
Q2: How can we measure the true business impact of false positives in our screening process? A: Beyond technical metrics like precision, you should track operational costs. Key performance indicators (KPIs) include:
- Time-to-Investigation: The average time analysts spend reviewing a false positive alert.
- Resource Allocation: The percentage of total analyst hours consumed by false positives.
- Opportunity Cost: The number of true positive investigations that were delayed or missed due to time spent on false alerts. Tracking these metrics helps build a business case for investing in AI model refinement.
Q3: What is the regulatory stance on using AI for critical screening, such as in drug development or financial compliance? A: Regulators welcome innovation but emphasize accountability. The core principle is that technology does not transfer accountability [43]. Institutions, not algorithms, are held responsible for failures. Key expectations include:
- Explainability: The ability to understand and explain the logic behind the system's decisions [43].
- Governance: A documented framework for how models are designed, validated, and controlled [43].
- Human Oversight: A hybrid approach where AI handles bulk data, but humans focus on complex, high-stakes investigations is considered most defensible [43].
Q4: Are simpler models like logistic regression sometimes better than complex deep learning models for screening? A: Yes, absolutely. A common mistake is chasing complexity before nailing the basics [44]. Simpler models like linear regression or pre-trained models often provide greater ROI, are easier to interpret and debug, and require less data. You should always start simple to establish a baseline and only increase complexity if it yields a significant and necessary improvement [44].
Experimental Protocols & Data
Protocol: Replicate Testing with Majority Rule for False Positive Reduction
This methodology is designed to minimize the dilution of efficacy estimates in clinical trials or the accumulation of false positives in screening caused by imperfect diagnostic assays or AI models [42].
1. Principle If multiple repeated runs of an assay or model inference can be treated as independent, requiring multiple positive results to confirm a case can drastically reduce the effective false positive rate.
2. Procedure
- Step 1: For a given sample, perform
nindependent tests (wherenis an odd number, typically 3). - Step 2: Apply a "majority rule." A case is only confirmed as positive if at least
mtests return a positive result, wherem = (n/2 + 1). - Step 3: Calculate the new, effective false positive rate (
FP_n,m) using the binomial distribution formula [42]:FP_n,m = Σ (from k=m to n) of [n!/(k!(n-k)!] * FP^k * (1-FP)^(n-k)WhereFPis the original false positive rate of a single test.
3. Application Example This strategy is particularly powerful in clinical trials where frequent longitudinal testing is required. It prevents the accumulation of false positives over time, which would otherwise systematically bias (dilute) the estimated efficacy of an intervention downward [42].
Performance Data of Selected AI Detection Tools
The following table summarizes the performance of various AI detection tools as reported in recent studies. Note: Performance is highly dependent on the specific versions of the AI and detection tools and can change rapidly. This data should be used to understand trends, not to select a specific tool [45].
Table 1: Accuracy of Tools in Identifying AI-Generated Text
| Tool Name | Kar et al. (2024) | Lui et al. (2024) |
|---|---|---|
| Copyleaks | 100% | |
| GPT Zero | 97% | 70% |
| Originality.ai | 100% | |
| Turnitin | 94% | |
| ZeroGPT | 95.03% | 96% |
Table 2: Overall Accuracy in Discriminating Human vs. AI Text
| Tool Name | Perkins et al. (2024) | Weber-Wulff (2023) |
|---|---|---|
| Crossplag | 60.8% | 69% |
| GPT Zero | 26.3% | 54% |
| Turnitin | 61% | 76% |
Source: Adapted from Jisc's National Centre for AI [45].
Key Insight: Mainstream, paid detectors like Turnitin are engineered for educational use and prioritize a low false positive rate (often cited as 1-2%), which is crucial in high-stakes environments where false accusations are harmful [45].
Visualizing the AI Screening Pipeline
Workflow for AI-Powered Screening with Human Oversight
This diagram illustrates a robust and defensible workflow for integrating AI into a screening process, emphasizing human oversight and continuous improvement to manage false positives.
Replicate Testing Strategy Logic
This diagram outlines the decision-making process for the replicate testing "majority rule" strategy used to minimize false positives.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Components for an AI Screening Research Pipeline
| Item | Function & Explanation |
|---|---|
| High-Quality Labeled Data | The foundational reagent. AI models learn from data; inaccurate, incomplete, or biased labels will directly lead to high false positive rates and poor model performance [43] [41]. |
| Explainable AI (XAI) Library | A tool for model diagnosis. Libraries like SHAP or LIME help interpret "black box" models by identifying which features contributed most to a specific prediction, which is crucial for troubleshooting and regulatory compliance [43]. |
| A/B Testing Platform | The framework for objective evaluation. This allows you to test a new model against a current one in production to see which performs better on real-world data, preventing the deployment of models that degrade performance [44]. |
| MLOps Platform | The infrastructure for sustainable AI. MLOps (Machine Learning Operations) provides tools for versioning data and models, monitoring performance, and managing pipelines, preventing systems from becoming brittle and unmaintainable [44]. |
| Gas Chromatography–Mass Spectrometry (GC-MS) | (For clinical/biological contexts) A confirmatory test. When an initial immunoassay screen (or AI-based screen) returns a positive result, GC-MS provides a highly accurate, definitive analysis to rule out false positives, setting a gold standard for verification [40]. |
Troubleshooting and Optimizing Screening Systems for Maximum Efficiency
Troubleshooting Guides
Guide 1: Addressing High False Positive Rates in Screening Data
Problem: My screening experiments are generating an unmanageably high number of false positive alerts, overwhelming analytical resources and obscuring true results.
Solution: A systematic approach targeting the root causes of false positives, from data entry to algorithmic matching.
1. Check Data Completeness and Standardization:
- Action: Verify that critical data fields (e.g., compound IDs, sample identifiers, subject names) contain no null or missing values. Ensure data conforms to standardized formats (e.g., dates, units of measure).
- Rationale: Incomplete or non-standardized data is a primary driver of erroneous matches and false alerts [46]. Standardization ensures uniform interpretation by screening algorithms.
- Methodology: Run data profiling scripts to calculate the percentage of missing values in key columns. Implement automated validation rules to enforce format standards at the point of data entry [47].
2. Improve Matching Algorithms:
- Action: Move beyond exact-string matching to implement fuzzy matching algorithms that account for phonetic similarities, nicknames, and transliteration variations.
- Rationale: Rigid matching strategies cannot account for real-world data variations, flagging near-misses as potential positives [46].
- Methodology: Configure your screening system's similarity threshold based on your risk appetite. Utilize secondary data attributes (e.g., geographic location, structural properties) for automated discounting of weak matches [46].
3. Implement a Risk-Based Screening Policy:
- Action: Avoid a "one-size-fits-all" screening approach. Create multiple screening configurations tailored to different customer or data types.
- Rationale: Overscreening increases noise. A targeted approach focuses resources on the highest-risk areas, significantly reducing unnecessary alerts [46].
4. Utilize a Sandbox for Testing and Tuning:
- Action: Use an isolated sandbox environment to test new screening rules and configurations against historical data before deploying them to the live system.
- Rationale: This allows for the optimization of rules and thresholds without disrupting ongoing operations, providing a safe space to measure the impact on false positive rates [46].
Guide 2: Resolving Data Inconsistencies Across Multiple Source Systems
Problem: The same data element exists in different formats across source systems (e.g., clinical databases, lab instruments), leading to conflicting results and unreliable analysis.
Solution: Establish a single source of truth through data validation, transformation, and integration protocols.
1. Perform Data Profiling and Source Verification:
- Action: Conduct a comprehensive assessment to understand the structure, content, and quality of data in all source systems. Cross-reference entries to identify discrepancies.
- Rationale: You cannot fix what you don't measure. Profiling illuminates the scale and nature of inconsistency problems [48] [49].
- Methodology: Employ column-based profiling to get statistical information (e.g., value frequencies, patterns) and rule-based profiling to validate data against defined business logic [48].
2. Establish Robust Data Transformation and Cleansing:
- Action: Develop and execute scripts or use data quality tools to parse, standardize, and cleanse data. This includes correcting errors, removing duplicates, and converting units into a consistent format.
- Rationale: Cleansing rectifies existing inconsistencies, while standardized transformation rules prevent new ones from being introduced during data integration [47].
- Methodology: In ETL (Extract, Transform, Load) processes, implement steps for error correction, standardization, and deduplication. Maintain detailed documentation of all transformation rules for auditability [47].
3. Enforce Data Governance and User Training:
- Action: Define clear data ownership and accountability. Train all personnel involved in data entry on standardized protocols and the importance of data quality.
- Rationale: Many data inconsistencies originate from human error during manual entry. A strong governance culture addresses this at the source [47].
Frequently Asked Questions (FAQs)
Q1: What are the most critical dimensions of data quality to monitor for reducing false positives in research? The most critical dimensions are Completeness, Accuracy, Consistency, and Validity [50] [48] [49]. Ensuring your datasets are free from missing values, accurately reflect real-world entities, are uniform across sources, and conform to defined business rules directly impacts the reliability of screening algorithms and reduces erroneous alerts.
Q2: How can I quantitatively measure the quality of my input data? You can track several key data quality metrics [50]:
- Number of Empty Values: The count of records with missing fields in critical columns.
- Duplicate Record Percentage: The proportion of repeated entries in a dataset.
- Data Validity Score: The percentage of data that conforms to predefined format and rule requirements.
- Data Transformation Error Rate: The number of failures during data conversion processes, indicating underlying quality issues.
Q3: Our team is small. What's the first step we should take to improve data quality? Begin with a focused data quality assessment on your most critical dataset [51]. Profile the data to identify specific issues like missing information, duplicates, or non-standardized formats. Even a simple, one-time cleanup of this dataset and the implementation of basic validation rules for future data entry can yield significant improvements in research outcomes without requiring extensive resources.
Q4: Can AI and machine learning help with data quality? Yes, Augmented Data Quality (ADQ) solutions are transforming the field [49]. These tools use AI and machine learning to automate processes like profiling, anomaly detection, and data matching. They can learn from your data to recommend validation rules, identify subtle patterns of errors, and significantly reduce the manual effort required to maintain high-quality data.
Data Quality Defense Workflow
The following diagram visualizes the multi-layered defense system for ensuring data quality in screening research, from initial entry to final analysis.
Data Quality Defense System
Research Reagent Solutions: Essential Tools for Data Quality
The following table details key "reagents" – in this context, tools and methodologies – essential for conducting high-quality data screening and validation in research.
| Tool / Methodology | Primary Function in Data Quality |
|---|---|
| Data Profiling Tools [48] | Provides statistical analysis of source data to understand its structure, content, and quality, identifying issues like missing values, outliers, and patterns. |
| Fuzzy Matching Algorithms [46] | Enables sophisticated name/entity matching by accounting for phonetic similarities, nicknames, and typos, reducing false positives/negatives. |
| Sandbox Environment [46] | Offers an isolated space to test, tune, and optimize screening rules and configurations using historical data without impacting live systems. |
| Automated Data Validation Rules [47] [52] | Enforces data integrity by automatically checking incoming data against predefined business rules and formats, preventing invalid data entry. |
| Augmented Data Quality (ADQ) [49] | Uses AI and machine learning to automate profiling, anomaly detection, and rule discovery, enhancing the efficiency and scope of quality checks. |
Quantitative Data Quality Metrics
The table below summarizes key metrics for measuring data quality, helping researchers quantify issues and track improvement efforts.
| Data Quality Dimension | Key Metric to Measure | Calculation / Description |
|---|---|---|
| Completeness [50] | Number of Empty Values | Count or percentage of records with missing (NULL) values in critical fields. |
| Uniqueness [50] | Duplicate Record Percentage | Percentage of records that are redundant copies within a dataset. |
| Validity [50] [49] | Data Validity Score | Percentage of data values that conform to predefined syntax, format, and rule requirements. |
| Accuracy [49] | Data-to-Errors Ratio | Number of known errors (incomplete, inaccurate, redundant) relative to the total size of the dataset. |
| Timeliness [50] | Data Update Delays | The latency between when a real-world change occurs and when the corresponding data is updated in the system. |
Understanding False Positives in Screening Research
What is a false positive in screening data and why is it a problem?
In cancer screening, a false positive is an apparent abnormality on a screening test that, after further evaluation, is found not to be cancer [53]. While ruling out cancer is an essential part of the screening process, false positives create significant problems:
- Patient Burden: They lead to unnecessary stress, anxiety, and inconvenience for patients [53]. The process can take 1-2 years, causing lingering worry about a potential cancer diagnosis [53].
- Reduced Future Screening: Women who experience a false-positive mammogram are less likely to return for future routine screening, potentially missing early cancer detection [53].
- Healthcare Costs: False positives generate obligations for additional imaging, biopsies, and other follow-up tests, increasing system costs [53] [54].
What is the quantitative impact of false positives in different screening paradigms?
The burden of false positives varies dramatically depending on the screening strategy. The table below compares two hypothetical blood-based testing approaches for 100,000 adults [54].
| Screening System Metric | Single-Cancer Early Detection (SCED-10) | Multi-Cancer Early Detection (MCED-10) |
|---|---|---|
| Description | 10 individual tests, one for each of 10 cancer types | One test targeting the same 10 cancer types |
| Cancers Detected | 412 | 298 |
| False Positives | 93,289 | 497 |
| Positive Predictive Value | 0.44% | 38% |
| Efficiency (Number Needed to Screen) | 2,062 | 334 |
| Estimated Cost | $329 Million | $98 Million |
This data shows that a system using multiple SCED tests, while detecting more cancers, produces a vastly higher number of false positives—over 150 times more per annual screening round—and is significantly more costly and less efficient than a single MCED test [54].
Troubleshooting Guides: Mitigating False Positives
How can I reduce false positives in image-based screening (e.g., CT scans)?
Problem: A high rate of false-positive nodules in lung cancer CT screening is leading to unnecessary follow-up scans, higher costs, and patient anxiety.
Solution: Integrate a validated AI algorithm for pulmonary nodule malignancy risk stratification.
Protocol: AI-Assisted Nodule Assessment
- Data Acquisition: Obtain low-dose CT scan images from the screening population.
- AI Model Application: Process the images through a deep learning algorithm trained on large datasets (e.g., >16,000 lung nodules, including over 1,000 malignancies) [55].
- Risk Stratification: The AI model generates a 3D image of each nodule and calculates a malignancy risk score [55].
- Clinical Decision:
- High-Risk Score: Proceed with standard follow-up procedures (e.g., short-interval follow-up scan or biopsy).
- Low-Risk Score: Categorize the nodule as probably benign, avoiding immediate further action.
Expected Outcome: This methodology has been shown to reduce false positives by 40% in the difficult group of nodules between 5-15 mm, while still detecting all cancer cases [55].
How can I configure system rules to minimize cumulative false-positive burden in a multi-test environment?
Problem: Our research uses a panel of sequential single-cancer tests, and the cumulative false-positive rate is overwhelming our diagnostic workflow.
Solution: Re-evaluate the screening paradigm from multiple single-cancer tests to a single multi-cancer test with a low fixed false-positive rate.
Protocol: System-Level Screening Configuration
- Define Cancer Targets: Identify the set of cancers for early detection (e.g., the cancers responsible for the highest number of deaths) [54].
- Performance Benchmarking: Model two systems for the same population and cancer targets:
- Compare System Metrics: Calculate and compare the total number of false positives, positive predictive value, and required diagnostic investigations for each system (refer to the table in FAQ 1.2) [54].
- Implement and Monitor: Adopt the system that offers the best balance of cancer detection and manageable false positives for your resource constraints. Continuously monitor adherence, as false positives can deter individuals from future screening [53].
How can I address the "human factor" where false positives reduce future screening adherence?
Problem: Study participants who experience a false-positive result are not returning for their next scheduled screening, creating a dropout bias.
Solution: Implement pre-screening education and post-result communication protocols.
Protocol: Participant Communication and Support
Pre-Screening Education:
- Frame the Process: Clearly explain that a screening test is not diagnostic and that follow-up testing is a normal part of the process to rule out cancer [53].
- Discuss Likelihood: Inform participants about the chance of a false positive (e.g., over half of women screened annually for 10 years will experience one) [53].
- Manage Expectations: Emphasize that a false-positive result does not reflect an error but is inherent to sensitive early detection [53].
Post-Result Support:
- Prompt Communication: Provide clear, timely results and explain the meaning of a false-positive finding.
- Streamline Follow-Up: Explore operational changes, such as same-day follow-up imaging for abnormal results, to reduce anxiety and inconvenience [53].
- Reinforce Value: When giving the "all clear," affirm that the additional testing was an important part of ensuring early detection, not a waste of effort [53].
Experimental Protocols for Validation
Protocol: External Validation of an AI Model for False-Positive Reduction
This protocol is based on a study that validated a deep learning algorithm for lung nodule malignancy risk stratification using European screening data [55].
1. Objective: To independently test the performance of a pre-trained AI model in reducing false-positive findings on low-dose CT scans from international screening cohorts.
2. Research Reagent Solutions
| Item | Function |
|---|---|
| Low-Dose CT Image Datasets | Source of imaging data for model testing and validation. Includes nodules of various sizes and pathologies. |
| Pre-Trained Deep Learning Algorithm | The core AI model that performs 3D analysis of pulmonary nodules and outputs a malignancy risk score. |
| PanCan Risk Model | A widely used clinical risk model for pulmonary nodules; serves as the benchmark for performance comparison. |
| Validation Cohorts | Independent, multi-national datasets (e.g., from Netherlands, Belgium, Denmark, Italy) not used in model training. |
3. Methodology:
- Data Sourcing: Obtain de-identified CT scans and associated clinical data (including final diagnosis) from large, international screening studies.
- AI Inference: Process all scans through the AI algorithm to generate a malignancy risk score for each detected pulmonary nodule.
- Benchmark Comparison: Compare the AI's performance against the current standard (e.g., PanCan model) using the same set of nodules.
- Outcome Analysis: Calculate key performance metrics, focusing on the reduction of false-positive recommendations for follow-up while maintaining 100% sensitivity for confirmed cancers, particularly in the 5-15mm nodule size group [55].
4. Key Metrics:
- False-Positive Reduction Rate
- Overall Sensitivity and Specificity
- Performance in specific nodule size ranges
The Scientist's Toolkit: Research Reagent Solutions
| Tool or Reagent | Function in Screening Research |
|---|---|
| Multi-Cancer Early Detection (MCED) Test | A single blood-based test designed to detect multiple cancers simultaneously with a very low false-positive rate (<1%) [54]. |
| Validated AI Risk Stratification Algorithm | A deep learning model trained on large datasets to distinguish malignant from benign findings in medical images, reducing unnecessary follow-ups [55]. |
| Stacked Autoencoder (SAE) with HSAPSO | A deep learning framework for robust feature extraction and hyperparameter optimization, shown to achieve high accuracy (95.5%) in drug classification and target identification tasks [56]. |
| Large, Multi-Center Validation Cohorts | Independent datasets from diverse populations and clinical settings, essential for proving the generalizability and real-world performance of a new screening method or algorithm [55]. |
In high-throughput research environments, alert overload is a critical challenge. Security Operations Centers (SOCs) often receive thousands of alerts daily, with only a fraction representing genuine threats [57]. This overwhelming volume creates a significant bottleneck, with studies suggesting that poorly tuned environments can generate false positive rates of 90% or more [58]. For researchers and scientists, this noise directly impacts experimental integrity and operational efficiency, wasting valuable resources on investigating irrelevant alerts instead of focusing on genuine discoveries.
Implementing a risk-scoring framework provides a systematic solution to this problem. By quantifying the potential impact of security events and screening alerts, organizations can prioritize threats and focus resources on the most critical risks [59]. This approach is particularly valuable in drug development and scientific research, where data integrity and system security are paramount. A well-designed triage system transforms chaotic alert noise into actionable intelligence, enabling research professionals to distinguish between insignificant anomalies and genuine incidents that require immediate investigation.
Understanding Risk Scoring Fundamentals
What is Risk Scoring?
Risk scoring uses a numerical assessment to quantify an organization's vulnerabilities and threats [59]. This calculation incorporates multiple factors to generate a combined risk score that quantifies risk levels in a clear, actionable way. The fundamental components of risk scoring include:
- Likelihood Assessment: The probability that a potential threat event will occur
- Impact Analysis: The potential damage or loss that could result from a threat
- Asset Valuation: Determining the criticality of affected systems, data, or experiments
Modern risk scoring has evolved from slow, manual processes into data-driven endeavors leveraging artificial intelligence (AI) and machine learning (ML). These technological advances enable organizations to sift through vast amounts of data at unprecedented speeds, improving assessment accuracy and enabling real-time monitoring and updating of risk scores [59].
The Risk Scoring Process
Implementing an effective risk scoring system involves three key stages [59]:
- Identify assets at risk: Determine which data, physical assets, or personnel are vulnerable, then evaluate associated threats and vulnerabilities.
- Assess each risk event: Evaluate both the likelihood and potential impact of threat events using appropriate assessment matrices.
- Prioritize risks: Use final risk scores to focus efforts and resources on mitigating the highest-priority risks.
Risk Assessment Workflow - This diagram illustrates the cyclical process of risk assessment, from identification through to continuous monitoring.
Implementing Risk Scoring: A Step-by-Step Methodology
Establishing Your Risk Scoring Framework
The foundation of effective risk scoring begins with careful planning and framework development [59]:
- Define Objectives and Criteria: Establish clear risk scoring objectives and develop criteria based on impact, likelihood, and organizational risk appetite. Ensure these criteria align with your overall risk management strategy and relevant industry standards.
- Collect Data and Identify Risks: Gather comprehensive data from internal and external sources. Use a combination of automated tools and expert analysis to identify and catalog potential risks across research operations.
- Develop Scoring Algorithms: Create customized scoring algorithms tailored to your organization's specific needs. Integrate the risk scoring system with existing IT and research infrastructure, ensuring seamless operation within current workflows.
- Train Stakeholders: Conduct training sessions to educate research teams about the risk scoring process and their roles. Consider initial rollout through a pilot project, allowing for adjustments based on feedback before wider implementation.
- Monitor and Update: Continuously monitor system effectiveness and gather feedback for improvements. Regularly review and update risk scoring criteria and algorithms to adapt to new threats and changes in the research landscape.
Core Risk Scoring Formula and Components
The fundamental risk scoring equation combines threat likelihood with potential impact:
Risk Score = Likelihood × Impact
To operationalize this formula, research teams should incorporate these critical components:
- Asset Criticality: Assign values to research systems based on their importance to ongoing experiments and data integrity.
- Threat Intelligence: Integrate current information about known attack patterns and vulnerabilities relevant to research environments [57].
- Contextual Enrichment: Incorporate additional data points such as user role, system ownership, and recent behavioral patterns to validate potential matches [60].
Risk Scoring Components - This diagram shows how various input factors contribute to the final risk score calculation.
Essential Research Reagent Solutions
The following tools and technologies are essential for implementing effective risk scoring in research environments:
Table 1: Research Reagent Solutions for Risk Scoring Implementation
| Solution Category | Specific Tools/Platforms | Primary Function in Risk Scoring |
|---|---|---|
| Network Detection & Response (NDR) | Corelight Open NDR Platform [57] | Provides network evidence and alert enrichment through interactive visual frameworks |
| Security Information & Event Management (SIEM) | Splunk Enterprise Security, Microsoft Sentinel, IBM QRadar [61] | Correlates security events, applies initial filtering, and enables statistical analysis across datasets |
| Endpoint Detection & Response (EDR) | CrowdStrike Falcon [61] | Monitors endpoint activities and provides threat graph capabilities to understand attack progression |
| Entity Resolution Platforms | LexisNexis Risk Solutions [62] | Leverages advanced analytics and precise entity linking to match data points and determine likelihood of matches |
| Automated Threat Analysis | VMRay Advanced Threat Analysis [58] | Provides detailed behavioral analysis to reveal threat intentions beyond simple signature matching |
| AI-Powered Triage | Dropzone AI [61] | Investigates alerts autonomously using AI reasoning, adapting to unique alerts without predefined playbooks |
Troubleshooting Common Risk Scoring Issues
FAQ: Addressing Implementation Challenges
Q: Our research team is overwhelmed by false positives. What configuration changes can reduce this noise? A: Implement these proven techniques to minimize false positives [60]:
- Calibrate Matching Algorithms: Choose appropriate name-matching algorithms (Jaro-Winkler vs. Levenshtein) and adjust similarity thresholds to filter spurious hits while maintaining detection sensitivity.
- Utilize Secondary Identifiers: Incorporate additional data points like user roles, department affiliations, and normal operational patterns to validate potential matches.
- Apply Risk-Based Thresholds: Implement different sensitivity settings based on risk profiles, using stricter matching for critical research systems and relaxed criteria for low-risk environments.
- Leverage Stopwords and Tokenization: Configure systems to ignore common irrelevant terms that often cause mismatches in research contexts.
Q: How can we maintain consistency in risk scoring across different team members? A: Standardization is key to consistent scoring [58]:
- Develop Triage Playbooks: Create standardized procedures that define clear criteria for alert classification, validation steps, and escalation thresholds.
- Implement Severity Scoring: Establish consistent severity scoring based on business impact, threat sophistication, and affected research systems.
- Conduct Regular Training: Ensure all team members understand scoring criteria and application through ongoing education sessions.
- Document Decisions: Maintain records of scoring rationales for future reference and continuous improvement.
Q: What metrics should we track to measure the effectiveness of our risk scoring implementation? A: Focus on these key performance indicators [61]:
Table 2: Essential Risk Scoring Metrics
| Metric | Definition | Target Benchmark |
|---|---|---|
| Mean Time to Conclusion (MTTC) | Total time from detection through final disposition | Hours (vs. industry average of 241 days) |
| False Positive Rate | Percentage of alerts that are false positives | Significant reduction from 90%+ baseline |
| Alert Investigation Rate | Percentage of alerts thoroughly investigated | Increase from 22% industry average |
| Analyst Workload Distribution | Time allocation between false positives vs. genuine threats | >70% focus on genuine threats |
Q: How can we adapt risk scoring models as new threats emerge in our research environment? A: Implement a continuous improvement cycle [59]:
- Regular Model Reviews: Schedule quarterly reviews of scoring algorithms and criteria to ensure relevance.
- Feedback Integration: Establish mechanisms to incorporate analyst feedback and new data to refine accuracy over time.
- Threat Intelligence Integration: Automatically correlate incoming alerts with current threat intelligence feeds [58].
- Performance Monitoring: Track metrics to identify improvement opportunities and optimize detection rules.
Advanced Risk Scoring Techniques
Entity Resolution for Enhanced Match Precision
Entity resolution shifts the focus from alert quantity to quality by bringing relevance and match precision to screening [62]. Rather than using rules-based approaches to accept or reject matches, entity resolution leverages advanced analytics and precise entity linking to match data points, determining the likelihood that two database records represent the same real-world entity.
When entity resolution incorporates risk scoring—ranking matches by severity and match likelihood—it enables quantitative customer risk assessment based on match strength between a customer account and a watch list entity [62]. This approach allows prioritization of alerts with the most severe consequences and greatest likelihood of being true positives, ensuring efficient allocation of investigative resources.
AI and Machine Learning Integration
Modern AI technologies transform risk scoring from static rule-based systems to dynamic, adaptive frameworks [61]. AI SOC agents don't just follow predefined playbooks; they reason through investigations like experienced human analysts would, investigating alerts in 3-10 minutes compared to 30-40 minutes for manual investigation.
These systems provide continuous learning capabilities, refining their accuracy as they process more alerts and incorporate analyst feedback [60]. This creates a virtuous cycle where the system becomes increasingly effective at recognizing legitimate threats while filtering out false positives specific to your research environment. Organizations using AI-powered security operations have demonstrated nearly $2 million in reduced breach costs and 80-day faster response times according to industry research [61].
Frequently Asked Questions
Q1: What is the primary benefit of implementing a feedback loop in our screening algorithms? The core benefit is the continuous reduction of false positives. A feedback loop allows your algorithm to learn from the corrections made by human analysts. This means that over time, the system gets smarter, automatically clearing common false alerts and allowing researchers to focus on analyzing true positives and novel discoveries. Systems designed this way have demonstrated a reduction of false positives by up to 93% [60].
Q2: We use a proprietary algorithm. Can we still integrate analyst feedback? Yes. The principle is tool-agnostic. The key is to log the data points surrounding an analyst's decision. You need to capture the initial alert, the features of the data that triggered it, the analyst's final determination (e.g., "true positive" or "false positive"), and any notes they provide. This dataset becomes the training material for your model's next retraining cycle, regardless of the underlying technology [60].
Q3: How can we ensure the feedback loop doesn't "over-correct" and begin missing true positives? This is managed through a process of supervised learning and continuous validation. The algorithm's performance is consistently measured against a holdout dataset of known true positives. Furthermore, a sample of the alerts automatically cleared by the AI should be audited by senior analysts. This provides a check on the system's learning and ensures its decisions remain explainable and justifiable, maintaining a high degree of accuracy [60].
Q4: What is the simplest way to start building a feedback loop for our research? Begin with a structured logging process. Create a standardized form for your analysts to complete for every alert they review. This form should force them to tag the alert as true/false positive and select from a predefined list of reasons for their decision (e.g., "background signal," "assay artifact," "compound interference"). This consistent, structured data is the foundation for effective model retraining [60].
Troubleshooting Guides
Problem: High Volume of False Positives Overwhelming Analysts
- Description: The screening system generates an excessive number of alerts that upon manual review, are found to be irrelevant, wasting valuable research time.
- Solution:
- Calibrate Matching Algorithms: Adjust the similarity thresholds for your alerts. A higher threshold makes the system stricter. Fine-tune this balance to catch real hits while ignoring harmless variations [60].
- Implement Secondary Filters: Use additional data points to validate alerts. For example, if an alert is based on a name match, cross-reference it with other identifiers (e.g., structural properties, source organism) to automatically dismiss false hits before they reach an analyst [60].
- Enable Automated Suppression: Deploy a dedicated AI agent to handle clear-cut false positives. This agent can learn from historical analyst decisions to automatically clear common false alerts in real-time, dramatically reducing the analyst's workload [60].
Problem: Algorithm Performance Degrades After Implementing Feedback
- Description: After retraining the model with new analyst feedback, the system's overall performance decreases, leading to more errors.
- Solution:
- Check for Biased Feedback: Ensure the feedback data is representative. If analysts only review a certain type of alert, the model will become biased. Broaden the scope of alerts included in the training set.
- Validate on a Clean Set: Always retrain and validate the model on a separate, pristine dataset of known true and false positives. This helps ensure that new learning generalizes well and doesn't just mirror the latest few cases [60].
- Control the Learning Rate: In machine learning terms, reduce the "learning rate" for the model. This means each batch of new feedback has a smaller, more gradual impact on the algorithm, preventing drastic and potentially harmful changes.
Problem: Lack of Trust in Automated Decisions
- Description: Researchers are skeptical of alerts that are automatically cleared by the system and fear that true positives are being missed.
- Solution:
- Ensure Transparent Logging: For every action taken by the AI, a disposition narrative must be automatically generated and logged. This narrative explains the rationale for clearing an alert (e.g., "Cleared due to mismatch on secondary property X") [60].
- Maintain a Full Audit Trail: Every automated decision must be timestamped and stored in an immutable log. This creates a complete history that can be reviewed by compliance officers or senior researchers, building trust through transparency [60].
- Implement a Human-in-the-Loop Protocol: Configure the system so that alerts with a low confidence score or those matching specific high-risk criteria are always escalated for human review, ensuring expert oversight where it matters most [60].
Experimental Protocols & Data
Table 1: WCAG 2.1 Level AAA Color Contrast Requirements for Data Visualization This table outlines the minimum contrast ratios for text and visual elements in diagrams and interfaces, as defined by the Web Content Accessibility Guidelines (WCAG) Enhanced contrast standard [63].
| Element Type | Description | Minimum Contrast Ratio |
|---|---|---|
| Normal Text | Most text content in diagrams, labels, and interfaces. | 7:1 [63] |
| Large Scale Text | Text that is 18pt or 14pt and bold. | 4.5:1 [63] |
| User Interface Components | Visual information used to indicate states and boundaries of UI components. | 3:1 [63] |
Table 2: Configuration Parameters for Alert Tuning This table summarizes key parameters that can be adjusted to fine-tune screening algorithms and reduce false positives [60].
| Parameter | Function | Impact on Screening |
|---|---|---|
| Similarity Threshold | Sets how close a data match needs to be to trigger an alert. | Higher threshold = Fewer, more precise alerts. Lower threshold = More, broader alerts. [60] |
| Stopword List | A list of common but irrelevant terms (e.g., "Ltd," "Inc") ignored by the matching logic. | Prevents false hits triggered by generic, non-discriminatory terms [60]. |
| Secondary Identifiers | Additional data points (e.g., source, molecular weight) used to validate a primary match. | Greatly reduces false positives by requiring corroborating evidence [60]. |
| Risk-Based Thresholds | Applies different sensitivity levels to data based on predefined risk categories. | Focuses stringent screening on high-risk areas, reducing noise in low-risk data streams [60]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for High-Throughput Screening (HTS) Assays
| Reagent / Material | Function in the Experiment |
|---|---|
| Target Protein (e.g., Kinase, Receptor) | The biological molecule of interest against which compounds are screened for activity. |
| Fluorescent or Luminescent Probe | A detectable substrate used to measure enzymatic activity or binding events in the assay. |
| Compound Library | A curated collection of small molecules or compounds screened to identify potential hits. |
| Positive/Negative Control Compounds | Compounds with known activity (or lack thereof) used to validate assay performance and calculate Z'-factor. |
| Cell Line (for cell-based assays) | Engineered cells that express the target protein or pathway being investigated. |
| Lysis Buffer | A solution used to break open cells and release intracellular contents for analysis. |
| Detection Reagents | A cocktail of enzymes, co-factors, and buffers required to generate the assay's measurable signal. |
Workflow Visualization
Algorithm Refinement Loop
Alert Triage Workflow
Validating and Comparing Screening Approaches for Superior Outcomes
Frequently Asked Questions
What do PPV and NPV tell me that sensitivity and specificity do not?
While sensitivity and specificity describe the test's inherent accuracy, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) tell you the probability that a result is correct in your specific population [64] [65].
- Sensitivity/Specificity: Fixed properties of the test itself. Sensitivity is the proportion of true positives the test correctly identifies, while specificity is the proportion of true negatives it correctly identifies [64].
- PPV/NPV: Depend heavily on the prevalence of the condition in your population. PPV is the probability that a positive test result is a true positive, while NPV is the probability that a negative test result is a true negative [65] [66].
This means a test with excellent sensitivity and specificity can have a surprisingly low PPV when used to screen for a rare condition [67].
Why does my screening test have a high false positive rate even though it's "accurate"?
You are likely experiencing the False Positive Paradox [67] [68]. This occurs when the condition you are screening for is rare (low prevalence). Even a test with a low false positive rate can generate more false positives than true positives in this scenario.
The relationship between prevalence, PPV, and false positives is illustrated in the following workflow:
For example, with a disease prevalence of 0.1% and a test with 99% specificity, the vast majority of positive results will be false positives [67].
How can I improve the Positive Predictive Value of my screening method?
The most direct way to improve PPV is to increase the prevalence of the condition in the population you are testing [65]. This can be achieved by:
- Targeted Screening: Moving from general population screening to targeting high-risk sub-populations.
- Sequential Testing: Using a first, highly sensitive test to identify potential positives, followed by a second, highly specific confirmatory test on the initial positives.
The formula for PPV shows its direct dependence on prevalence, sensitivity, and specificity [66]: PPV = (Sensitivity × Prevalence) / [(Sensitivity × Prevalence) + (1 – Specificity) × (1 – Prevalence)]
Quantitative Data Tables
Table 1: Impact of Disease Prevalence on Predictive Values
Assumes a test with 99% Sensitivity and 99% Specificity
| Disease Prevalence | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) |
|---|---|---|
| 0.1% (1 in 1,000) | 9.0% | 99.99% |
| 1% (1 in 100) | 50.0% | 99.99% |
| 10% (1 in 10) | 91.7% | 99.9% |
| 50% (1 in 2) | 99.0% | 99.0% |
Table 2: Real-World Screening Example - Low-Dose CT for Lung Cancer
Data from the National Lung Screening Trial (NLST) [65]
| Metric | Value |
|---|---|
| Sensitivity | 93.8% |
| Specificity | 73.4% |
| Disease Prevalence | ~1.1% |
| Positive Predictive Value (PPV) | 3.8% |
| Interpretation | Over 96% of positive results were false positives, leading to unnecessary follow-up procedures. |
Experimental Protocols
Protocol: Calculating Key Performance Metrics from a 2x2 Contingency Table
This protocol provides a standard method for benchmarking the performance of any screening test against a gold standard.
1. Research Reagent Solutions & Essential Materials
| Item | Function in Experiment |
|---|---|
| Gold Standard Reference Method | Provides the definitive diagnosis for determining true condition status (e.g., clinical follow-up, PCR, biopsy) [64]. |
| Study Population Cohort | A representative sample that includes individuals with and without the target condition. |
| Data Collection Tool | A standardized form or database for recording test results and gold standard results. |
| Statistical Software | For performing calculations and creating the 2x2 contingency table. |
2. Procedure
- Step 1: Conduct Testing - Perform the screening test on all participants in your cohort. Simultaneously (or blinded), determine their true disease status using the gold standard method [64].
- Step 2: Construct a 2x2 Table - Tally the results into a 2x2 contingency table as shown below.
- Step 3: Calculate Metrics - Use the formulas in the diagram below to compute sensitivity, specificity, PPV, and NPV.
The following diagram illustrates the logical relationship between the 2x2 table and the derived metrics:
Troubleshooting Guides
Problem: High Number of False Positives Overwhelming Research Workflow
- Potential Cause: The False Positive Paradox is in effect due to low disease prevalence in your screened population [67].
- Solution:
- Re-evaluate Population: Consider if you can refine your inclusion criteria to create a higher-prevalence cohort.
- Implement a Two-Stage Screening Process: Use a first-line test optimized for high sensitivity (to catch all possible cases) and a second, different test optimized for high specificity to confirm initial positives [65].
Problem: Promising Treatment Fails in Late-Stage Trials
- Potential Cause: False Negatives in early-phase trials can lead to abandoning effective treatments. Early studies are often underpowered (e.g., with 50% power), meaning they have a low probability of detecting a true effect [4].
- Solution:
- Increase Power in Early Trials: Increase the sample size in early-phase trials to achieve higher statistical power (e.g., 80% or more). The cost of larger studies is often offset by the increased probability of correctly identifying effective treatments and the associated profits [4].
Frequently Asked Questions (FAQs)
FAQ 1: How do the false positive rates of single-cancer tests and multi-cancer early detection (MCED) tests compare?
Single-cancer screening tests have variable false positive rates that can accumulate when multiple tests are used. One study estimated the lifetime risk of a false positive is 85.5% for women and 38.9% for men adhering to USPSTF guidelines, which include tests like mammograms and stool-based tests [69]. In contrast, a leading MCED test (Galleri) demonstrates a specificity of 99.6%, meaning the false positive rate is only 0.4% [70]. This high specificity is a deliberate design priority for MCED tests to minimize unnecessary diagnostic procedures when screening for multiple cancers simultaneously [71].
FAQ 2: What is the clinical significance of a false positive MCED test result?
A false positive result indicates a "cancer signal detected" outcome when no cancer is present. Research shows that most individuals with a false positive result remain cancer-free in the subsequent years. In the DETECT-A study, 95 out of 98 participants with a false positive result were still cancer-free after a median follow-up of 3.6 years [72]. The annual cancer incidence rate following a false positive was 1.0% [72]. While a false positive requires diagnostic workup, the data suggests that a comprehensive imaging-based workflow, such as FDG-PET/CT, can effectively rule out cancer with a low long-term risk of a missed diagnosis [72].
FAQ 3: How does the Positive Predictive Value (PPV) of MCED tests compare to established single-cancer tests?
Positive Predictive Value (PPV) is the proportion of positive test results that are true cancers. MCED tests are being developed to have a high PPV. Real-world data for one MCED test showed an empirical PPV of 49.4% in asymptomatic individuals and 74.6% in symptomatic individuals [71]. The test's developer reports a PPV of 61.6% [70]. This is several-fold higher than PPVs for common single-cancer screens like mammography (4.4-28.6%), fecal immunochemical test (FIT) (7.0%), or low-dose CT for lung cancer (3.5-11%) [71].
FAQ 4: What is the potential impact of integrating MCED testing with the standard of care?
Microsimulation modeling of 14 cancer types predicts that adding annual MCED testing to the standard of care (SoC) can lead to a substantial stage shift, diagnosing cancers at earlier, more treatable stages. Over 10 years, supplemental MCED testing is projected to yield a 45% decrease in Stage IV diagnoses [73]. The largest absolute reductions in late-stage diagnoses were seen for lung, colorectal, and pancreatic cancers [73]. This indicates MCED tests could address a critical gap in screening for cancers that currently lack recommended tests.
Troubleshooting Guides
Issue 1: Interpreting a Positive MCED Test Result
Problem: A researcher or clinician receives a "Cancer Signal Detected" result from an MCED test and needs to determine the appropriate next steps, mindful of the potential for a false positive.
Solution: Follow a validated diagnostic workflow to confirm the result.
- Consult the Cancer Signal Origin (CSO): The MCED test predicts the tissue or organ associated with the cancer signal. A CSO accuracy of 87% to 93.4% provides a starting point for a targeted workup [71] [70].
- Initiate Diagnostic Imaging: Begin with advanced imaging based on the CSO. In clinical studies, fluorine-18 fluorodeoxyglucose positron emission tomography–computed tomography (18-F-FDG PET/CT) has been used effectively [72].
- Confirm with Standard Diagnostics: Use established methods (e.g., biopsy, further imaging) to confirm or rule out cancer. In a real-world cohort, the median time from MCED result to diagnosis was 39.5 days [71].
- Resolution: If no cancer is found after comprehensive evaluation, the result is considered a false positive. Longitudinal data shows a low subsequent cancer risk, providing reassurance for clinical management [72].
Issue 2: High False Positive Burden in a Screening Study
Problem: A research protocol using multiple single-cancer screening tests is generating a high cumulative false positive rate, leading to patient anxiety, unnecessary procedures, and poor resource allocation.
Solution: Evaluate the integration of a high-specificity MCED test.
- Quantify the Cumulative Burden: Calculate the combined false positive rate of all single-cancer tests in your protocol. For reference, the lifetime risk of at least one false positive is high, especially for groups screened more frequently [69].
- Benchmark Against MCED Metrics: Compare your protocol's rate to the 0.4% false positive rate (99.6% specificity) of a leading MCED test [70].
- Assess Protocol Efficiency: Model whether layering one MCED test could maintain broad cancer coverage while reducing the overall false positive burden, as MCED tests are designed to minimize false positives when used for multiple cancers [71].
- Implement and Monitor: Integrate the MCED test into the study protocol and track key performance indicators, including the overall positivity rate, PPV, and the number of unnecessary invasive procedures avoided.
Table 1: Comparative Performance Metrics of Screening Tests
| Performance Measure | Single-Cancer Screening Tests (Examples) | Multi-Cancer Early Detection (MCED) Test |
|---|---|---|
| False Positive Rate | Mammogram: ~4.9% per test [69]Lifetime Risk (Women): 85.5% [69] | ~0.4% (Specificity 99.6%) [70] |
| Positive Predictive Value (PPV) | Mammography: 4.4% - 28.6% [71]FIT: 7.0% [71]Low-dose CT (Lung): 3.5% - 11% [71] | 61.6% (Galleri) [70]Real-world ePPV (asymptomatic): 49.4% [71] |
| Cancer Signal Origin Accuracy | Not applicable (single-organ test) | 87% - 93.4% [71] [70] |
| Sensitivity (All Cancer Types) | Varies by test and cancer type. | 51.5% (across all stages) [70] |
Table 2: Projected Impact of Supplemental Annual MCED Testing on Stage Shift over 10 Years [73]
| Cancer Stage | Change in Diagnoses (Relative to Standard of Care Alone) |
|---|---|
| Stage I | 10% increase |
| Stage II | 20% increase |
| Stage III | 34% increase |
| Stage IV | 45% decrease |
Experimental Protocols
Protocol 1: Microsimulation Modeling for Long-Term MCED Impact Assessment
This methodology is used to predict the long-term population-level impact of MCED testing before decades of real-world data are available [73].
- Model Development (SiMCED): Develop a continuous-time, discrete-event microsimulation model (e.g., SiMCED) incorporating 14+ solid tumor cancer types that account for a majority of cancer incidence and mortality.
- Cohort Generation: Simulate a large cohort (e.g., 5 million individuals) matching the demographic composition (age, sex, race) of the target population.
- Parameter Calibration: Calibrate the model using epidemiological data from sources like the Surveillance, Epidemiology, and End Results (SEER) database. Input key parameters:
- Natural History: Cancer-specific dwell times in each stage (I-IV).
- SoC Diagnosis: Rates of diagnosis via current screening, symptoms, or incidental findings.
- MCED Test Performance: Incorporate cancer type- and stage-specific sensitivities and specificities from clinical studies.
- Simulation: Run the model to compare two scenarios over a long-term horizon (e.g., 10 years): (A) Standard of care alone, and (B) Standard of care plus annual MCED testing.
- Outcome Analysis: The primary outcome is typically stage shift—the change in the distribution of cancer stages at diagnosis. Secondary outcomes can include reductions in late-stage incidence for specific cancers [73].
Protocol 2: Prospective Interventional Trial for MCED Test Performance and Outcomes
This protocol, based on studies like DETECT-A and PATHFINDER, evaluates MCED test performance and diagnostic workflows in a clinical setting [72] [71] [70].
- Participant Recruitment: Enroll a large cohort (e.g., >10,000) of asymptomatic adults at elevated risk for cancer (e.g., aged 50+), with no prior cancer history.
- Blood Draw and MCED Testing: Collect a peripheral blood sample from each participant and analyze it using the MCED test.
- Result Management and Diagnostic Workup:
- "No Cancer Signal Detected": Continue routine follow-up.
- "Cancer Signal Detected": Provide the Cancer Signal Origin (CSO) prediction to the investigator.
- Initiate a predefined diagnostic workflow starting with imaging (e.g., 18-F-FDG PET/CT) guided by the CSO.
- Perform all necessary follow-up procedures (e.g., additional imaging, biopsy) to confirm or rule out cancer.
- Data Collection: Document all diagnostic procedures, final diagnoses (cancer type and stage), treatments, and clinical outcomes.
- Outcome Measures:
- Cancer Signal Detection Rate: Proportion of tests positive.
- False Positive Rate & Specificity: Proportion of positive tests without cancer.
- Positive Predictive Value (PPV): Proportion of positive tests that correctly identify cancer.
- CSO Accuracy: Proportion of correct tissue of origin predictions.
- Time to Diagnosis: Interval from positive test to confirmed diagnosis.
Diagnostic Workflow Diagram
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials for MCED Test Development and Evaluation
| Item | Function / Application in MCED Research |
|---|---|
| Cell-free DNA (cfDNA) Collection Tubes | Stabilizes blood samples to prevent genomic DNA contamination and preserve cfDNA fragments for analysis from peripheral blood draws [71]. |
| Targeted Methylation Sequencing Panels | Enriches and sequences specific methylated regions of cfDNA; the core technology for detecting and classifying cancer signals in many MCED tests [71]. |
| Machine Learning Algorithms | Analyzes complex methylation patterns to classify samples as "cancer" or "non-cancer" and predict the Cancer Signal Origin (CSO) [71]. |
| FDG-PET/CT Imaging | Serves as a primary tool in the diagnostic workflow to localize and investigate a positive MCED test result, guided by the CSO prediction [72]. |
| Reference Standards & Controls | Validated samples with known cancer status (positive and negative) essential for calibrating assays, determining sensitivity/specificity, and ensuring laboratory quality [70]. |
| Microsimulation Models (e.g., SiMCED) | Software platforms used to model the natural history of cancer and project the long-term population-level impact (e.g., stage shift) of implementing MCED testing [73]. |
Hierarchical Bayesian Models for Test Performance Estimation in Multi-Center Studies
Frequently Asked Questions (FAQs)
Core Concepts and Applications
Q1: What is the primary advantage of using a Hierarchical Bayesian Model for estimating test performance in multi-center studies?
Hierarchical Bayesian Models (HBMs) are particularly powerful for multi-center studies because they account for between-center heterogeneity while allowing for the partial pooling of information across different sites. This means that instead of treating each center's data as entirely separate or forcing them to be identical, the model recognizes that each center has its own unique performance characteristics (e.g., due to local patient populations or operational procedures) but that these characteristics are drawn from a common, overarching distribution. This leads to more robust and generalizable estimates of test performance, especially when some centers have limited data, as information from larger centers helps to inform estimates for smaller ones [74] [75].
Q2: How can HBMs help address the challenge of false positives in screening data research?
HBMs provide a structured framework to understand and quantify the factors that contribute to false positives. By modeling the data hierarchically, researchers can:
- Incorporate Covariates: Identify patient-level or center-level factors (e.g., breast density, radiologist experience) that influence the probability of a false-positive result [76].
- Estimate Accurately in Absence of Gold Standard: Use latent class models to estimate test sensitivity and specificity even when a perfect reference test is not available for all subjects, thus correcting for partial verification bias and providing a more realistic assessment of test performance [75] [77].
- Quantify Uncertainty: Provide full posterior distributions for all parameters, which allows researchers to quantify the uncertainty around false-positive rates and other performance metrics, leading to more informed decision-making [78] [79].
Q3: Can HBMs integrate data from different study designs, such as both cohort and case-control studies?
Yes, a key strength of advanced HBMs is their ability to integrate data from different study designs. A hybrid Bayesian hierarchical model can be developed to combine cohort studies (which provide estimates of disease prevalence, sensitivity, and specificity) with case-control studies (which only provide data on sensitivity and specificity). This approach maximizes the use of all available evidence, improving the precision of the overall meta-analysis and providing a more comprehensive evaluation of a diagnostic test's performance [75].
Implementation and Methodology
Q4: What is a typical model specification for assessing accrual performance in clinical trials using an HBM?
A Bayesian hierarchical model can be used to evaluate performance metrics like trial accrual rates. The following specification models the number of patients accrued in a trial as a Poisson process, with performance varying across studies according to a higher-level distribution [78]:
- Data Level: The observed number of patients accrued ((mi)) in trial (i) over a specific period is modeled as: (mi \sim \text{Poisson}(\lambdai)), where (\lambdai = Pi \times n{\text{adj}, i}). Here, (Pi) is the unknown accrual performance parameter for trial (i), and (n{\text{adj}, i}) is the adjusted target accrual given the observation time.
- Process Level: The log of the individual performance parameters is modeled as varying around a yearly mean: (\log(Pi) \sim N(\log(\mu{j[i]}), \sigma^2)). Here, (\mu_{j[i]}) is the mean accrual performance across all trials in the year (j) that trial (i) belongs to.
- Prior Level: Non-informative or weakly informative priors are placed on the hyper-parameters: (\log(\mu_j) \sim N(0, 1000)) (1/\sigma^2 \sim \text{Uniform}(0, 10))
The primary parameter for inference is (\mu_j), which represents the annual accrual performance across all trials [78].
Q5: How is an HBM constructed for diagnostic test meta-analysis without a perfect gold standard?
A hierarchical Bayesian latent class model is used for this purpose. It treats the true disease status as an unobserved (latent) variable and simultaneously estimates the prevalence of the disease and the performance of the tests [80] [77].
The following workflow outlines the key stages in implementing such a model.
The model specifies the likelihood of the observed test results conditional on the latent true disease status. The sensitivities and specificities of the tests from each study are assumed to be random effects drawn from common population distributions (e.g., a Beta distribution), which is the hierarchical component that allows for borrowing of strength across studies [77].
Model Selection and Validation
Q6: How do I choose between a conditional independence and a conditional dependence HBM for diagnostic tests?
The choice hinges on whether you believe the tests' results are correlated beyond their shared dependence on the true disease status.
- Conditional Independence Model: Assume that once the true disease status is known, the results of the different tests are independent. This is a simpler model and a good starting point. A Bayesian hierarchical conditional independence latent class model is applicable to both with-gold-standard and without-gold-standard situations [80].
- Conditional Dependence Model: If it is known or suspected that the tests share common technological principles or are interpreted by the same personnel, their errors might be correlated. In this case, the model should be extended to include covariance terms between tests to account for this dependence. Model fit statistics, such as posterior predictive checks or Deviance Information Criterion (DIC), and correlation residual analysis can help determine if the more complex dependent model is warranted [80].
Q7: What are the key steps for validating and ensuring the robustness of an HBM?
Robustness and validation are critical. Key steps include:
- Sensitivity Analysis: Run the model with different prior distributions (e.g., more non-informative priors) to ensure that the posterior inferences are not overly sensitive to prior choice [78].
- Posterior Predictive Checks: Simulate new data from the fitted model and compare it to the observed data. Good agreement suggests the model adequately captures the data-generating process.
- Convergence Diagnostics: When using Markov Chain Monte Carlo (MCMC) sampling, use tools like trace plots and the Gelman-Rubin statistic ((\hat{R})) to ensure the chains have converged to the target posterior distribution. Software like JAGS or Stan is commonly used for this [80] [75].
Troubleshooting Guide
Computational and Data Issues
| Problem Symptom | Possible Cause | Solution Steps |
|---|---|---|
| Model fails to converge during MCMC sampling. | Poorly specified priors, overly complex model structure, or insufficient data. | 1. Simplify the model: Start with a simpler model (e.g., conditional independence) and gradually add complexity.2. Use stronger priors: Incorporate domain knowledge through weakly informative priors to stabilize estimation [78].3. Check for identifiability: Ensure the model parameters are identifiable, especially in latent class models without a gold standard. |
| Estimates for false-positive rates are imprecise (wide credible intervals). | High heterogeneity between centers or a low number of events (false positives) in the data. | 1. Investigate covariates: Include center-level (e.g., volume) or patient-level (e.g., age, breast density) covariates to explain some of the heterogeneity [76].2. Consider a different link function: The default logit link might not be optimal; explore others like the probit link.3. Acknowledge limitation: The data may simply be too sparse to provide precise estimates; report the uncertainty transparently. |
| Handling missing data for the reference standard (partial verification bias). | The missingness mechanism is often related to the index test result, violating the missing completely at random (MCAR) assumption. | Implement a Bayesian model that explicitly accounts for the verification process. Model the probability of being verified by the reference standard as depending on the index test result (Missing at Random assumption), and jointly model the disease and verification processes to obtain unbiased estimates of sensitivity and specificity [75]. |
Interpretation and Reporting
| Problem Symptom | Possible Cause | Solution Steps |
|---|---|---|
| Counterintuitive results, such as a test's sensitivity being lower than expected based on individual study results. | The hierarchical model is shrinking extreme estimates from individual centers (with high uncertainty) toward the overall mean. | This is often a feature, not a bug. Shrinkage provides more reliable estimates for centers with small sample sizes by borrowing strength from the entire dataset. Interpret the pooled estimate as a more generalizable measure of performance. |
| Difficulty communicating HBM results to non-statistical stakeholders. | The output (posterior distributions) is inherently probabilistic and more complex than a simple p-value. | 1. Visualize results: Use forest plots to show center-specific estimates and how they are shrunk toward the mean.2. Report meaningful summaries: Present posterior medians along with 95% credible intervals (CrIs) to convey the estimate and its uncertainty [78] [77].3. Use probability statements: For example, "There is a 95% probability that the true sensitivity lies between X and Y." |
Key Research Reagent Solutions
The following table details essential methodological components for implementing Hierarchical Bayesian Models in this field.
| Item/Concept | Function in the Experimental Process | Key Specification / Notes |
|---|---|---|
| Bayesian Hierarchical Latent Class Model | Estimates test sensitivity & specificity in the absence of a perfect gold standard. | Allows for between-study heterogeneity; essential for synthesizing data from multiple centers where reference standards may vary [80] [77]. |
| Hybrid GLMM | Combines data from both cohort and case-control studies in a single meta-analysis. | Prevents loss of information; corrects for partial verification bias by modeling the verification process [75]. |
| MCMC Sampling Software (e.g., JAGS, Stan) | Performs Bayesian inference and samples from the complex posterior distributions of hierarchical models. | JAGS is efficiently adopted for implementing these models; critical for practical computation [80] [75]. |
| Posterior Probability | Used for making probabilistic inferences and comparing performance across time periods or groups. | e.g., "The posterior probability that annual accrual performance is better with a new database (C3OD) was 0.935" [78]. |
| Bivariate Random Effects Model | A standard HBM for meta-analyzing paired sensitivity and specificity, accounting for their inherent correlation. | Recommended by the Cochrane Diagnostic Methods Group; a foundational model in the field [75]. |
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: What does it mean when a gold standard is "imperfect," and why is this a problem for my research?
An imperfect gold standard is a reference test that is considered definitive for a particular disease or condition but falls short of 100% accuracy in practice [81]. Relying on such a standard without understanding its limitations can lead to the erroneous classification of patients (e.g., false positives or false negatives), which ultimately affects treatment decisions, patient outcomes, and the validity of your research findings [81]. For example, colposcopy-directed biopsy for cervical neoplasia has a sensitivity of only 60%, making it far from a definitive test [81].
Q2: What are the common sources of bias when using an imperfect reference standard?
Several biases can compromise your reference standard [81]:
- Selection Bias: Occurs when the reference standard is only applicable to a subgroup of the target population. For instance, an invasive test with associated risks is more likely to be performed on high-suspicion patients, and its performance may not be generalizable to the entire population [81].
- Poorly Defined Criteria: Vaguely defined diagnostic criteria can lead to variability in how patients are classified, resulting in poor reproducibility and precision [81].
- Unclear Rationale for Treatment: If the reasons for treatment decisions are not documented, it becomes difficult to validate the reference standard against clinical outcomes [81].
Q3: My screening assay is producing a high rate of false positives. What is a systematic approach to troubleshoot this?
A high false-positive rate often indicates an issue with diagnostic specificity. A structured troubleshooting protocol is outlined below. Begin by verifying reagent integrity and protocol adherence, then systematically investigate biological and technical interferents. A definitive confirmation with an alternative method is crucial to identify the root cause, such as antibody cross-reactivity in serological assays [82].
Q4: What is a composite reference standard, and when should I use it?
A composite reference standard combines multiple tests or sources of information to arrive at a diagnostic outcome. It is used when a single "true" gold standard does not exist or has low disease detection sensitivity [81]. The multiple tests can be organized hierarchically to avoid redundant testing. This approach is advantageous for complex diseases with multiple diagnostic criteria, as it typically results in higher sensitivity and specificity than any single test used alone [81].
Q5: How can I validate a new reference standard I am developing for my research?
Validation is a comprehensive process to ensure your reference standard is accurate and fit for purpose. It involves two key strategies [81]:
- Internal Validation: Performed on a single dataset to determine accuracy within your target population. This involves comparing the new standard against the current best available standard and ensuring it is clinically credible and feasible [81].
- External Validation: Assesses the generalizability and reproducibility of the reference standard in different target populations. This demonstrates that the standard is precise and reliable beyond your initial study group [81].
Troubleshooting Guides
Problem: High Rate of False Positives in a Serological Assay
Background: This issue is common in immunoassays, such as ELISA, where antibody cross-reactivity can occur. A documented case involved a surge in false-positive HIV test results following a wave of SARS-CoV-2 infections, attributed to structural similarities between the viruses' proteins [82].
Investigation and Solution Protocol:
Confirm the Result:
- Action: All initially reactive specimens should be tested in duplicate. Specimens that remain reactive must be confirmed with a definitive method, such as a Western blot or PCR, at an expert referral laboratory [82].
- Documentation: Classify specimens confirmed negative by the definitive test as false positives.
Correlate with Clinical and Epidemiological Data:
- Action: Analyze the temporal trend of false-positive rates. Correlate this data with population-level data on other infections or vaccinations. Statistical methods like Pearson correlation analysis can be used to quantify the relationship [82].
- Example: In the HIV false-positive case, a significant positive correlation (r=0.927, p<0.01) was found between the HIV false-positive rate and the prevalence of SARS-CoV-2 antibodies in the donor population [82].
Implement a Mitigation Strategy:
- Action: Based on the root cause, adjust your diagnostic algorithm.
- Solution: Adopt a multi-step diagnostic process. Use the initial screening assay (e.g., fourth-generation ELISA) as a sensitive first pass. All positive results must then be routed through a confirmatory assay that relies on a different principle (e.g., nucleic acid test or a different immunoassay) before a final diagnosis is assigned [82].
- Benefit: This sequential testing strategy preserves the sensitivity of screening while drastically improving specificity, thus mitigating the impact of cross-reactivity.
Problem: Mitigating Model Misconduct in Distributed Machine Learning
Background: In Federated or Distributed Federated Learning (DFL) on electronic health record data, a critical vulnerability is "model misconduct" or "poisoning," where a participating site injects a tampered local model into the collaborative pipeline. This can degrade the global model's performance and introduce false patterns[f].
Investigation and Solution Protocol:
Detect Potential Misconduct:
- Action: Implement a detection heuristic to flag local models that deviate significantly from the consensus or expected behavior. This detection should be transparent and recorded on a tamper-proof ledger like a blockchain for auditability[f].
Implement a False-Positive Tolerant Mitigation:
- Action: Instead of immediately quarantining a site after a single flag, assign each participant a "misbehavior budget." Each potential misconduct incident incurs a budget penalty (a hyperparameter, e.g., γ=0.15). A site is only quarantined when its budget is exhausted[f].
- Benefit: This budget-based system prevents the over-ostracization of benign sites due to occasional false alarms, preserving the collaborative sample size and maintaining the model's performance. Research has shown this method results in statistically significant gains in model performance (AUC) compared to non-tolerant approaches[f].
Key Experimental Protocols & Data Presentation
Protocol: Developing and Validating a Composite Reference Standard
This methodology is adapted from the development of a new reference standard for vasospasm [81].
- Objective: To create a reference standard applicable to an entire patient population by incorporating multiple levels of diagnostic evidence.
- Materials: Patient data, including clinical exam notes, imaging reports (DSA, CT, MRI), and treatment records.
- Hierarchical Methodology:
- Primary Level (Strongest Evidence): Use the current best available invasive or definitive test (e.g., DSA for vasospasm) to determine the presence or absence of the condition. Apply to patients who have undergone this test.
- Secondary Level (Sequela of Condition): For patients not undergoing the primary test, evaluate for sequelae using both:
- Clinical Criteria: Evidence of permanent neurological deficits distinct from baseline.
- Imaging Criteria: Evidence of delayed infarction on CT or MRI.
- A diagnosis is assigned if either criterion is met. If not, and the patient was not treated, a "no condition" diagnosis is assigned.
- Tertiary Level (Response-to-Treatment): For treated patients without primary or secondary evidence, assign a diagnosis based on their response to appropriate therapy. Patients showing improvement are classified as having the condition; those without improvement and with an alternative etiology are classified as not having it.
- Validation: Conduct a two-phase internal validation [81]:
- Phase I: Compare the secondary/tertiary level outcomes with the primary level (current gold standard) in the subgroup of patients who had both.
- Phase II: Apply the new composite standard to the entire target population and compare its feasibility and outcomes with the historical "chart diagnosis."
Summary of Validation Approaches for Imperfect Standards
| Strategy | Core Principle | Best Use Case | Key Advantage |
|---|---|---|---|
| Composite Reference Standard [81] | Combines multiple tests (imaging, clinical, outcome) into a single hierarchical diagnosis. | Complex diseases with multiple diagnostic criteria; no single perfect test exists. | Higher aggregate sensitivity and specificity than any single component test. |
| False-Positive Tolerant Mitigation [83] | Uses a "budget" to quarantine participants only after repeated model misconduct flags. | Distributed machine learning (e.g., Federated Learning) to maintain collaboration. | Prevents over-ostracization, preserves sample size, and recovers model performance (AUC). |
| Multi-Step Diagnostic Algorithm [82] | Employs a sensitive screening test followed by a specific confirmatory test. | Serological assays prone to cross-reactivity; high-throughput screening scenarios. | Dramatically reduces false positives while maintaining high sensitivity for true positives. |
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function/Benefit | Example Application |
|---|---|---|
| Multiple Generation Assays | Using different generations (e.g., 3rd vs. 4th Gen ELISA) can help identify interferents, as they may have different vulnerabilities to cross-reactivity [82]. | Investigating a spike in false positives by comparing results across assay generations [82]. |
| Confirmatory Test (Western Blot, PCR) | Provides a definitive result based on a different biological principle than the screening assay, used to confirm or rule out initial positive findings [82]. | Verifying the true disease status of samples that tested positive in a screening immunoassay [82]. |
| Statistical Correlation Software | Analyzes temporal trends and quantifies the strength of association between an interferent (e.g., SARS-CoV-2 antibodies) and the rate of false positives [82]. | Establishing a statistically significant link (e.g., r=0.927, p<0.01) between an interferent and assay performance [82]. |
| Blockchain Network | A decentralized ledger for recording model updates in distributed learning, providing transparency, traceability, and tamper-proof records to discourage and detect misconduct [83]. | Creating a secure, auditable record of all local model submissions in a Federated Learning environment [83]. |
| Misconduct Detection Heuristic | An algorithm designed to flag local models in a collaborative learning system that deviate significantly from the norm, indicating potential tampering or poisoning [83]. | The first step in a budget-based mitigation system to identify potentially malicious model updates [83]. |
Conclusion
Effectively managing false positives is not merely a technical exercise but a strategic imperative that enhances the entire drug development lifecycle. The key takeaways underscore that foundational data quality, coupled with the adoption of modern statistical methods like MMRM over outdated practices such as LOCF, is critical for data integrity. Methodologically, technologies like entity resolution and AI offer a path to greater precision, while operational optimization through system tuning and intelligent triage ensures resource efficiency. Finally, robust validation frameworks allow for the informed selection of superior screening strategies, as evidenced by the stark efficiency gains of multi-cancer early detection tests over multiple single-cancer tests. The future direction points toward greater integration of AI and machine learning, the establishment of industry-wide benchmarks for acceptable false-positive rates, and the development of even more sophisticated, explainable models to further reduce noise and amplify true signal in biomedical research.
References
- 1. False positives and false negatives [https://en.wikipedia.org/wiki/False_positives_and_false_negatives]
- 2. Practices of Science: False Positives and False Negatives [https://manoa.hawaii.edu/exploringourfluidearth/chemical/matter/properties-matter/practices-science-false-positives-and-false-negatives]
- 3. False Positives and False Negatives [https://www.geeksforgeeks.org/machine-learning/false-positives-and-false-negatives/]
- 4. The Burden of the “False‐Negatives” in Clinical Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC6402187/]
- 5. Classification: Accuracy, recall, precision, and related metrics [https://developers.google.com/machine-learning/crash-course/classification/accuracy-precision-recall]
- 6. Likelihood of False-Positive Results in High-Impact ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3294657/]
- 7. False-positive psychology [https://www.bitss.org/education/mooc-parent-page/week-2-publication-bias/is-there-a-credibility-crisis/false-positive-psychology-2/]
- 8. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 9. Boosting Accuracy and Efficiency: Assay Development ... [https://dispendix.com/blog/boosting-accuracy-and-efficiency-assay-development-and-validation-process-for-drug-discovery]
- 10. Considerations for Clinical Trial Design to More Effectively ... [https://www.aptitudehealth.com/oncology-news/phase-iii-oncology-trial-designs-false-positives/]
- 11. How to Minimize False Positives in ADP Detection [https://bellbrooklabs.com/how-to-minimize-false-positives-in-adp-detection/?srsltid=AfmBOoosVLE5oXawtELMWcKgwnPYbr_Yrj3JpydTgtGvYDQkyqdpX4U6]
- 12. Overcoming a false-positive mechanism in RapidFire MRM ... [https://www.sciencedirect.com/science/article/pii/S2472555225000450]
- 13. 6 Root Cause Analysis Tools & How To Use Them [https://www.amper.co/post/6-root-cause-analysis-tools-how-to-use-them]
- 14. Questions and Answers on Current Good Manufacturing ... [https://www.fda.gov/drugs/guidances-drugs/questions-and-answers-current-good-manufacturing-practice-regulations-production-and-process]
- 15. The impact of missing data and how it is handled on ... [https://pubmed.ncbi.nlm.nih.gov/17853425/]
- 16. Methodologies for Missing Data in Clinical Trials [https://www.quanticate.com/blog/missing-data-in-clinical-trials]
- 17. [PDF] The impact of missing data and how it is handled on ... [https://www.semanticscholar.org/paper/The-impact-of-missing-data-and-how-it-is-handled-on-Barnes-Mallinckrodt/f506faf983c31cbdf8aea2b8e942e12bd5920521]
- 18. Comparison of different approaches in handling missing data ... [https://hqlo.biomedcentral.com/articles/10.1186/s12955-025-02364-0]
- 19. Strategies for Dealing with Missing Data in Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC3767219/]
- 20. The Eradication of False Signals in Monitoring [https://www.appliedclinicaltrialsonline.com/view/the-eradication-of-false-signals-in-monitoring]
- 21. Reporting of missing data and methods used to ... [https://www.sciencedirect.com/science/article/abs/pii/S0304395914003078]
- 22. 2025 Clinical Data Trend Report [https://www.veeva.com/2025-clinical-data-trend-report/]
- 23. PD-L1 interaction false positive monitoring [https://www.bmglabtech.com/en/application-notes/identification-of-false-positives-in-a-htrf-screen-for-small-molecule-inhibitors-of-pd-1-pd-l1/]
- 24. Help for package mmrm [https://cran.r-project.org/web/packages/mmrm/refman/mmrm.html]
- 25. Mixed Models for Repeated Measures Should Include ... [https://pubmed.ncbi.nlm.nih.gov/34674187/]
- 26. What difference does multiple imputation make in ... [https://pubmed.ncbi.nlm.nih.gov/34797507/]
- 27. Multiple Imputation: A Flexible Tool for Handling Missing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4638176/]
- 28. Missing Data in Clinical Research: A Tutorial on Multiple ... [https://www.sciencedirect.com/science/article/pii/S0828282X20311119]
- 29. Controlling false positive rates in research and its clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4296621/]
- 30. Avoiding false positives and false negatives with power ... [https://www.statsig.com/perspectives/avoiding-false-positives-negatives]
- 31. Chapter7 Multiple Imputation models for Multilevel data [https://bookdown.org/mwheymans/bookmi/multiple-imputation-models-for-multilevel-data.html]
- 32. Trouble validating a Bayesian MMRM implemented with {brms} [https://discourse.mc-stan.org/t/trouble-validating-a-bayesian-mmrm-implemented-with-brms/33564]
- 33. Troubleshooting matching workflows - AWS Entity Resolution [https://docs.aws.amazon.com/entityresolution/latest/userguide/troubleshooting.html]
- 34. What is Entity Resolution: Techniques, Tools & Use Cases [https://www.puppygraph.com/blog/entity-resolution]
- 35. Entity Resolution Guide: Everything You Need To Know [https://winpure.com/entity-resolution-guide/]
- 36. Optimized Dual Threshold Entity Resolution For Electronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3900213/]
- 37. Data Matching Service – AWS Entity Resolution FAQs [https://aws.amazon.com/entity-resolution/faqs/]
- 38. Advanced Analytics: The Future of Clinical Decision Making [https://www.compunnel.com/blogs/advanced-analytics-in-clinical-decision-support/]
- 39. Common Errors - AWS Entity Resolution [https://docs.aws.amazon.com/entityresolution/latest/apireference/CommonErrors.html]
- 40. Urine Drug Screening: Minimizing False-Positives and ... [https://www.uspharmacist.com/article/urine-drug-screening-minimizing-false-positives-and-false-negatives-to-optimize-patient-care]
- 41. A Comprehensive Guide to Error Analysis in Machine ... [https://medium.com/mlearning-ai/a-comprehensive-guide-to-error-analysis-in-machine-learning-288e353f7c8d]
- 42. Replicate Testing of Clinical Endpoints Can Prevent No-Go ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10535203/]
- 43. AI and Machine Learning in Sanctions Screening [https://www.silenteight.com/blog/ai-and-machine-learning-in-sanctions-screening-where-ofac-draws-the-line]
- 44. Critical Mistakes Companies Make When Integrating AI/ML ... [https://towardsdatascience.com/critical-mistakes-companies-make-when-integrating-ai-ml-into-their-processes/]
- 45. AI Detection and assessment - an update for 2025 [https://nationalcentreforai.jiscinvolve.org/wp/2025/06/24/ai-detection-assessment-2025/]
- 46. 5 ways to reduce false positives in screening [https://www.napier.ai/post/reduce-false-positives-screening]
- 47. Top 10 Data Quality Best Practices to Improve Data ... [https://atlan.com/data-quality-best-practices/]
- 48. Data Quality: Best Practices for Accurate Insights [https://www.gartner.com/en/data-analytics/topics/data-quality]
- 49. Data Quality Measurement 2025 Trends and Proven ... [https://www.bitechnology.com/data-quality-measurement-2025-trends-and-proven-improvement-methodologies/]
- 50. 12 Data Quality Metrics to Measure Data Quality in 2025 [https://lakefs.io/data-quality/data-quality-metrics/]
- 51. The Imperative Role of Data Quality in Watchlist Screening [https://www.finscan.com/post/data-quality-in-watchlist-screening]
- 52. Data Quality Issues Affecting the Pharmaceutical Industry [https://firsteigen.com/blog/data-quality-issues-affecting-the-pharmaceutical-industry-finding-a-solution/]
- 53. Mammogram False Positives Affect Future Screening ... [https://www.cancer.gov/news-events/cancer-currents-blog/2024/mammogram-false-positives-affect-future-screening]
- 54. Estimating the Burden of False Positives and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11912434/]
- 55. AI supports lung cancer screening: false positives ... [https://www.radboudumc.nl/en/news-items/2025/ai-supports-lung-cancer-screening-false-positives-decrease-by-forty-percent]
- 56. Automated drug design for druggable target identification ... [https://www.nature.com/articles/s41598-025-18091-x]
- 57. What is Alert Triage in Cybersecurity? [https://corelight.com/resources/glossary/alert-triage]
- 58. Alert Triage: What It Is and How to Streamline It for Your SOC [https://www.vmray.com/alert-triage/]
- 59. What Is Risk Scoring? How To Score Risk [https://www.splunk.com/en_us/blog/learn/risk-scoring.html]
- 60. How to Minimize False Positives in AML Screening [https://www.flagright.com/post/how-to-minimize-false-positives-in-aml-screening]
- 61. Alert Triage in 2025 Guide [https://www.dropzone.ai/resource-guide/alert-triage-guide-2025]
- 62. Reduce False Positives & Enhance Entity Resolution [https://risk.lexisnexis.com/insights-resources/article/entity-resolution-redefining-false-positive-problem]
- 63. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 64. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 65. Understanding PPV and NPV in Healthcare Testing [https://harbinger-health.com/2024/09/26/understanding-ppv-and-npv-in-healthcare-testing-crucial-tools-for-diagnostic-accuracy/]
- 66. Positive and negative predictive values [https://en.wikipedia.org/wiki/Positive_and_negative_predictive_values]
- 67. The False Positive Paradox [https://medium.com/@gabrielcapela/the-false-positive-paradox-62e46b92a3a1]
- 68. 5 Paradoxes in Statistics Every Data Scientist Should be ... [https://towardsai.net/p/l/5-paradoxes-in-statistics-every-data-scientist-should-be-familiar-with]
- 69. Estimating the lifetime risk of a false positive screening test result [https://pmc.ncbi.nlm.nih.gov/articles/PMC9931091/]
- 70. Galleri Test Sensitivity & Specificity | Galleri® for HCPs [https://www.galleri.com/hcp/galleri-test-performance]
- 71. Real-world data and clinical experience from over ... [https://www.nature.com/articles/s41467-025-64094-7]
- 72. Outcomes Following a False-Positive Multi-Cancer Early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11292315/]
- 73. The impact of multicancer early detection tests on cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598375/]
- 74. Application of the hierarchical Bayesian models to analyze ... [https://www.sciencedirect.com/science/article/pii/S0892687525003140]
- 75. A Hybrid Bayesian Hierarchical Model Combining Cohort ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4245380/]
- 76. Factors associated with false-positive screening ... [https://www.nature.com/articles/s41598-025-86993-x]
- 77. Review A Hierarchical Bayesian Latent Class Model for the ... [https://www.sciencedirect.com/science/article/pii/S2274580724002681]
- 78. Using Bayesian hierarchical modeling for performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10900093/]
- 79. Bayesian Hierarchical Models for Quantitative Estimates ... [https://arxiv.org/abs/2505.13621]
- 80. Bayesian hierarchical latent class models for estimating ... [https://pubmed.ncbi.nlm.nih.gov/31146651/]
- 81. Developing a New Reference Standard… Is Validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2919497/]
- 82. Cross-reactivity mediated by SARS-CoV-2 antibodies: ... [https://www.sciencedirect.com/science/article/abs/pii/S0732889325004110]
- 83. False-positive tolerant model misconduct mitigation in ... [https://www.nature.com/articles/s41598-025-04069-2]